COVINGTON, KY. – Providers continue to rely on blood cultures to detect serious bacterial infections in children with bronchiolitis, even though urinary tract infections are the most common culprit, a chart review shows.
"Even though there is outstanding evidence in the literature that cultures are unnecessary in the vast majority of infants with clinical bronchiolitis, this practice is common, has a cost, and false-positive results can result in prolonged length of stay and exposure to antibiotics that is unnecessary," according to researcher Dr. Brian Alverson.
Dr. Alverson of Hasbro Children’s Hospital in Providence, R.I., said the chart review supports other studies that show that the rate of UTI positivity is approximately the same as reported rates of benign transient bacteriuria in infants. Indeed, the incidence of UTI in the analysis was only 2.9% among patients who underwent urine testing, and the rates of meningitis and bacteremia were zero.
The study comprised 652 children, aged 1-24 months, with a discharge diagnosis of bronchiolitis. Of those, 26% had a blood culture obtained and 18.4% had a urinalysis or urine culture. Of patients undergoing blood cultures, 55% also had a urinalysis or urine culture.
"People who are going to look for infections aren’t looking in the right place," the study’s lead author, Dr. Jamie Librizzi, said at Pediatric Hospital Medicine 2012.
The findings are noteworthy since children in the analysis were discharged during 2007-2008 – after the American Academy of Pediatrics bronchiolitis practice guidelines recommending that clinicians should diagnose bronchiolitis and assess disease severity on the basis of history and physical examination.
The 2006 guidelines (Pediatrics 2006;118:1774-93) state that "the clinical utility of diagnostic testing in infants with suspected bronchiolitis is not well supported by evidence" and that "the occurrence of serious bacterial infections (SBIs) such as urinary tract infections (UTIs), sepsis, and meningitis is very low."
Despite the cohort being drawn from Hasbro Children’s Hospital and University of Missouri Children’s Hospital in Columbia, the misdirected testing could be explained by a knowledge gap and a wide variation in providers including residents, emergency department physicians, and referring community physicians, Dr. Librizzi said.
"Even though we know these guidelines are out there, the practices maybe still haven’t caught up to the evidence," she said. " ... It’s also hard when a kid comes in febrile, not looking great, to sit back and be assured that the numbers are really low for a concurrent infection."
"It’s a good reminder that we still have work to do educating our emergency departments," Dr. Paul Hain, now with Children’s Medical Center, Dallas, commented in a separate interview. "A lot of kids are seen in adult EDs, and folks who are not familiar with children are mostly scared of adult bacteremia and think that blood cultures are what they need, even though bronchiolitis is a special subset."
Children who were evaluated for an SBI received significantly more antibiotics and had significantly longer hospital stays, said Dr. Librizzi, formerly with Hasbro and now a hospitalist fellow at Children’s National Medical Center in Washington.
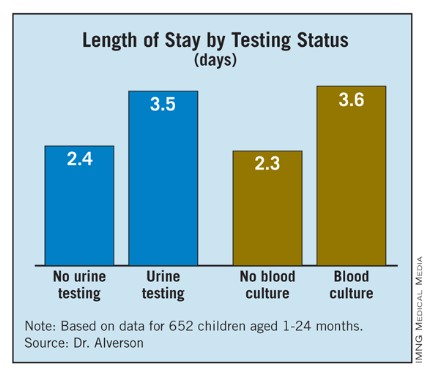
Length of stay (LOS) was 3.6 days for patients with blood cultures and 2.3 days for those without blood cultures, and 3.5 days for patients undergoing urine testing alone vs. 2.4 days for those without urine testing More than half (56.6%) of patients who underwent testing for an SBI received antibiotics, compared with 24% who did not.
Specifically, the percent of children receiving antibiotics was 17.5% among children with no urine testing (48/445); 48.6% for those with urine testing (51/105); 14% for those without blood cultures (58/411); and 51% for those with blood cultures (71/139), Dr. Librizzi said.
LOS for patients without an SBI who were on antibiotics was significantly longer than for patients off antibiotics (3.7 days vs. 2.5 days).
All of the children in the study were deemed to have bronchiolitis based on the note of the ED physician, or the ward’s physician for direct admissions. Their mean age was 5.6 months, 19% were premature infants, and 57% were male.
Patients were considered positive for a UTI if cultures grew more than 10,000 colony-forming U/mL of a single organism, or in the absence of culture results, if urinalysis was positive for leukocyte esterase and/or nitrites with evidence of pyuria (more than five white blood cells/high-power field).
Patients were considered bacteremic if blood cultures were positive for a pathogen not deemed a contaminant in more than one set, the authors reported in a poster at the meeting, sponsored by the Society of Hospital Medicine, American Academy of Pediatrics, and Academic Pediatric Association.