Cognitive restructuring of anxiety-provoking thoughts (eg, “Everyone will think I’m stupid”) and exposure to social situations and cues that patients with this disorder typically avoid are other key components of treatment.25,26 Exposure often occurs outside of the therapy setting. Patients may be instructed to go to a cafeteria and have lunch alone without looking at their phone or reading a book, for instance, or to go to a coffee shop and strike up a conversation with someone of the opposite sex while in line. Exposures within the therapeutic setting may involve associates of the therapist to help create an anxiety-provoking environment—eg, having a patient give an impromptu speech in front of an attractive associate of the opposite sex.
Where psychopharmacology fits in
While CBT is clearly a viable alternative to medication, psychopharmacology is sometimes indicated for anxiety or trauma-related disorders, depending on the diagnosis and on whether psychotherapy is ongoing.27 Evidence shows that specific types of drugs are effective for treating some anxiety-related disorders, while other medications may worsen symptoms (eg, selective serotonin reuptake inhibitors have demonstrated effectiveness in the treatment of PD, while benzodiazepines are contraindicated for patients with PTSD).27-29 Other research has found that a combined approach (psychotherapy plus medication) can be effective for the treatment of some anxiety disorders, including OCD.30 Although the combination may initially assist patients in their efforts to manage troublesome symptoms, in some cases it may limit the gains made from CBT.31
Talking to patients about CBT
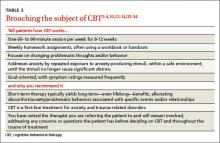
In discussing treatment options with patients with anxiety or trauma-related disorders (TABLE 3),2-4,10,12-14,32-34 it is important to note that psychotherapy—and particularly CBT—may be more cost-effective and have longerlasting effects than medication.32-34 Explain that it is a short-term treatment (typically lasting 9 to 12 weeks) but has been found to have long-term results.2-4,6,7 Point out, too, that patients who engage in CBT are likely to learn new skills, some of which may last a lifetime—and do not have to worry about adverse effects or potential drug-drug interactions as they would if they opted for psychopharmacology instead.
Finally, tell patients that you have vetted the practitioners you refer patients to and that you will continue to see them while they undergo treatment to ensure that the CBT is progressing well and following the established protocol.
CASE › Ms. S’s primary care physician considers prescribing alprazolam, but is concerned because this anti-anxiety medication can be habit-forming. Noting that although the patient is already taking sertraline, her distress related to the trauma appears to be worsening, the doctor suggests Ms. S try CBT. He explains that CBT is time-limited but has been found to have substantial long-lasting benefits for women who, like her, have been victims of sexual assault. The physician also tells Ms. S that CBT follows a specific protocol that typically consists of 9 to 12 weekly sessions; includes homework assignments and often follows a manual; is goal-oriented and measurable; and focuses on changing present behavior, thoughts, and feelings.
When Ms. S agrees to a referral, her physician assures her that he has vetted the practitioner and asks her to come in after 12 weeks of CBT so he can monitor her progress.
CORRESPONDENCE
Scott Coffey, PhD, Department of Psychiatry and Human Behavior, University of Mississippi Medical Center, 2500 North State Street, Jackson, MS 39216; scoffey@umc.edu