When speed is of the essence
There is no known antidote to aid in the reversal of dabigatran, rivaroxaban, or apixaban.4 Because of their relatively short half-lives, withholding the medication and providing supportive care is generally sufficient to ensure adequate hemostasis in cases of mild to moderate bleeding.4 If a patient presents with acute ingestion or an overdose, activated charcoal should be administered if the ingestion has occurred within the past 3 hours.4,24 The lack of a clear-cut reversal strategy can be extremely problematic in cases of trauma or life-threatening bleeding, however. (Fresh frozen plasma has not been shown to be effective at reversing NOACs’ effects.4)
In instances of severe bleeding or the need for urgent surgery, a more aggressive approach may be needed. Hemodialysis can be used to assist in the removal of dabigatran, but not rivaroxaban or apixaban.4 However, evidence suggests that the most effective therapy for patients who need rapid reversal of any NOAC is to administer 75 to 80 units/kg of activated prothrombin complex concentrate (aPCC).4,25-27 Recombinant factor VIIa has shown some promise in reversing the anticoagulant effects of these novel agents, but evidence is insufficient to recommend it as first-line therapy at this time.26, 27
Patients are more satisfied
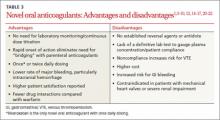
The most obvious advantage of the NOACs as a group compared with warfarin is the lack of need for laboratory monitoring or continuous dose titration. Reliably stable pharmacokinetics make once or twice daily dosing possible. A rapid onset of action negates the need for bridging therapy with parenteral anticoagulants in patients at high risk of thrombosis. This may improve compliance, as many patients are averse to the use of subcutaneous injections or need extensive education before they can safely self-inject. The incidence of heparin-induced thrombocytopenia may also be decreased if unfractionated heparin and LMWH are used less frequently.
NOACs also appear to improve patient satisfaction.20-22 In one study that included patients with AF on dabigatran or warfarin, satisfaction was higher in those taking dabigatran, particularly among those who did not experience significant GI adverse effects.20 Another study showed improved patient satisfaction with rivaroxaban compared with LMWH following lower extremity joint replacement, which led to significantly higher rates of compliance.22
… but problems and pitfalls remain
In addition to the lack of a readily available and clinically validated reversal agent, the absence of a lab test that reliably measures the concentration of NOACs makes it difficult to determine whether patients are following their prescribed regimen.3,4
Medication compliance must be assessed when considering a transition from warfarin to a NOAC. Switching patients with poor INR control on warfarin to a NOAC should be done only after determining that the poor control is not the result of nonadherence. Because of the NOACs’ shorter half-life, patients who don’t take them regularly may be at higher risk for thromboembolic events.1,12
Cost is a serious consideration. While there are some costs associated with the monitoring warfarin requires, the medication itself has been generic for several decades and can be found on many “$4 lists” at pharmacies nationwide. In contrast, all 3 NOACs are available only as branded drugs, and can cost a patient with limited drug coverage anywhere from $250 to $350 per month28—a serious concern, given that the likelihood of noncompliance increases as out-of-pocket costs rise. This was highlighted in a recent study that found patients were twice as likely to discontinue their cholesterol-lowering medication if 100% of the cost was out of pocket, compared with patients who had no prescription copay.29 From the perspective of the US health care system, however, NOACs have been found to be cost effective compared with warfarin, mostly due to the lack of laboratory monitoring.30-32
Adverse effects. The risk of GI bleeds has been shown to be higher in patients taking rivaroxaban and dabigatran vs warfarin.8,9 Dabigatran has also been associated with a significant risk for dyspepsia.5,8,14 In clinical trials, the reported rate for dyspepsia in patients taking dabigatran was 3% to 11%; subsequent investigations have found the incidence to be far higher (33%).8,14,33
Drug interactions. Warfarin has a large number of drug interactions, of course, but because of its long history, these interactions are well established. NOACs also have a number of drug interactions, but the true clinical impact has not yet been established. All 3 agents are substrates for the P-glycoprotein (P-gp) transport system, so any known inhibitors or inducers of the P-gp system should be used cautiously in patients on NOACs.1,3-7,12 Rivaroxaban and apixaban are also substrates for the CYP3A4 hepatic enzyme system, so any drugs known to inhibit or induce this system require caution, as well.1,3-7,12