Children with cancer are at increased risk of potentially life-threatening Clostridioides difficile infections (CDI), and Brianna Murphy, DO, reported at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year.
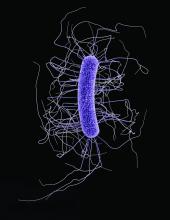
CDI are characterized by diarrhea, fever, and loss of appetite. The clinical features are caused by the release of toxins A and B by this gram-positive bacterium. In pediatric groups, CDI are a leading cause of antibiotic-associated gastric illness. This in turn can lead to a protracted stay in hospital and increases risk of mortality. The rising incidence in the United States over the last 2 decades prompted Dr. Murphy, a pediatric hematology oncology fellow working at the department of pediatric research at the University of Texas MD Anderson Cancer Center, Houston, to investigate further. A search of the literature found limited information regarding CDI and pediatric oncology patients.
Recognized factors for contracting CDI include the presence of other illnesses, a weakened immune system because of drugs or disease, enteral nutrition, usage of medicines such as proton pump inhibitors which decrease gastric acid production, and classically, treatment with broad spectrum antibiotics.
Dr. Murphy’s study included patients aged 1-18 years, all of whom had a cancer diagnosis and a positive stool culture for C. difficile. Presenting symptoms were three or more loose stools per day or acute onset ileus. The study evaluated data for the years 2000-2017 and included 11,366 children; 207 CDI (0.98%) cases were identified among pediatric oncology patients during the study period. This compares with historical data showing an incidence of 0.14% among hospitalized children in general.
Malignancy data were then subdivided into three groups: hematologic, nonneural solid tumors (NNST), and neural tumors. Hematologic malignancies had a CDI prevalence higher than the average for oncologic patients at 5.4%. Inside this group those suffering with acute myeloid leukemia had a rate of 10.5%. In the NNST and neural tumor groups, CDI rates were lower and closer to the overall average.
Dr. Murphy then looked at her patient population in more detail. Poor clinical outcomes (PCOs) were defined as severe, refractory, recurrent, or multiple infections. Severe CDI included features such as toxic megacolon, gastrointestinal perforation, or need for surgical intervention. Refractory CDI were defined as continuation of symptoms beyond 7 days of appropriate therapy, and recurrent CDI were classed as reinfection within 8 weeks of a previous CDI. Ultimately, 51% of patients in this study died. Patients with severe CDI experienced increased mortality (P = .02). There was no difference shown when looking at the type of cancer, age, gender, or patient ethnicity.
Next, Dr. Murphy looked for associations. Hematologic and biochemical testing identified that elevated creatinine was statistically associated with the likelihood of PCOs, compared with leukocytosis and neutropenia, particularly in the NNST group. Treatment modality also was studied. Here radiation therapy was the only treatment shown to increase PCOs in patients with CDI. One-fifth (22%) of radiation therapy recipients experienced multiple CDI, compared with 12% of the total population.
In commenting on her paper, Louis Bent, MD, from the Netherlands raised the issue of deaths in septic patients. What was the origin of the responsible organism, for example from the GI tract or from central lines, and were patients receiving appropriate antibiotic treatment?
Dr. Kelly responded that sepsis was generally believed to occur as a result of infection with mixed bacterial translocation through the bowel wall, notably Escherichia coli. Patients were usually on a cocktail of antibiotics targeting CDI, but also other infections illustrating the serious nature of the situation.
Dr. Murphy had no financial conflicts of interest to declare.