Small-molecule drugs such as aspirin, albuterol, atorvastatin, and lisinopril are the backbone of disease management in family medicine.1 However, large-molecule biological drugs such as monoclonal antibodies (MAbs) are increasingly prescribed to treat common conditions. In the past decade, MAbs comprised 20% of all drug approvals by the US Food and Drug Administration (FDA), and today they represent more than half of drugs currently in development.2 Fifteen MAbs have been approved by the FDA over the past decade for asthma, atopic dermatitis (AD), hyperlipidemia, osteoporosis, and migraine prevention.3 This review details what makes MAbs unique and what you should know about them.
The uniqueness of monoclonal antibodies
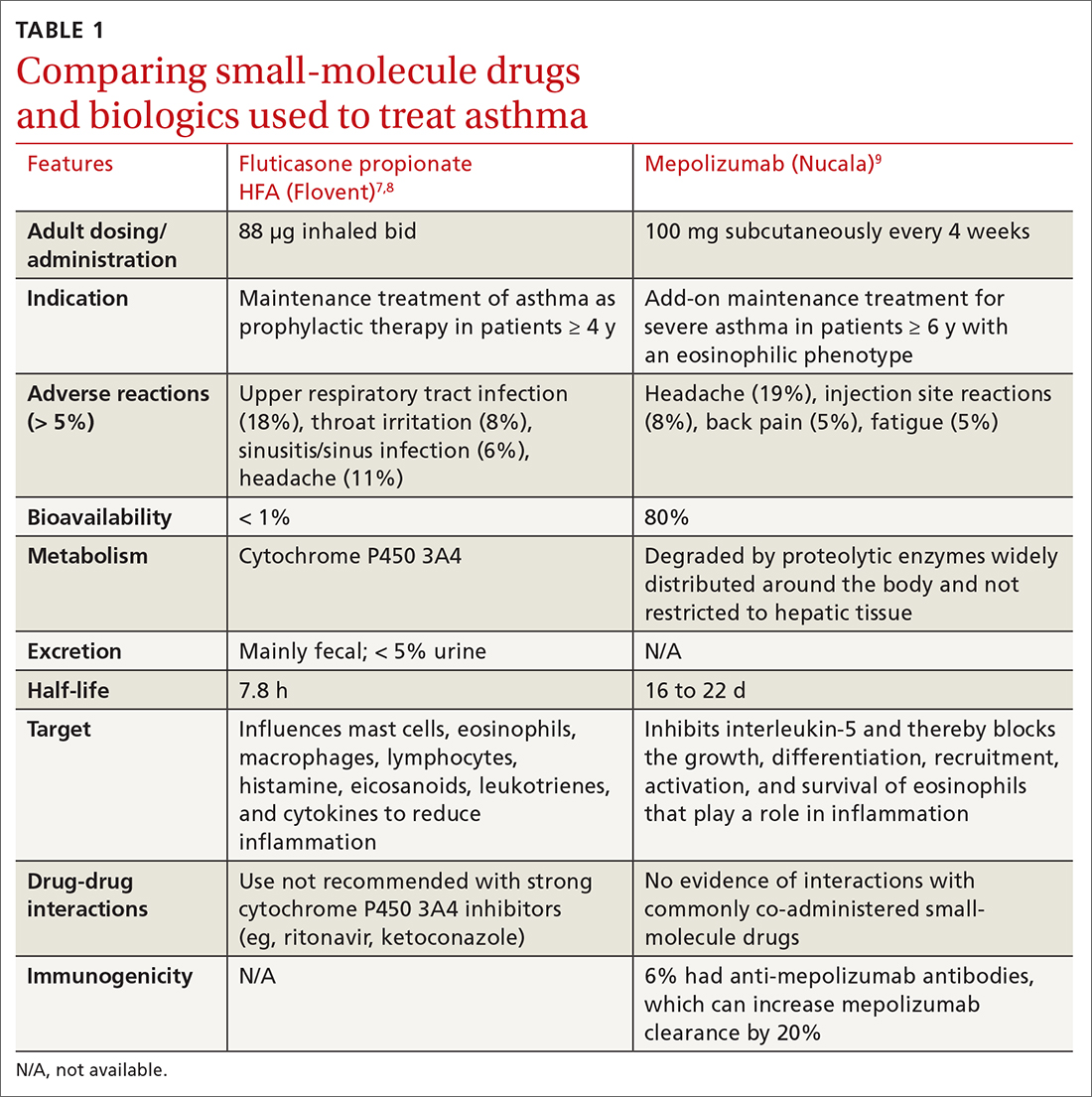
MAbs are biologics, but not all biologics are MAbs—eg, adalimumab (Humira) is a MAb, but etanercept (Enbrel) is not. MAbs are therapeutic proteins made possible by hybridoma technology used to create an antibody with single specificity.4-6 Monoclonal antibodies differ from small-molecule drugs in structure, dosing, route of administration, manufacturing, metabolism, drug interactions, and elimination (TABLE 17-9).
MAbs can be classified as naked, “without any drug or radioactive material attached to them,” or conjugated, “joined to a chemotherapy drug, radioactive isotope, or toxin.”10 MAbs work in several ways, including competitively inhibiting ligand-receptor binding, receptor blockade, or cell elimination from indirect immune system activities such as antibody-dependent cell-mediated cytotoxicity.11,12
Monoclonal antibody uses in family medicine
Asthma
Several MAbs have been approved for use in severe asthma, including but not limited to: omalizumab (Xolair),13 mepolizumab (Nucala),9,14 and dupilumab (Dupixent).15All 3 agents can be self-administered subcutaneously (SC), depending on the clinician’s assessment. The Global Initiative for Asthma (GINA) guidelines recommend that, prior to considering MAb therapy for a patient who has asthma, clinicians should assess the patient’s inhaler technique and adherence, treat comorbidities such as gastroesophageal reflux disease, and modify triggering factors such as smoking or allergen exposure.16 In patients with severe asthma still uncontrolled after receiving high-dose inhaled corticosteroids (ICSs) or the lowest possible dose of oral corticosteroid (OCS), GINA recommends assessing for type 2 airway inflammation: blood eosinophils ≥ 150/μL, sputum eosinophils ≥ 2%, or evidence of allergen stimulation.16 If these factors are present, consider prescribing anti-immunoglobulin E (anti-IgE) (omalizumab), anti-interleukin-5 (anti-IL-5) (mepolizumab), or anti-IL-4/anti-IL-13 (dupilumab).16
Omalizumab is a humanized MAb that prevents IgE antibodies from binding to mast cells and basophils, thereby reducing inflammatory mediators.13 A systematic review found that, compared with placebo, omalizumab used in patients with inadequately controlled moderate-to-severe asthma led to significantly fewer asthma exacerbations (absolute risk reduction [ARR], 16% vs 26%; odds ratio [OR] = 0.55; 95% CI, 0.42-0.60; number needed to treat [NNT] = 10) and fewer hospitalizations (ARR, 0.5% vs 3%; OR = 0.16; 95% CI, 0.06-0.42; NNT = 40).13
Significantly more patients in the omalizumab group were able to withdraw from, or reduce, the dose of ICS. GINA recommends omalizumab for patients with positive skin sensitization, total serum IgE ≥ 30 IU/mL, weight within 30 kg to 150 kg, history of childhood asthma and recent exacerbations, and blood eosinophils ≥ 260/mcL.16 Omalizumab is also approved for use in chronic spontaneous urticaria and nasal polyps.
Mepolizumab is a humanized MAb that inhibits IL-5, effectively blocking the growth, differentiation, recruitment, activation, and survival of eosinophils.14 Mepolizumab was studied in patients with frequent exacerbations while already taking high-dose ICSs. The mean rate of clinically consequential exacerbations was significantly reduced with mepolizumab compared with placebo (0.83 vs 1.74; P < .001).17 This translates to about 1 less moderate-to-severe asthma exacerbation per year per person.
Continue to: Another trial found that...