The Centers for Medicare & Medicaid Services has begun the process of considering coverage of screening for cervical cancer with human papillomavirus testing.
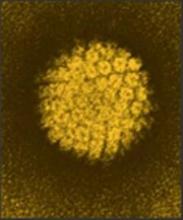
The agency announced Nov. 25 it has initiated a national coverage analysis at the request of the American Academy of Family Physicians to conduct the screening with a combination of HPV and cytology testing. “Our current coverage does not include the HPV testing,” CMS said in its announcement. Medicare currently covers a screening pelvic examination and Pap smear test for all female beneficiaries at 12- or 24-month intervals based on risk factors.
The CMS notes that the U.S. Preventive Services Task Force gives the HPV/cytology testing pathway an A grade for women aged 30-65 at 5-year intervals as an alternative to triennial Pap smears, a practice which also has a grade A recommendation.
The AAFP requested that Medicare cover the screening in an April 24 letter to the agency. The letter was sent the same day the Food and Drug Administration approved the cobas HPV test as a first-line screen for cervical cancer.
CMS expects to issue a proposed decision memo on May 25, 2015. Comments on the decision to open the analysis are due Dec. 25 and can be submitted through the CMS website.