Disrupting mitophagy may be a “promising strategy” for eliminating leukemia stem cells (LSCs) in acute myeloid leukemia (AML), according to researchers.
The team found that AML LSCs depend on mitophagy to maintain their “stemness,” but targeting the central metabolic stress regulator AMPK or the mitochondrial dynamics regulator FIS1 can disrupt mitophagy and impair LSC function.
Craig T. Jordan, PhD, of the University of Colorado in Aurora, and his colleagues reported these findings in Cell Stem Cell.
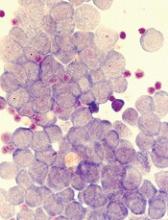
The researchers said in vitro experiments showed that LSCs have elevated levels of FIS1 and “distinct mitochondrial morphology.”
When the team inhibited FIS1 in the AML cell line MOLM-13 and primary AML cells, they observed disruption of mitochondrial dynamics. Experiments in mouse models indicated that FIS1 is required for LSC self-renewal.
Specifically, the researchers said they found that depletion of FIS1 hinders mitophagy and leads to inactivation of GSK3, myeloid differentiation, cell-cycle arrest, and loss of LSC function.
Dr Jordan and his colleagues also found that AMPK is an upstream regulator of FIS1, and targeting AMPK produces similar effects as targeting FIS1—namely, disrupting mitophagy and impairing LSC self-renewal.
The researchers said their findings suggest that mitochondrial stress generated from oncogenic transformation may activate AMPK signaling in LSCs. And the AMPK signaling drives FIS1-mediated mitophagy, which eliminates stressed mitochondria and allows LSCs to thrive.
However, when AMPK or FIS1 is inhibited, the damaged mitochondria are not eliminated. This leads to “GSK3 inhibition and other unknown events” that prompt differentiation and hinder LSC function.
“Leukemia stem cells require AMPK for their survival, but normal hematopoietic cells can do without it,” Dr Jordan noted. “The reason this study is so important is that, so far, nobody’s come up with a good way to kill leukemia stem cells while sparing normal blood-forming cells. If we can translate this concept to patients, the potential for improved therapy is very exciting.”