PHOENIX – Adding a protocol of bundled nonpharmacologic interventions to the currently recommended standard of care nearly halved the amount of time patients spent delirious in the intensive care unit, a study has shown.
The combination of soothing music, natural light, routine cognitive stimulation, and the use of any necessary patient vision or hearing aids, added to standard ICU mobility and sedation protocols, also reduced the odds of developing any delirium, when researchers controlled for age, dementia, APACHE II score, and mechanical ventilation.
The data are from a prospective pre- and post–quality improvement cohort evaluation of the percentage of time patients spent delirious during their total medical ICU stay, rather than just the prevalence of delirium.
“We think this study really brings something unique to the knowledge of ICU delirium,” Ryan Rivosecchi, Pharm.D., a second-year resident at the University of Pittsburgh, said at the Critical Care Congress, sponsored by the Society for Critical Care Medicine. “Delirium is a disease of a waxing and waning nature, and purely going on its prevalence may not tell the full story.”
Currently, the recommendation with the highest level of evidence for preventing ICU delirium, as noted in the 2013 updated SCCM guidelines for pain, agitation, and delirium, is early mobilization. There are scant other evidence-based recommendations for how to prevent and treat the condition, leaving “a lot of practitioners wondering how they should take care of their delirious patients,” Dr. Rivosecchi said.
Delirium experienced during ICU stays has been associated with some form of residual cognitive impairment in more than 70% of patients and increases in lengths of stay by as many as 15 days. Delirium in the ICU has also been associated with a nearly 20% increase in mortality rates 6 months after admission to the ICU.
Noting that his institution already adhered to the standard recommendations for early mobility and sedation algorithms, Dr. Rivosecchi said he and his colleagues conducted the study at the University of Pittsburgh’s 24-bed medical ICU, in hopes of providing an additional evidence-based intervention to reduce ICU delirium.
Among 729 adult patients screened between September 2013 and April 2014, 230 patients who had not been in the ICU prior to MICU admission, and who did not present with delirium or baseline cognitive impairment, were chosen for the pre–quality improvement phase.
The post–quality improvement arm of the study comprised 253 patients who met the same criteria as did those in the first arm. The median age for both groups was 59 years. Slightly more than half of all patients were male.
The primary outcome was the total time a patient spent delirious throughout the entire MICU stay, as measured six times daily, every 4 hours, via the Intensive Care Delirium Screening Checklist. “Patients evaluated as ‘delirious’ at time point A were considered delirious for the next 4 hours until they were evaluated again at time point B,” Dr. Rivosecchi said.
During the first 3 months of the study, nurses on the MICU floor were unaware that baseline data about their unit were being collected. In the fourth month, the investigators discussed their observations with the nursing staff, and with the nursing director and clinician on the unit.
Several unique interventions, distilled from these meetings and a review of protocols already in place, were combined with findings from a systematic review of the literature, into one preventive protocol named M.O.R.E.: Music; Opening of blinds; Reorientation and cognitive stimulation; Eye and ear protocol.
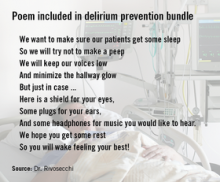
After the nurse meetings, another month passed before the post–quality improvement phase of the study began. The nurses were once again unaware data were being collected; however, according to Dr. Rivosecchi, not only did the entire medical staff, including the pharmacists, embrace the new protocol, but the nurses were so enthusiastic about it they collaborated on a poem to express their intentions to the patients and the patients’ families. Copies of the poem were placed in zippered pouches that included a sleep mask, ear plugs, and headphones, distributed to each MICU patient to help them block out unnecessary stimulation.
“The delirium prevention care bag was an idea the nurses came up with on their own to really help the patients out,” Dr. Rivosecchi said.
Signage detailing the specific actions included in the mnemonic M.O.R.E. was posted throughout the MICU to make it easier for the nursing staff to remember, although how the nurses implemented the protocol was left to them, Dr. Rivosecchi said.
The signs advised that MICU patients be exposed to at least 1 hour of “relaxing/soothing” music per nurse shift, and that if the patient were not actually viewing the television, it be kept off.