A 64-year-old woman came into our emergency department (ED) complaining of constipation and worsening rectal pain. In an attempt to promote her overall health, the patient had recently begun experimenting with healthy alternatives to her regular diet. Three days before her visit, she had ceased having stools and was experiencing intermittent abdominal cramping. She self-administered 2 bisacodyl suppositories, 2 sodium biphosphate enemas, one 10-ounce bottle of magnesium citrate, and 15 senna-containing laxative tablets without improvement.
She sought care at an urgent care clinic where she received 2 additional enemas and a trial of manual disimpaction—without results. She was sent home to rest and asked to return the next morning for another trial of disimpaction. When the patient’s efforts to manually disimpact herself at home were unsuccessful, she contacted her primary care physician, who arranged a house call. When his own protracted disimpaction procedure was unsuccessful, he referred her to our ED.
On presentation, the patient had lower abdominal and rectal discomfort. Her vital signs were normal except for a temperature of 38.8° C. Her abdomen was soft and nontender. Inspection of her perianal area revealed erythema and excoriations. On digital rectal exam (which was poorly tolerated because of pain), we noted a moderate amount of soft, clay-like feces in the rectal vault, with overflow liquid stool expulsion.
Computed tomography (CT) imaging of the abdomen was obtained to rule out rectal injury or colonic perforation (FIGURE 1).
FIGURE 1
CT scan reveals a speckled intraluminal mass
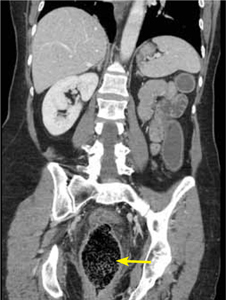
The patient had a markedly distended rectum and distal sigmoid colon caused by an intraluminal mass. Also present: circumferential wall thickening, perirectal edema without extraluminal gas, and generalized proximal colonic wall edema without a drainable collection.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?

