LOS ANGELES – The prevalence of cerebral microbleeds increased from 24% to 28%, and microbleeds rarely disappeared over a mean of 3 years, in a study of 831 older adults in the general Dutch population.
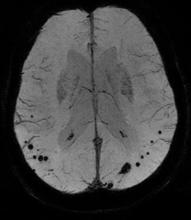
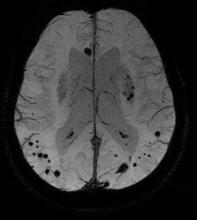
A subset of nondemented adults aged 60 years or older in the Rotterdam Study underwent brain MRI scans and other examinations in 2005-2006 and again in 2008-2010. Independent raters looked for microbleeds in side-by-side comparisons of the baseline and follow-up scans without knowing which was which and without access to other imaging or test results. The mean time between scans was 3.4 years.
People with microbleeds at baseline were five times more likely to develop new microbleeds. Among 203 people with microbleeds on the first scan, 25% had new microbleeds on the second scan compared with 5% of 628 people without microbleeds at baseline, Dr. Mariëlle M.F. Poels said at the International Stroke Conference.
The risk was even higher in people who had multiple microbleeds at baseline, who were seven times more likely to develop new microbleeds compared with people with no microbleeds on the initial scan, said Dr. Poels of Erasmus University, Rotterdam, the Netherlands.
The incidence of microbleeds increased with age, from 8% in people aged 60-69 years to 19% in people older than 80 years (Stroke 2011;42:656-61).
Previous longitudinal studies of cerebral microbleeds were smaller and focused on patients seen at memory clinics or patients with cerebral amyloid angiopathy instead of the general population.
The study used a three-dimensional T2*-weighted gradient-recalled echo sequence to detect microbleeds, defined as focal areas of very low signal intensity. The investigators used other MRI sequences to rate infarcts and used a validated tissue classification technique to assess white matter lesion volume. They collected DNA samples for apolipoprotein E genotyping.
Only six people (3%) had fewer microbleeds at follow-up compared with baseline. Four of these six had one microbleed on the initial scan and none at follow-up. The fifth person had two microbleeds at baseline and one at follow-up. The number of microbleeds in the sixth person decreased from 11 at baseline to 6 at follow-up, Dr. Poels said at the conference, sponsored by the American Heart Association.
In addition, another six people had some microbleeds on the initial scan that had disappeared at follow-up, but they also had new microbleeds, so their total number of microbleeds did not decrease over time. All but one of these six had more than five microbleeds at baseline and a higher number at follow-up.
In the entire cohort, 258 new microbleeds developed between the first and second scans, and only 18 microbleeds seemed to disappear. "Microbleeds rarely disappear," she said.
The location of microbleeds at baseline strongly predicted the location of new microbleeds. Of the new microbleeds, 60% were strictly lobar and 40% were either deep or infratentorial microbleeds.
Certain vascular risk factors for microbleeds were associated with the location of new microbleeds, suggesting that deep or infratentorial microbleeds are independent indicators of hypertensive vasculopathy, the investigators suggested.
High systolic blood pressure, high pulse pressure, and hypertension were associated with new deep or infratentorial microbleeds but not with new lobar microbleeds. Increasing serum total cholesterol was associated with a decreasing incidence of deep or infratentorial microbleeds on the follow-up scan.
The presence of lacunar infarcts at baseline was associated with a fourfold higher risk for new deep or infratentorial microbleeds at follow-up than in people without infarcts. A fourfold higher risk for new strictly lobar microbleeds was seen in people with the apolipoprotein E4 genotype. People with larger white matter lesion volume at baseline had double the likelihood of new microbleeds in any of the locations, compared with people with smaller white matter lesion volume at baseline.
"Microbleed assessment on T2*-weighted MRI may serve as a possible marker of both cerebral amyloid angiopathy and hypertensive vasculopathy progression," Dr. Poels said.
Controlling vascular risk factors in people who already have microbleeds may slow the progression of pathology and prevent symptomatic intracerebral hemorrhage, she suggested.
The 831 participants who completed both MRI scans were younger and healthier than the 231 people who dropped out of the study after the first scan, either because they refused a second scan or were ineligible to continue. This may have resulted in underestimation of the true incidence of microbleeds in the general population and underestimation of associations between risk factors and incident cerebral microbleeds, the investigators noted.