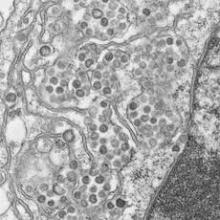
A coronavirus documented in four Saudi hospitals has caught the attention of investigators, who say its potential for easy transmission poses a challenge, particularly in health care settings. The team of experts investigating the recent cases of Middle East respiratory syndrome also investigated a deadly 2003 outbreak of severe acute respiratory syndrome (SARS) in Toronto hospitals and noted similarities between the two events, according to a report published online in the New England Journal of Medicine June 19.
Fifteen of 23 people with laboratory-confirmed Middle East respiratory syndrome coronavirus infections (MERS-CoV) died in the outbreak at four centers in eastern Saudi Arabia this spring
Fourteen of the 23 cases were in patients who caught the virus in the hemodialysis or, less frequently, intensive care or other units of a single 150-bed general hospital in Al-Hofuf. Some of those patients were transferred or sought hemodialysis at other facilities, spreading the infection. The outbreak likely originated from a probable case admitted originally for dizziness and diaphoresis, whose room was adjacent to a hemodialysis patient’s room (N. Engl. J. Med. 19 June 2013 [doi:10.1056/NEJMoa1306742]).
Proximity was the common denominator. In most cases, patients picked up the infection when they shared space or had a room near someone who was already symptomatic. "We are unable to determine whether person-to-person transmission occurred through respiratory droplets or through direct or indirect contact, and whether the virus was transmitted when contact was more than 1 meter away from the case patient," noted investigators from the Ministry of Health in Riyadh, Saudi Arabia; Johns Hopkins University in Baltimore; University College London; and elsewhere.
"Because some patients presented with gastrointestinal symptoms, and transmission appeared to occur between rooms on the ward, the current WHO [World Health Organization] recommendations for surveillance and control should be regarded as minimum standards. Hospitals should use contact and droplet precautions and should consider the follow-up of persons who were in the same ward as a patient with MERS-CoV infection,"they said.
WHO reported two cases of severe community-acquired pneumonia caused by MERS-CoV in September 2012. Since then, it’s been reported as a cause of pneumonia in Saudi Arabia, Qatar, Jordan, the United Kingdom, Germany, France, Tunisia, and Italy. The natural host and reservoir "remain unknown," they noted.
Three confirmed cases and two probable cases were in family members who visited symptomatic patients; an additional confirmed case was in a doctor who cared for them and a fifth in a nurse administrator who had face-to-face contact with the physician once he was symptomatic. No other cases were detected among 217 family members and more than 200 health care workers who came in contact with sick patients.
Once it was recognized, infection control measures contained the outbreak. The efforts included monitored hand hygiene, droplet and contact precautions for febrile patients, testing febrile patients for MERS-CoV, masking all patients undergoing hemodialysis, enhanced environmental cleaning, excluding patients with suspected infection from hemodialysis units, and banning contact with visitors and nonessential staff.
Symptoms included fever in 20 (87%) patients, cough in 20 (87%), shortness of breath in 11 (48%), and gastrointestinal symptoms in 8 (35%). "It is not yet known what proportion of ill patients shed virus in their stool," investigators said.
Twelve patients (52%) had end-stage renal disease, 17 (74%) had diabetes, 9 (39%) heart disease, and 10 (43%) lung disease. The majority had unilateral or bilateral infiltrates on chest x-ray; 17 (74%) cases were in men and 17 (74%) patients were 50 years or older. As of June 12, six patients had recovered from the infection and two remained hospitalized.
Among those who progressed, the median time for symptom onset to ICU admission was 5 days and median time to death was 11 days. The median incubation period was 5.2 days.
Infection was confirmed by reverse-transcriptase polymerase chain reaction. "Results of throat swabs were occasionally negative and repeat testing" was required. "It is not clear whether sputum of nasopharyngeal samples might be superior," the authors noted. There were 11 probable but not confirmed cases in the outbreak.
The investigators said that several similarities between MERS-CoV and SARS, also caused by a coronavirus, include a range of severity from "mild to fulminate"; a nonspecific early phase; heterogeneity in transmission, "with many infected patients not transmitting disease at all and one patient transmitting disease to seven others"; and gastrointestinal symptoms.
"The 65% case-fatality rate in this outbreak is of concern," but it may come down if more cases are identified, including those with mild symptoms, they said.