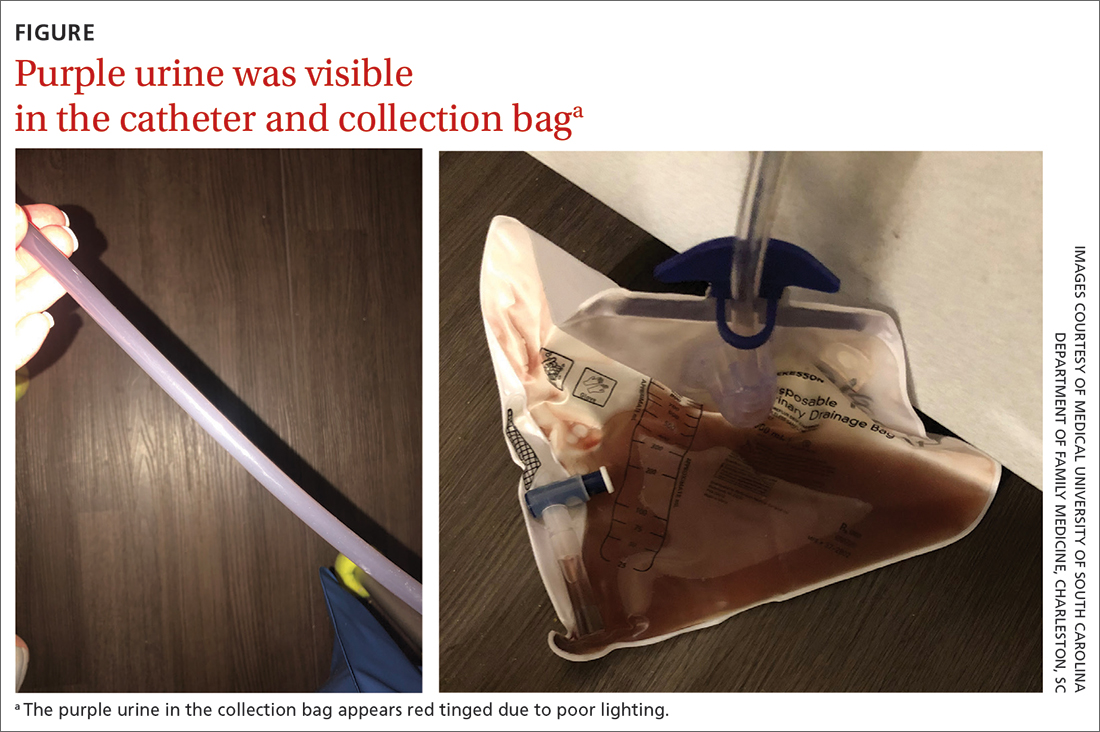
An 81-year-old man was admitted to our skilled nursing facility (SNF) after hospitalization for an acute kidney injury secondary to bladder outflow obstruction. While at the hospital, he received hemodialysis for the acute kidney injury, underwent transurethral resection of the prostate for benign prostatic hyperplasia (BPH), and had lithotripsy for nephrolithiasis. He was admitted to our SNF with an indwelling urinary catheter that had been placed 3 days prior to discharge from the hospital for urinary retention and a serum creatinine level of 3.28 mg/dL (normal range, 0.7-1.3 mg/dL [male]). Four days after his admission, the nursing staff reported acute onset of purple urine in his catheter and collection bag (FIGURE).
Physical examination revealed an older man whose vital signs were normal and who had a regular heart rate and rhythm. He denied any pain, and his abdomen was soft and nontender with normal bowel sounds. There was no suprapubic or costovertebral angle tenderness, and his urinary catheter was correctly placed. His urine output was within normal limits, but the urine in the catheter and collection bag was purple.
The patient’s medical history was remarkable for mild cognitive impairment, BPH, and hypertension. A urine culture was significant for > 100,000 CFU/mL pan-sensitive Pseudomonas aeruginosa.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?