CASE 1 › A 28-year-old woman (G0P0) came to our office with recurrent episodes of postprandial epigastric and right upper quadrant pain. Upper and lower endoscopy, sonography, body imaging, and laboratory tests were normal. A biliary nuclear scan showed an ejection fraction (EF) of 95%; normal is >35%. We made a diagnosis of biliary dyskinesia (BD) and recommended a laparoscopic cholecystectomy. The patient underwent this procedure and her pain was relieved. She has been much improved for 2 years, although she has since been diagnosed with an autoimmune disorder.
CASE 2 › A 21-year-old woman with right upper quadrant, postprandial, colicky pain presented to the emergency department. The episode lasted approximately 30 minutes and was followed by residual soreness. This episode was one of several that had been increasing in frequency and intensity. A sonogram showed a normal gallbladder and common duct. All laboratory tests were normal. She improved and was discharged. Outpatient evaluation included body imaging and endoscopy, which were negative. A hepatobiliary (HIDA) scan revealed an EF of 90%, and the scan reproduced her symptoms.
We diagnosed BD in this patient. After reviewing the risks and benefits of cholecystectomy, the patient consented to the procedure. She has been asymptomatic for 2 years.
Family physicians often are the first to evaluate patients with recurrent biliary colic. Biliary colic without gallstones—also known as BD or acalculous cholecystitis—is a functional disorder of the gallbladder or bile duct. Approximately 8% of men and 21% of women with biliary pain do not have gallstones.1-5
BD has been successfully treated with cholecystectomy. Physicians typically have viewed cholecystectomy as being effective primarily for patients with biliary pain who have a low EF (<35%).2-4 However, recent studies and our experience with cholecystectomy in these 2 patients with high EFs suggest that EF is only one of several factors to consider when deciding whether cholecystectomy might be appropriate for a given patient.
Which patients are most likely to benefit from cholecystectomy?
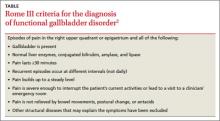
BD is a diagnosis of exclusion, considered when other upper abdominal disorders are eliminated. To receive a diagnosis of BD, patients must meet the Rome III criteria (TABLE).2
Before the advent of oral cholecystography in the 1920s, biliary disease was a clinical diagnosis confirmed by examination of the excised gallbladder.6 In 2 large studies conducted before cholecystography was in common use, researchers noted improvement in 75% to 85% of BD patients after cholecystectomy.7,8 Several years later, with the benefit, of cholecystography, Mackey9 reported similar improvement rates among patients with BD who underwent cholecystectomy.
Cholecystography has largely been replaced with HIDA scanning, which provides an objective measure of EF. Although some studies have suggested low EFs may predict which patients will benefit from cholecystectomy, others have suggested this value doesn’t tell the whole story.2,4,10,11 In some studies, patients who had biliary symptoms and a low EF (<35%) were found to be most likely to experience relief after cholecystectomy.2,4 More recently, in a chart review, DuCoin et al10 found that of 19 BD patients with an EF >35% who underwent cholecystectomy, 17 had complete symptom resolution, one had partial resolution, and one was unchanged. Only one abstract of a study of cholecystectomy for BD patients with a high EF (>80%) has been published.11 Of 28 patients who received cholecystectomy, 22 were asymptomatic after cholecystectomy and 5 others improved.11
Other tests to consider. A cholecystokinin infusion without a scan has been used to reproduce biliary colic; some physicians consider this to be diagnostic of BD and sufficient for cholecystectomy.12 Others have advocated endoscopic injection of botulinum into the sphincter of Oddi to differentiate pain arising from the sphincter of Oddi from pain in the gallbladder.5,13 If symptoms are relieved by this injection, an endoscopic biliary sphincterotomy—cutting of the biliary sphincter—is done. Cholecystectomy is reserved for patients whose pain is not relieved by botulinum. In an initial report, 25 BD patients received botulinum injections into the sphincter of Oddi; of the 11 whose pain was relieved by this injection, 10 underwent endoscopic biliary sphincterotomy, and pain resolved for all of these patients.13
Why we chose cholecystectomy for our patients
Despite a plethora of tests available to visualize and assess gallbladder and bile duct function, clinical assessment of BD by experienced physicians may be sufficient to determine which BD patients will benefit from cholecystectomy. In the cases we report on here, each patient had a high EF, but both met Rome III criteria and were experiencing clinically significant pain. Also, for both patients, a cholecystokinin infusion administered to calculate EF reproduced their pain. This clinical picture led us to recommend laparoscopic cholecystectomy, which ultimately relieved their symptoms.