GRAPEVINE, TEX. – Policy makers are scrambling for ways to bring down health care spending, but what if it were as simple as telling physicians how much things cost?
A new study by investigators at Johns Hopkins Hospital in Baltimore, which looks at the impact of displaying cost data on laboratory tests, shows that physicians' behavior is affected by seeing the price of the tests they order.
To see how having cost data at the time of order entry would affect behavior, researchers at Johns Hopkins compiled a list of both the most frequently ordered and the most expensive laboratory tests in their hospital, based on 2007 data.
Costly tests were only included in the study if they were ordered at least 50 times during the year. The researchers then randomized the tests to be either active tests or concurrent controls. For active tests, the researchers displayed the price, based on 2008 Medicare allowable cost figures, on the hospital's computerized provider order entry (CPOE) system. For example, a blood gas was listed at $28.25 and a heme-8 lab was $9.37.
Results
During the 6-month intervention period from November 2009 to May 2010, there was a mean decrease of about $15,692 per test for the lab tests in which cost data was displayed in the CPOE, compared with a baseline period exactly 1 year earlier.
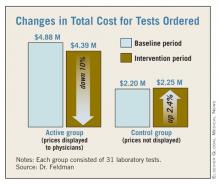
For all 31 of the active tests, there was a combined decrease of about $486,000, resulting in a 10% reduction among tests in which the costs were displayed. The active test costs dropped from $4,877,439 to $4,390,979. Among the group of 31 control tests, in which cost information was not listed on the CPOE, there was a mean increase of $1,718 per test. Overall, costs for the control group went up about $53,000 for all 31 tests.
The total number of tests ordered in the active group fell from 458,518 during the baseline period to 417,078 during the intervention. But in the control group, the number of tests rose from 142,196 to 149,455 during the study period.
Investigator Doesn't Find Results Surprising
Dr. Leonard Feldman, one of the study investigators and who is in the department of medicine at Johns Hopkins, said the results did not come as a surprise.
"I think many of us do recognize that a lot of these tests and imaging studies that are done are unnecessary," Dr. Feldman said during the annual meeting of the Society of Hospital Medicine.
Physicians order unnecessary tests for a number of reasons, he said, ranging from defensive medicine to patient expectations. But another reason is a lack of awareness of how much the tests cost, he said. "We, as doctors, have a limited understanding of diagnostic and nondrug therapeutic costs," Dr. Feldman said. "We just have no idea, mostly, how much things cost when we go to order them."
Study Limitations
While the study appears to show a relatively simple and inexpensive way to reduce the ordering of tests, Dr. Feldman acknowledged that the study had some limitations. For example, the study looked at only costs and did not include data on how the change in orders might have affected patient outcomes. And the intervention period was only 6 months.
Dr. Feldman said more time would be needed to show whether physicians would begin to ignore the costs over time. Similarly, costs were only displayed for 31 tests during the study. It's unclear if displaying all laboratory test costs would have the same effect on behavior, Dr. Feldman said.
The authors reported no financial disclosures.