Even in this era of novel therapies for multiple myeloma, for patients with newly diagnosed disease, autologous stem cell transplant (ASCT) after chemotherapy provides benefits in terms of disease progression and extent of response, compared with chemotherapy alone. The benefit of ASCT was especially pronounced among certain groups of high-risk patients.
Novel proteasome inhibitors and immunomodulators “have dramatically increased the complete response rate and significantly extended progression-free survival and overall survival in previously untreated multiple myeloma patients,” Dr. Michele Cavo, head of the Seragnoli Institute of Hematology at the University of Bologna School of Medicine in Italy, said at a presscast in advance of the annual meeting of the American Society of Clinical Oncology.
But questions remain about how these newer agents perform, compared with high-dose melphalan (HDM) followed by ASCT, traditionally seen as the standard of care for younger and fit patients with newly diagnosed disease.
EMN02/HO95 is a large, prospective, multicenter, intergroup, randomized phase III study that addresses this question, as well as single vs. double ASCT and the use of consolidation therapy or not. The study includes patients 65 years old or younger, and the trial protocol involves induction therapy with bortezomib (Velcade)–cyclophosphamide-dexamethasone (VCD) and subsequent collection of peripheral blood stem cells.
Patients were then randomly assigned to receive bortezomib-melphalan-prednisone (VMP) or HDM as intensification therapy in centers that had a single ASCT policy. For those centers doing double (tandem) ASCT procedures, the randomization was to VMP vs. HDM + single ASCT vs. HDM + double ASCT.
Patients in each treatment arm then underwent another randomization to consolidation therapy with bortezomib-lenalidomide (Revlimid)–dexamethasone or no consolidation. All patients received lenalidomide maintenance until disease progression or toxicity. At the time of a preliminary analysis of trial data in January 2016, results from the second randomization to consolidation or no consolidation therapy were not yet complete. This first prespecified interim analysis was performed after at least 33% of the required events had occurred.
Early results show ASCT benefit
Early results on 1,266 patients (VMP, n = 512; HDM, n = 754) show that a median progression-free survival (PFS) was not yet reached after a median follow-up of 23.9 months from the first randomization (to VMP vs. HDM+ASCT), the primary endpoint of the trial.
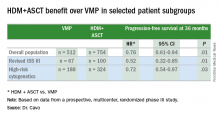
In the overall patient population, patients achieved a significant 24% benefit in PFS when given HDM+ASCT up front (hazard ratio, 0.76 vs. VMP), and this benefit extended to certain patient subgroups, as well.
“PFS benefit with bortezomib-based ASCT was of relevance for patients at high risk of early relapse, in particular for those with revised ISS [International Staging System] stage III and high-risk cytogenetic profiles, who had a relative reduction in the risk of progression or death of 48% and 28%, respectively,” Dr. Cavo said.
Other predictors of longer PFS were ISS stage I (HR, 0.44; 95% confidence interval, 0.28-067; P less than .0001), standard risk cytogenetics (HR, 0.57; 95% CI, 0.41-0.78; P less than .0001), randomization to the HDM+ASCT arm (HR, 0.61; 95% CI, 0.45-0.82; P = .001), and less than 60% bone marrow plasma cells (HR, 0.67; 95% CI, 0.48-0.99; P = .014).
More patients receiving ASCT up front had a significantly greater reduction in tumor volume of at least 90%, as indicated by the composite of very good partial remission, complete response, and stringent complete response, which was achieved in 74.0% in the VMP arm and in 84.4% of the HDM+ASCT arm (P less than .0001).
For patients at low risk of relapse, Dr. Cavo said longer follow up will be needed to compare the different arms of the study, and future analyses will delineate the effects of consolidation or no consolidation therapy and the use of the VMP regimen, compared with single or double ASCT.
ASCO president Dr. Julie Vose said that even with effective novel agents available, older, proven approaches still retain their value. “This study demonstrated that combining the best of both worlds – initial therapy with a novel agent followed by stem cell transplant – resulted in the best patient outcomes,” she said.