What to do when the biopsy isn’t helpful
This case points out an important pathologic rule: If the biopsy doesn’t correlate with the observed disease, additional biopsies are indicated. Calciphylaxis is diagnosed on tissue microscopy, but the initial punch biopsy of the lesion revealed no significant pathologic abnormality. However, a subsequent deep-tissue biopsy showed extensive vascular wall calcification and septal fibrosis with subcutaneous fat necrosis.
Repeating abnormal laboratory testing is often appropriate, too. However, in this patient’s case, it probably would not have been helpful because she had intermittently elevated calcium levels over the years.
Wound cultures are often inaccurate in identifying a causative agent and this patient did not appear to have acute infection.
Management is mainly supportive
If you have a patient with calciphylaxis, address predisposing conditions such as hyperparathyroidism, hypercalcemia, and renal dysfunction5 (strength of recommendation [SOR]: C). In addition, discontinue calcium and vitamin D supplementation6 (SOR: C).
Finally, the patient will need meticulous wound care with adequate pain control; special attention to prevention of secondary infection is essential1,6 (SOR: C).
Our patient was one of the lucky ones
We treated this patient’s hypercalcemia, which was noted on admission to the hospital, with zoledronate and corrected her hypophosphatemia. Her renal function significantly improved with aggressive hydration.
With correction of electrolytes and normalization of kidney function, lesion progression was arrested. Granulation tissue developed in the lesions and split-thickness expanded skin grafts were performed on the large lesions (FIGURE 2). Fortunately, this patient survived despite the usual high rate of mortality. JFP
FIGURE 2
Good granulation beds, followed by closure
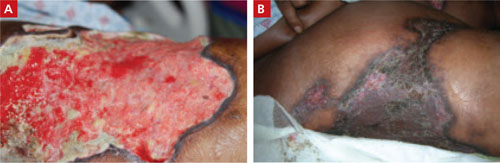
After aggressive treatment of renal dysfunction, correction of electrolyte abnormalities, and meticulous wound care, the patient’s lesions developed good granulation beds and showed signs of healing (A). The second image (B), taken 9 months after the patient first sought treatment for the lesions, shows the wounds after skin grafting.
CORRESPONDENCE
E.J. Mayeaux, Jr, MD, DABFP, FAAFP, Louisiana State University Health Sciences Center, 1501 Kings Highway, Shreveport, LA 71130; emayea@lsuhsc.edu

