The need for improved recognition. Twice-exceptionality commonly manifests as children reach grade-school age, but they are underrepresented in programs for the gifted due to misunderstanding and misdiagnosis by professionals.15,16 Best practices in identifying 2E children incorporate multidimensional assessments including pre-referral and screening, preliminary intervention, evaluation procedures, and educational planning.16 Despite research asserting that 2E individuals need more support services, knowing how to best identify and support individuals across various settings can prove difficult.7,17-19
Primary care, as we will discuss in a bit, is an interdisciplinary setting in which identification and comprehensive and collaborative support can occur. Historically, though, mental and physical health care have been “siloed” and mental health professionals’ functions in medical settings have often been circumscribed.20,21
A lesson from how our case unfolded
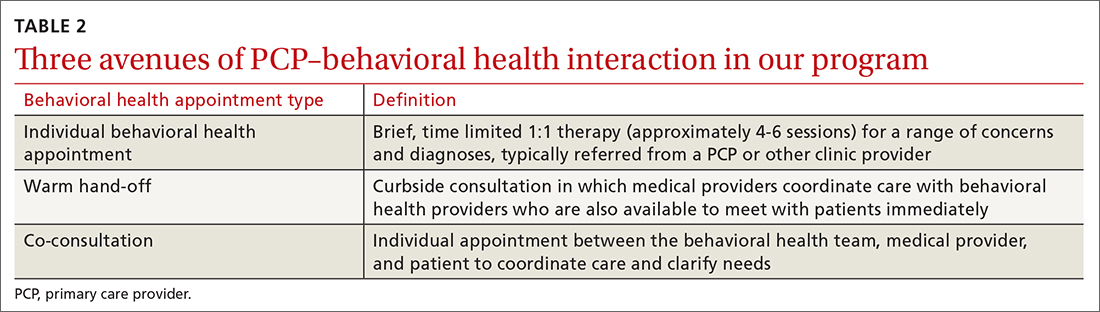
Our integrated health team, known as Integrated Behavioral Health Plus (IBH+), was developed at the University of Colorado School of Medicine, and is a system-level integration of behavioral health professionals working with medical providers to improve outcomes and satisfaction.22 Psychology supervisors and trainees, telepsychiatrists and psychiatry residents, social workers, and pharmacists work together with PCPs and residents to deliver comprehensive patient care. Our model includes a range of behavioral health access points for patients (TABLE 2) and the use of complex patient databases and care team meetings.
In the case we have described here, the nature of the patient’s presentation did not trigger any of the clinical procedures described in TABLE 2, and he fell under the radar of complex patient cases in the clinic. Instead, informal, asynchronous clinical conversations between providers were what eventually lead to diagnostic clarification. Team consultation and psychometric testing provided by IBH+ helped uncover the “hidden diagnosis” of this patient in primary care and identified him as twice-exceptional, experiencing both giftedness and significant emotional suffering (major depression and social anxiety, low self-esteem and self-worth).
Takeaways for primary care
Not all PCPs, of course, have immediate onsite access to a program such as ours. However, innovative ways to tap into available resources might include establishing a partnership with 1 or more behavioral health professionals or bridging less formal relationships with such providers in the community and schools to more easily share patient records.
Continue to: Other presentations within 2E populations