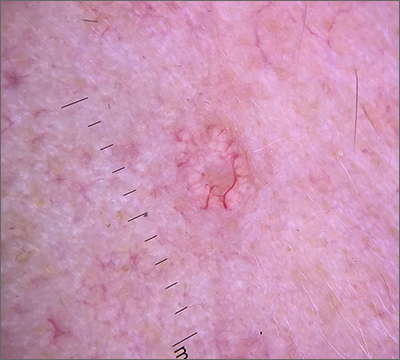
Dermoscopy revealed multiple small white structures around a central pore and tortuous, but not arborizing, blood vessels around the periphery (frequently called a crown pattern). These features pointed to the diagnosis of sebaceous gland hyperplasia (SGH).
SGH is a common benign condition seen predominantly in middle- to older-age people and patients on immunosuppressant drugs (especially ciclosporin). SGH tends to manifest as multiple lesions on the face and forehead, although the lesions can appear elsewhere.1
As the name implies, SGH is hyperplasia of the sebocytes of the hair follicle, which results in white-to-yellow clusters around the dilated opening of the follicle.1 In contrast to BCCs, which have arborizing blood vessels that can occur throughout the lesion, the vessels in SGH have a lower propensity for branching and tend to follow the periphery instead of crossing into the central pore.2 This characteristic pattern, as well as the appearance of multiple similar lesions elsewhere on a patient’s body, suggests a diagnosis of SGH. If the lesion is atypical, solitary, or has other features that make the diagnosis uncertain, a biopsy is recommended.
SGH is not malignant and is asymptomatic, so treatment is not required. However, the cosmetic appearance can be distressing or undesirable for some patients.1 The most common cosmetic remedies are destructive and include electrodessication, cryosurgery, and treatments with laser and intense pulsed light. Unfortunately, if there is residual tissue after treatment, recurrence is common, and due to the destructive nature of treatment, scarring is possible. It is important to counsel the patient regarding both of these possibilities and to balance the extent of destruction.
In patients with multiple lesions, oral isotretinoin may be used, but SGH will recur if treatment is discontinued. Additionally, isotretinoin, which is also used for cystic acne, is a high-risk medication due its potential to cause fetal anomalies and death if used during pregnancy. Patients usually get cheilitis and dyshidrosis due to its drying effect, but those symptoms are manageable with topical emollients.
This patient declined treatment, as he already had scars from previous NMSCs and was not concerned about the appearance of SGH.
Photo courtesy of Daniel Stulberg, MD. Text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.