Preclinical research suggests a small-molecule inhibitor could potentially improve the donation and transplant of hematopoietic stem cells (HSCs).
One study showed that the inhibitor, CASIN, could improve HSC yields from murine transplant donors.
Another study showed that CASIN could be used as conditioning, with or without fludarabine, in murine transplant recipients.
Yi Zheng, PhD, of Cincinnati Children’s Cancer and Blood Diseases Institute in Ohio, and his colleagues conducted both studies and reported the results in Leukemia.
Previous research had shown that genetic ablation of CDC42 in HSCs mobilizes the cells without affecting their survival. CDC42 is a Rho family small GTPase that helps regulate HSC maintenance.
Dr. Zheng and his colleagues expanded upon this finding with two studies.
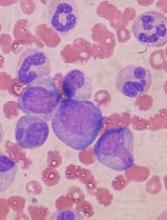
In the first study, the researchers identified CASIN, a small-molecule inhibitor of CDC42. The team tested CASIN in mice and found the inhibitor can effectively mobilize HSCs.
In fact, CASIN and plerixafor mobilized a similar number of phenotypic HSCs. However, HSCs harvested from CASIN-treated donor mice had better long-term reconstitution potential after transplant than HSCs harvested from plerixafor-treated mice.
In the second study, Dr. Zheng and his colleagues used CASIN to condition mice that were receiving HSC transplants.
The team found that CASIN reduced the number of phenotypic long-term HSCs in the bone marrow, starting 2 hours after CASIN administration and ending within 24 hours.
The researchers also found that CASIN synergized with fludarabine. Engraftment of transplanted HSCs was significantly higher in mice that received conditioning with CASIN and fludarabine than in mice that received either CASIN or fludarabine alone.
“Our data demonstrate that the new regimen of CASIN application has the potential to improve both sides of the transplant practice,” Dr. Zheng said. “It mobilizes higher quality donor HSCs during stem cell harvest, and it would condition transplant patients beforehand to increase engraftment efficiency.”
“This would be a major step forward, especially for the most vulnerable patients who cannot withstand the toxicity of chemotherapy conditioning regimens or are non-responsive to current [HSC] mobilization regimens.”
Both of these studies were funded, in part, by the National Institutes of Health. The authors declared no conflicts of interest.