A new, effective method of assessing tuberculosis infectiousness involves directly measuring aerosols from the coughs of pulmonary TB patients, according to a study published Jan. 10 in the American Journal of Respiratory and Critical Care Medicine.
An analysis of cough aerosols, when available, more accurately predicted transmission than did the traditional method of sputum smear microscopy or culture, reported Dr. Edward C. Jones López of Boston Medical Center and his associates (Am. J. Respir. Crit. Care Med. 2013 Jan. 10 [doi: 10.1164/rccm.201208-1422OC]).
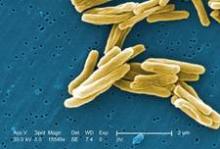
Therefore, the researchers analyzed the number of M. tuberculosis colony forming units (CFUs) in TB patients’ aerosols to see whether the CFU number better predicted new infection in contacts than did an AFB-positive smear. The study group included 96 adult TB patients with sputum AFB-positive culture and their 442 household contacts from May 2009 to January 2011.
The TB patients attended the Mulago Hospital National Tuberculosis and Leprosy Programme in Kampala, Uganda, and lived with at least three household contacts. All had an initial AFB of at least 1+ plus M. tuberculosis culture growth and had received fewer than 6 days of antituberculous treatment or no treatment.
A total of 45% of patients (43) produced culturable M. tuberculosis in aerosols during the two 5-minute coughing periods of sample collection. The 26% of total study group patients who produced high aerosols (at least 10 CFUs) were more likely to transmit an infection to their contacts than the 19% with low aerosols (1-9 CFUs) or the 55% of aerosol-negative cases. Ten was selected as a CFU cut-off, based on an associated increase in tuberculin skin test (TST) conversion risk at this number.
While 69% of the contacts of high aerosol patients were "at-risk" of TST conversion, 25% of contacts of low aerosol patients and 30% of contacts of aerosol negative patients were at risk of TST conversation (P = .009). New infections were diagnosed through a positive tuberculin skin test (TST) or interferon-gamma release assay (IGRA), with retests six weeks later for contacts who tested negative at baseline for both TST and IGRA.
TST conversion risk in low aerosol and aerosol-negative patient contacts was similar (odds ratio, 0.77; 95% confidence interval 0.27-2.17; P = .62). However, the risk in contacts of high-aerosol patients was over five times greater than in contacts of low-aerosol patients (OR, 5.18; 95% CI 1.52-17.61) before adjustment. An adjusted analysis yielded a similar odds ratio (OR, 4.81; 95% CI 1.20-19.23).
Meanwhile, "the same analysis using sputum AFB smear grade to classify exposure groups did not show a clear or consistent risk stratification," the authors wrote. Therefore, high-aerosol TB patients more accurately predicted new TB infections, based on risk of TST conversion.
"In addition to providing a more precise marker of source infectiousness, cough aerosols may help determine the individual risk of M. tuberculosis infection after exposure, which can be variable and is poorly understood," the authors wrote. Yet they acknowledge the limitation that cough aerosols’ predictive value over time is unknown.
They noted three primary implications of their findings, first of which is a "new framework for rational and cost-effective infection control decisions" since the common wisdom that all sputum AFB positive patients are equally infectious is no longer necessarily the case. They also noted that Latent Tuberculosis Infection treatment programs may be improved through more efficient selection of TB contacts with TB exposure.
Finally, the authors suggested that analyzing TB aerosols might offer more accurate classifications of contacts’ inhaled doses of TB, thereby potentially offering an opportunity to better understand how the immune system responds to TB. This information may, in turn, contribute to studies related to TB vaccines, medications and immune responses.
This study was supported by a University of Medicine and Dentistry of New Jersey Foundation award with matching funds from the Division of Infectious Diseases at New Jersey Medical School, funds from the section of infectious diseases at Boston Medical Center and support to Dr. Matthew Fox from the National Institute of Allergy and Infectious Diseases.