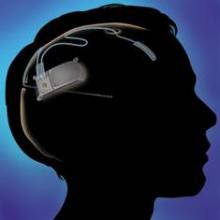
WASHINGTON – A recently approved device that provides responsive cortical stimulation was safe and provided sustained seizure reduction for a substantial number of patients with medically intractable partial onset seizures in a long-term efficacy and safety study.
The device – the RNS system (NeuroPace Inc.), which received Food and Drug Administration approval in November for use in adults – was associated with a median reduction in seizure frequency of 38.9% at 1 year and 51.1% at 2 years in 256 adult patients; 20% of patients were free of seizures for at least 6 months. No safety issues arose over a median of 4.5 years of follow-up (1,200 patient implant-years) as of Nov. 1, 2012, Dr. Gregory K. Bergey reported at the annual meeting of the American Epilepsy Society.
Study subjects had a mean age of 34 years and a mean epilepsy duration of 19.6 years. They were taking a mean of 2.9 antiepileptic drugs. Their seizures were localized to one or two seizure foci, and their median seizure frequency was 10.2 per 28 days, said Dr. Bergey, director of the Johns Hopkins Epilepsy Center in Baltimore.
The study population was extremely refractory, experiencing at least three debilitating seizures monthly and having no months with fewer than two such seizures, he noted.
The first 65 patients were implanted during an earlier 2-year feasibility study, and 191 additional patients were implanted during a 2-year, multicenter, double-blind, randomized, sham-controlled, pivotal study in which the RNS system was also found to be safe and effective as an adjunct treatment for adults with partial-onset seizures.
In the current long-term efficacy and safety study, no unanticipated device-related serious adverse events occurred, and the overall rate of device-related adverse events declined over time. The serious adverse event rate was 0.010 per implant-year for hemorrhage-related events, and 0.023 per implant-year for infection-related events. Most of these events occurred in the first year after implant.
Of 11 deaths that occurred during the study period, 2 involved suicide, 1 occurred because of complications associated with status epilepticus, 1 was because of lymphoma, and 7 were attributed to sudden unexpected death in epilepsy (including 2 among patients not being treated with responsive stimulation) for a rate of 2.5/1,000 patient stimulation-years.
"This new treatment is an option for patients with intractable partial seizures," Dr. Bergey concluded, adding that the current findings, which show progressive improvement over time, support the long-term safety and efficacy of the RNS system.
A 7-year, open-label phase of the study is ongoing to accumulate 9 years of prospective data for those implanted during the feasibility and pivotal studies.
Dr. Bergey reported having no disclosures.