THE CASE
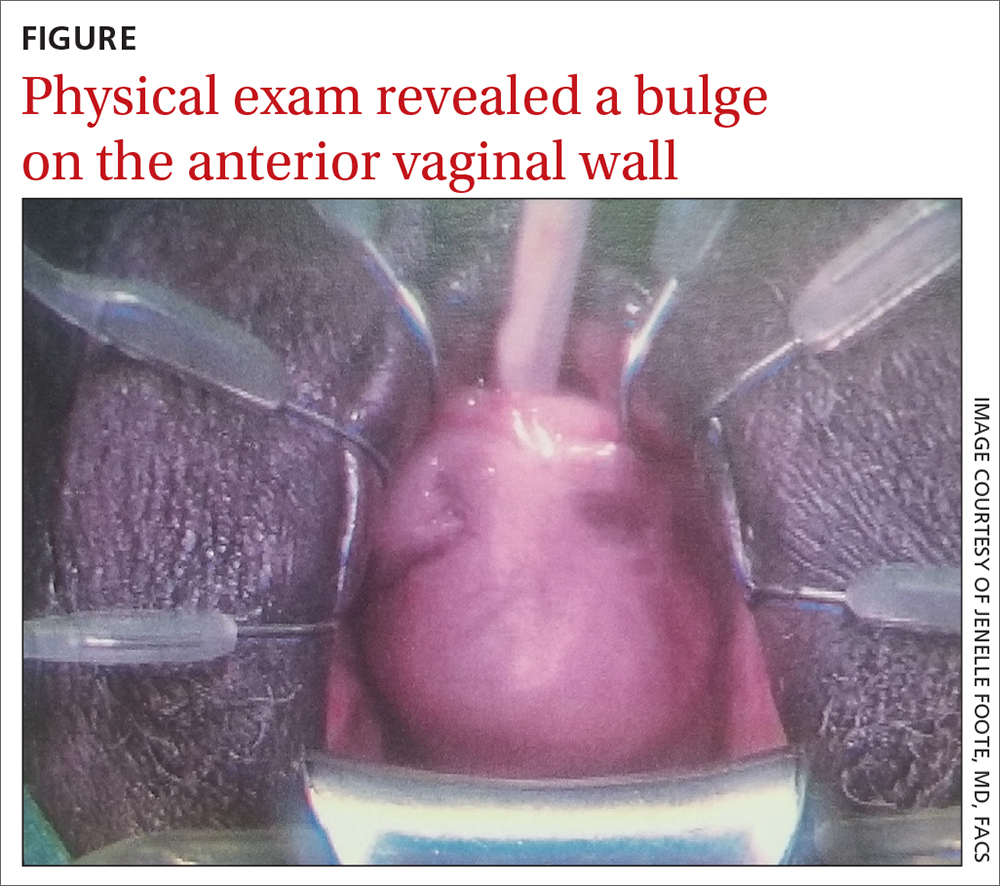
A 62-year-old postmenopausal woman presented to the clinic as a new patient for her annual physical examination. She reported a 9-year history of symptoms including dysuria, post-void dribbling, dyspareunia, and urinary incontinence on review of systems. Her physical examination revealed an anterior vaginal wall bulge (FIGURE). Results of a urinalysis were negative. The patient was referred to Urology for further evaluation.
THE DIAGNOSIS
A pelvic magnetic resonance imaging (MRI) scan revealed a large periurethral diverticulum with a horseshoe shape.
DISCUSSION
Urethral diverticulum is a permanent sac-like cavity projecting into the periurethral fascia arising from the posterior urethral lumen.1 It is a rare condition that affects fewer than 20 per 1 million women per year.2 Urethral diverticulum can range from 1 cm to 8 cm in diameter and is located in the mid or distal urethra.1,3
Women are more likely than men to develop urethral diverticulum, and it can manifest at any age, usually in the third through seventh decade.4,5 It was once thought to be more common in Black women, although the literature does not support this.6 Black women are 3 times more likely to be operated on than White women to treat urethral diverticula.7
Unknown origin. Most cases of urethral diverticulum are acquired; the etiology is uncertain.8,9 The assumption is that urethral diverticulum occurs as a result of repeated infection of the periurethral glands with subsequent obstruction, abscess formation, and chronic inflammation.1,2,4 Childbirth trauma, iatrogenic causes, and urethral instrumentation have also been implicated.3,4 In rare cases of congenital urethral diverticula, the diverticula are thought to be remnants of Gartner duct cysts, and yet, incidence in the pediatric population is low.8
Diagnosis is confirmed through physical exam and imaging
The urethral diverticulum manifests anteriorly and palpation of the anterior vaginal wall may reveal a painful mass.10 A split-speculum is used for careful inspection and palpation of the anterior vaginal wall.9 If the diverticulum is found to be firm on palpation, or there is bloody urethral drainage, malignancy (although rare) must be ruled out.4,5 Refer such patients to a urologist or urogynecologist.
Radiologic imaging (eg, ultrasound, voiding cystourethrography [VCUG], and MRI) is useful in detecting the size, location, and extent of the diverticulum, revealing the relationship to surrounding tissues, and providing insights for appropriate surgical management.3,4,9 Ultrasound, which is usually readily available, noninvasive, and less expensive, can be considered for initial screening of suspected urethral diverticulum.3,11 A postvoid MRI is recommended when a urethral diverticulum is highly suspected.11,12 The MRI, with or without endoluminal coil, is considered the gold standard; it is a favorable complement to the work-up and offers the most diagnostic value.3,4 According to a single-institution study, the MRI was 100% sensitive and specific in diagnosing urethral diverticulum.12 However, the limitation of the MRI lies in its cost and lack of availability in some countries.13
Continue to: Nonspecific symptoms may lead to misdiagnosis