TABLE 2
Clinical and laboratory findings associated with common causes of hyperthyroidism51-57
| Mechanism | Thyroid exam | Lab results | Radioactive iodine uptake | |
|---|---|---|---|---|
| Graves’ disease | Antithyroid antibodies | Diffuse goiter | Low TSH; elevated T3 and/or T4; elevated thyroid antibodies | Diffusely increased |
| Toxic multinodular goiter | Iodine deficiency | Goiter with multiple nodules | Low TSH; elevated T3 and/or T4 | Normal/increased uptake; "hot nodules" with suppression of extranodular tissue |
| Toxic adenoma | Benign thyroid hormone?secreting tumor; iodine deficiency | Palpable nodule | Low TSH; elevated T3 and/or T4 | Normal/increased uptake; functioning "hot nodule" on scan with suppression of surrounding thyroid tissue |
| Subacute thyroiditis | Viral | Tender thyroid on palpation | Low TSH; elevated T3 and/or T4; elevated ESR; elevated thyroid antibodies | Low uptake with poor imaging of the thyroid on scan |
| Factitious hyperthyroidism | Excessive intake of exogenous thyroid hormone | Normal exam | Low TSH; elevated T3 and/or T4; low thyroglobulin level | Low or normal uptake |
| Secondary hyperthyroidism | Excessive pituitary TSH | Goiter | Elevated TSH; elevated T3 and/or T4 | Diffusely increased uptake |
| ESR, erythrocyte sedimentation rate; T3, triiodothyronine; T4, thyroxine; TSH, thyroid-stimulating hormone. | ||||
Which laboratory tests to order, and what the results may mean
Rely on second- or third-generation TSH screening (normal=0.5-5 mIU/L), which is more sensitive and specific than measuring free T4 (thyroxine) alone.6
Older patients usually have a higher normal TSH level. In one study, 70% of patients >80 years had a TSH >4.5 mIU/L.7
If the TSH level is low (<0.5 mIU/L), measure free T3 (triiodothyronine) and free T4 levels, which are elevated in hyperthyroidism, and are normal in subclinical hyperthyroidism.
Patients with Graves’ disease tend to have T3 thyrotoxicosis with a T3T4 ratio >20.8 Isolated T4 thyrotoxicosis is more commonly seen with nonthyroidal illness as a result of decreased conversion from T4 to T3, and also in amiodarone-induced hyperthyroidism.9
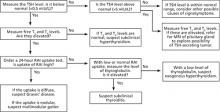
When further testing is needed (FIGURE). If the underlying cause of hyperthyroidism is not established on the basis of clinical findings (eg, diffuse goiter, myxedema, ophthalmopathy), order a 24-hour radioactive iodine (RAI) uptake test.10 Graves’ disease and toxic multinodular goiter exhibit increased RAI uptake that is diffuse and nodular, respectively. Subacute thyroiditis is associated with low RAI uptake (TABLE 2).
If RAI is contraindicated—eg, in pregnancy—testing for elevated levels of thyroid peroxidase antibodies (TPOab), TSH receptor antibodies (TRab), and thyroglobulin may help to differentiate Graves’ disease from multinodular goiter or uncover another autoimmune thyroid disorder.11 If a patient’s TSH, T4, and T3 levels are all elevated, refer him or her for magnetic resonance imaging of the pituitary gland to look for a TSH-secreting adenoma.
FIGURE
Suspect hyperthyroidism? Order these tests6-11
MRI, magnetic resonance imaging; RAI, radioactive iodine; T3, triiodothyronine; T4, thyroxine; TSH, thyroid-stimulating hormone.
Matching treatment to the underlying cause
RAI is usually the treatment of choice for patients without contraindications, although no randomized clinical trials have compared it with antithyroid medications or surgery.12 Each modality has its own risks and benefits (TABLE 3), and treatment selection should be individualized.
TABLE 3
Comparison of treatment modalities for hyperthyroidism12-21
| Antithyroid drugs* | Radioactive iodine* | Surgery | |
|---|---|---|---|
| Recurrence rate | High recurrence rate; no permanent hypothyroidism | Usually permanent hypothyroidism; long-term use of levothyroxine is required | Subtotal thyroidectomy associated with higher rates of recurrence or persistence of hyperthyroidism than total thyroidectomy; permanent hypothyroidism; long-term use of levothyroxine is required |
| Preferred method within treatment modality | MMI is the preferred medication; PTU is used with pregnancy and severe hyperthyroidism not responding to MMI | High ablative dose is preferred in MNG, toxic nodule, cardiac disease, elderly; low calculated dose is preferred in patients with GO | No outcome differences for GO, whether thyroidectomy is total, bilateral subtotal, or unilateral total and contralateral subtotal |
| Setting | Outpatient | Outpatient | Inpatient |
| Risks | No surgical risks | No surgical risks | Reaction to anesthesia, recurrent laryngeal nerve palsy, hypoparathyroidism |
| Adverse effects | ATD adverse effects, including life-threatening agranulocytosis | Worsening of Graves’ ophthalmopathy; transient exacerbation of hyperthyroid symptoms | Permanent hypothyroidism; hypoparathyroidism; anesthesia complications |
| Safety in pregnancy | PTU is used in pregnancy | Contraindicated in pregnancy/lactation | If surgery is indicated in pregnancy, it is best performed in the second trimester |
| ATD, antithyroid drugs; GO, Graves’ ophthalmopathy; MMI, methimazole; MNG, toxic multinodular goiter; PTU, propylthiouracil. *Concomitant use of ATD and RAI is associated with a high failure rate and persistent or recurrent hyperthyroidism. Discontinue ATD 2 weeks before radioactive iodine treatment. | |||
Radioactive iodine
In a 1990 survey, as many as 70% of specialists in the United States used RAI to treat hyperthyroidism, compared with just 22% of specialists in Europe.13 RAI is usually given in a single dose, and its maximal benefit is noted within 3 to 6 months. Two treatment methods are available: the ablative method and the gland-specific dosing method. Both have similar euthyroid state outcomes.14
The ablative method uses a high dose of RAI to achieve permanent hypothyroidism, necessitating lifelong levothyroxine replacement. This method is preferred for the elderly and for patients with cardiac disease, to achieve faster control of symptoms. It is also recommended for patients with toxic multinodular goiter and toxic nodules.