Assessing risk factors
Regardless of the risk assessment strategy, physicians should avoid overly aggressive preoperative investigation. The ACC/AHA state in their guideline on perioperative risk assessment that “intervention is rarely necessary simply to lower the risk of surgery unless such intervention is indicated irrespective of the preoperative context.”1
Coronary arteriography has a 0.3% mortality risk. Coronary artery bypass grafting (CABG) is associated with an overall operative mortality risk of 3%.11 In patients undergoing noncardiac surgery who have significant coronary artery disease without antecedent CABG, overall cardiac mortality is 2.4%, compared with 0.5% for those with antecedent CABG.12 Therefore, performing otherwise unnecessary bypass grafting simply to lower the risk of a subsequent surgical procedure incurs an antecedent mortality of greater than 3% from the CABG, whereas proceeding directly to the indicated procedure, on average, produces a 2.4% cardiac mortality.
However, patients who are otherwise candidates for CABG may be first identified when being evaluated for another surgical procedure. In such cases, when the intended surgery can be safely delayed, performing the CABG first is then most logical because the combined mortality of the procedures will be lowest when the CABG is performed first.
All of these tools focus exclusively on cardiovascular risk stratification or preoperative cardiac management (except the decision tool of Steyerburg et al 7; see below). Interestingly, few or none incorporate such risk factors as smoking, hypertension, or serum albumin, which are not independent predictors of major perioperative cardiac events. Two risk factors common to all algorithms are heart failure and prior myocardial infarction (MI). Seven of the 8 algorithms incorporate renal insufficiency, signs or symptoms of current coronary ischemia, and age. In branching algorithms, factors that may be included in an algorithm may not always be considered for a particular patient.
Electronic Decision Tools
STAT Cardiac Clearance
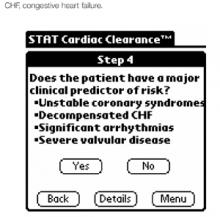
STAT Cardiac Clearance (STAT CC) version 1.1 (March 2002) is single-function software that exclusively performs cardiac preoperative assessment. After starting the program, the user chooses between the ACC/AHA 2002 algorithm and the ACP 1997 algorithm. Both of these algorithms provide management recommendations based on patient characteristics and surgical type. Both algorithms present users a series of yes/no questions (Figure 1), check boxes, and multiple choice questions, all completed by a tap with the stylus on the handheld computer’s touch-sensitive screen.
For the ACP algorithm, users eventually arrive at a management recommendation, such as “Sequence coronary revascularization and noncardiac management according to relative urgency of each and patient preference” or “Proceed directly to surgery.” Similarly, following the ACC/AHA algorithm, users receive recommendations such as “Operating room. Postoperative risk stratification and risk factor management.” The only problem in following either protocol’s implementation for the handheld is STAT CC-ACP algorithm’s use of “creatinine >260 mmol/L” (this value should be 260 μmol/L) and failure to note that this value is equivalent to 3 mg/dL. Both algorithms include patients with known coronary heart disease and patients undergoing major noncardiac and minor surgical procedures. The full text of the executive summary of the ACC/AHA article is available on STAT CC’s pull-down menu.
An addendum in the print version of the ACP protocol recommends “the perioperative use of atenolol in patients with coronary artery disease or risk factors for coronary artery disease… unless the patient has significant contraindications” based on information that became available after the guidelines were approved.2 This recommendation is not mentioned in the electronic implementation.
FIGURE 1
Stat Cardiac Clearance’s implementation of ACC/AHA guidelines
MedRules
MedRules (version 2.5, 2002) is a compilation of about 40 clinical prediction rules. Among these are 3 preoperative risk indices. Other than providing the literature citation for each rule, no assistance is provided in applying the rules. For example, users are not provided information to determine to which specific patient populations each rule applies.
MedRules’ Detsky calculator is a series of 3 screens of check boxes, all straightforward except the undefined “CCS Class” (Figure 2). Users can easily navigate among these screens to change entries if desired. The final result is a point total, risk class, and prediction of risk of major cardiac complications, eg, “15/100 points = class III: 20% risk of major cardiac complications.” Similarly, MedRules’ Goldman calculator is 3 screens of check boxes, also easily navigable in both directions.
In MedRules’ incarnation, an obvious major difference between the Detsky and Goldman implementations is Goldman’s categorization of surgical type into low-risk (minor) and high-risk (major) surgery. With other factors equal, risk of major cardiac complications may range from 3% (minor surgery) to 30% (high-risk procedure). An example result from MedRules’ Goldman index is “14/53 points = class III: 12% risk of major cardiac complications.” The original reference 4 and the software yield the same point totals and risk class.