Polymerase chain reaction can be used to make a presumptive diagnosis but should be followed by culture confirmation. Direct fluorescent antibody testing of nasopharyngeal specimens and serologic testing for antibodies are not currently recommended as diagnostic tests by the CDC.
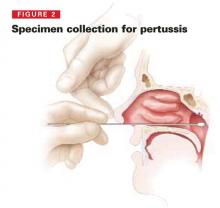
FIGURE 2
To collect a Bordella pertussis specimen, a nasopharyngeal swab should be performed in both nares. Insert the swab gently through the nostril toward the posterior nasopharynx; leave it there 15 to 30 seconds, then rotate it and remove. The sample should be put in an appropriate transport medium or immediately onto agar. (Choose shipping conditions based on how long the sample will be in transit; the laboratory will provide specific swab and transport medium requirements). Cotton swabs are not recommended because cotton is harmful to B pertussis. Cultures are usually incubated 10 to 14 days, but results are often available in 7 to 10 days.
Four antibiotics available for treatment of pertussis
The CDC’s recommended medications, doses, and duration of treatment are listed in TABLE 2.
Treatment, if started within the first 2 to 3 weeks, can reduce symptoms and clear B pertussis from the nasopharynx, thus reducing transmission to others. The CDC recommends initiating treatment as soon as pertussis is suspected.
Erythromycin is the agent with the longest history of use and most evidence for effectiveness. Due to its duration of therapy, however, and to the incidence of gastrointestinal side effects, it is less attractive to patients and physicians than other options.
New outcome studies of other macrolides are promising. Most authorities believe azithromycin and clarithromycin are acceptable alternatives and should achieve the same results as erythromycin.
Trimethoprim-sulfamethoxazole can be used for those older than 2 months, for those allergic to, or intolerant of, macrolides. The dose for children is 8 mg/40 mg per day in 2 divided doses for 14 days; for adults it is 320 mg/1200 mg per day in 2 divided doses for 14 days.
TABLE 2
Antibiotic treatment and chemoprophylaxis for pertussis
| AGE | AZITHROMYCIN (5-DAY COURSE) | ERYTHROMYCIN (14-DAY COURSE) | CLARITHROMYCIN (7-DAY COURSE) |
|---|---|---|---|
| <1 month | Recommended in this age group. 10 mg/kg/d in a single dose for 5 days | Not preferred due to association with pyloric stenosis. If used dose is 40–50 mg/kg/d divided in 4 doses for 14 days | Not recommended |
| 1–5 months | 10 mg/kg/d in a single dose for 5 days | 40–50 mg/kg/day divided in 4 doses for 14 days | 15 mg/kg/d in 2 divided doses (maximum 500 mg/dose for 7 days) |
| ≥ 6 months | 10 mg/kg/d in a single dose on day 1 then 5 mg/kg/d on days 2–5 | 40–50 mg/kg/d divided in 4 doses for 14 days | 15 mg/kg/d in 2 divided doses (maximum 500 mg/dose for 7 days) |
| Adults | 500 mg single dose on day 1 then 250 mg on days 2–5 | 2 g/d in 4 divided doses for 14 days | 500 mg twice a day for 7 days |
TABLE 3
Important public health functions for physicians in control of pertussis
| Be aware of the local infectious disease epidemiology and know when pertussis is circulating and increasing. |
| Think of the potential for pertussis in adults with a cough of two weeks duration or greater. |
| Collect nasopharyngeal specimens for culture on all patients with suspected pertussis. |
| Begin treatment when pertussis is suspected. |
| Report suspect and confirmed pertussis to the local public health department. |
| When pertussis is highly suspected or confirmed, begin chemoprophylaxis for family members. |
| Insure that respiratory hygiene is practiced in the clinic waiting areas. |
| Implement systems to insure that all patients are vaccinated according to CDC recommendations. |
| Insure that all clinic staff who have been exposed are given chemoprophylaxis and that symptomatic staff are excluded from work until after 5 days of treatment or until 21 days after cough onset if treatment is refused. |
| Collaborate with schools and local public health departments to evaluate symptomatic close contacts from schools and day care centers with outbreaks. This includes taking nasopharyngeal specimens for culture and initiating treatment if pertussis is suspected. |
Preventing infection in family members and close contacts
Those with pertussis are most infectious in the first 3 weeks of symptoms. The CDC recommends initiating chemoprophylaxis for all household and close contacts of those in whom pertussis is highly suspected or confirmed, regardless of the contacts’ age and vaccination status.
Close contacts are those with direct face-to-face contact with a symptomatic patient, or those who share a confined space for a prolonged period with the patient. Chemoprophylaxis is especially important for high-risk contacts: those under 1 year of age and those with chronic conditions that make them susceptible to complications from pertussis (eg, immune deficiencies, chronic lung disease, or cystic fibrosis).