In another case series, menstrual irregularities decreased from 40.4% to 4.6% following surgery (P<.001) among women who lost 50% of their excess weight.8 The incidence of urinary stress incontinence also decreased significantly (61.2% to 11.6%, P<.001 in this study8 ). The Swedish Obesity Study found significant improvements in Health-Related Quality of Life scores at 2 years with surgery vs conventional treatment.9
Bariatric surgery, including gastric bypass, has significant postoperative morbidity and mortality. Thirteen percent of patients in the Swedish Obesity Study experienced peri-operative complications, including pulmonary symptoms (6.2%), abdominal infection (2.1%), wound complications (1.8%), bleeding (0.9%), thromboembolic events (0.8%), and other miscellaneous complications (4.8%). Postoperative complications required reoperation for 2.2% of surgical patients, and there were 4 postoperative deaths (0.2% of the operative patients; 3 due to leakage, and 1 due to a technical laparoscopic error).2
Nutritional and vitamin deficiencies are common following gastric bypass, including deficiencies of vitamin B12, iron, folate, and calcium. Lifelong nutritional supplementation is generally necessary following this procedure.10
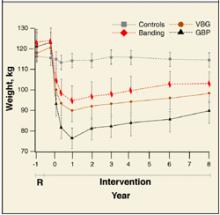
FIGURE 2
Long-term weight loss with bariatric surgery
Long-term weight loss with bariatric surgery: comparison of controls, horizontal gastric banding (Banding), vertical band-ed gastroplasty (VPG), and gastric bypass (GBP). Source: Sjostrom et al 2000. 3
Recommendations from others
A 1991 National Institutes of Health consensus conference suggested consideration of obesity surgery for patients with a body-mass index ≥40, or ≥35 plus severe obesity-related medical comorbidities (such as severe sleep apnea, obesity hypoventilation syndrome, obesity-related cardiomyopathy, or severe diabetes) who have not been successfully treated with non-surgical attempts at weight reduction.
Selected patients should be well-informed and motivated, with acceptable operative risk. A multidisciplinary team with medical, surgical, psychiatric, and nutritional expertise should evaluate patients who are candidates for surgery. An experienced surgeon, working in a clinical setting with adequate support for all aspects of management and assessment, should perform the surgery.
Lifelong medical surveillance is necessary after surgery, and patients should be selected who are likely to comply with this.11
Bariatric surgery is an important option for select patients
Tim Mott, MD
Family Practice Staff, Navy Hospital, Pensacola, Fla
The lack of successful interventions for obesity is frustrating. This is accentuated as obesity is increasingly recognized as the proverbial forest in which we find ourselves hacking at the “trees” of diabetes, hypertension, dyslipidemia, and many other diseases. As we focus on this, the second-leading preventable cause of death, we find ourselves uniquely skilled as family physicians to offer balanced advice and advocacy.12
Bariatric surgery is an important option for select patients. For such a patient, I continuously advocate for lifestyle changes, document all non-surgical measures pursued (important for third-party review), discuss realistic expectations and risks, and direct the patient to a trusted bariatric surgery center. For the postsurgical patient, I reinforce the lifestyle commitments, ensure ongoing vitamin and mineral supplementation, and help monitor for possible complications.