A handful of papers published in the past few years have looked at different aspects of the current malpractice situation and have yielded some revelations (see page 775 in this issue) or data banks working on safety issues.
- Though it does a reasonable job at separating valid from invalid claims and compensating them accordingly, it often takes a tremendously long time to accomplish this and still has a 10% to 16% rate of false positive (payment with no error) and false negative (no payment with error) outcomes.
- The system is not overwhelmed with frivolous claims. Still, it costs a lot of money to manage, and less than half of this money goes to claimants.
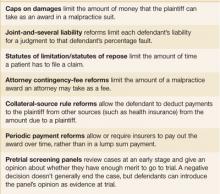
- Hard caps on total damages or noneconomic damages, unlike other state tort reforms (Figure), appear to reduce claims payments, physician premiums, and total health costs,7 while increasing physician supply.
- Defensive medicine exists, though putting a valid dollar amount on its costs is difficult.
- Anecdotal evidence suggests that physicians are leaving practice or limiting their practice (eg, family physicians discontinuing deliveries) as a result of malpractice costs.
FIGURE
Tort reforms commonly adopted by states
AMA’s proposal for change
Malpractice reform has been at or near the top of the AMA’s political agenda for the past 4 or 5 years, with strong lobbying efforts at the national level as well as support for state chapter efforts. The AMA’s proposal is based on California’s liability reform law known as MICRA that was passed over 30 years ago and has been associated with significantly lower premium growth since then compared with the rest of the US.8 Key provisions:
- Unlimited economic damages (medical expenses, future earnings)
- Limits on noneconomic damages (pain and suffering)
- Punitive damages, if available, up to $250,000 or 2 times economic damages, whichever is greater
- Allocation of damage awards in proportion to fault
- Sliding scale for attorney contingency fees.
Dubious premises. The AMA literature on malpractice includes valid information on the costs of the tort system, the rise in claims payouts, and effects on physician premiums. But it also suggests that meritless lawsuits are increasing. This is untrue. And its implication that physicians are increasingly leaving practice is anecdotal. There is no good research on the extent of this problem.8
Too narrow a focus. More important, the AMA plan is focused on physician premium costs while ignoring the unfairness of the system (eg, time to resolve claims, lack of payment for many patients with legitimate claims) and the vast number of medical errors for which claims are never filed.
The MEDIC proposal
Senators Hillary Clinton (D-NY) and Barack Obama (D-IL) have proposed federal legislation to address the malpractice crisis. Their bill would create an Office of Patient Safety in the Department of Health and Human Services, and would establish the National Medical Error Disclosure and Compensation (MEDIC) program within that office.9
Apologies would not be actionable in court. The MEDIC program would provide grants to physicians, hospitals, and health systems for the creation of programs to disclose medical errors to patients and negotiate fair compensation. The law would preserve confidentiality so that any apology offered by a health care provider as part of those negotiations would be kept confidential and could not be used in a trial. Any savings achieved from lower administrative and legal costs would be used to reduce physician malpractice premiums and toward patient safety initiatives.
Federal mandating of caps unlikely, however. At the federal level, Democrats have firmly opposed mandating caps on malpractice claims settlements. They argue that caps are unfair to patients who have been victims of medical errors. Others say this opposition reflects financial contributions from trial lawyers. It seems time to get past this conflict. Without dramatic changes in the composition of the Senate, which seems unlikely, there is little or no chance that caps will pass at the national level. At the same time, physician groups have been successful at achieving caps in a number of states (total of 26 at last count).
Signs this program could succeed. The MEDIC proposal is an attempt to find another way out of the malpractice impasse in the Senate by linking the patient safety and tort reform issues. It is primarily based on a growing movement to have physicians more directly acknowledge medical errors to patients,10 and in some cases, link these apologies to immediate financial negotiations to settle any potential claim of injury. The University of Michigan is the best known academic institution pursuing these strategies, and they report a significant decrease in the number of claims and annual litigation costs. The Lexington, Kentucky, VA Hospital has a similar program that has reduced liability costs compared with other VA hospitals.