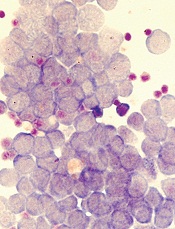
Image by Robert Paulson
Two groups of researchers have reported results that help explain how leukemia resists treatment with BET inhibitors.
One group was able to grow and maintain leukemia stem cells (LSCs) in vitro, and their subsequent experiments showed how LSCs react to BET inhibition.
The other group found evidence to suggest that by measuring Wnt signaling markers, we might be able to predict which patients will respond to BET inhibition.
Both groups described their research in letters to Nature.
“[T]he risk of resistance developing is common in any cancer treatment,” said Mark Dawson, PhD, a researcher at Peter MacCallum Cancer Centre in East Melbourne, Victoria, Australia and an author of the LSC study.
“Knowing precisely how that happens in advance puts us one step ahead in outmaneuvering the disease. Being able to grow and maintain leukemia
stem cells in vitro also gives us unprecedented access and insight into how they work so we can find new and better ways to target and destroy them.”
In their study, Dr Dawson and his colleagues assessed BET inhibitor resistance in a model of acute myeloid leukemia.
The team transduced murine hematopoietic stem and progenitor cells with MLL–AF9 and treated the cells with the BET inhibitor I-BET or dimethylsulfoxide (vehicle). They then isolated individual blast colonies to generate 4 vehicle-treated and 5 I-BET-resistant cell lines.
The researchers found that resistance to I-BET also conferred resistance to the chemically distinct BET inhibitor JQ1 and to genetic knockdown of BET proteins.
Further investigation revealed that resistance to BET inhibitors emerges from LSCs, both ex vivo and in vivo. And that resistance is, in part, a result of increased Wnt/β-catenin signaling.
The researchers noted that not all LSCs are intrinsically resistant to BET inhibition, but a small proportion of them are either transcriptionally primed or display rapid transcriptional plasticity to survive the initial BET inhibitor challenge. The team said these cells then thrive and become the dominant population.
These findings are consistent with results of the other study, conducted by Johannes Zuber, MD, of the Research Institute of Molecular Pathology in Vienna, Austria, and his colleagues.
With this study, the researchers set out to determine why only certain leukemia subtypes are sensitive to BET inhibitors. Their experiments revealed that loss of the PRC2 complex, which is known to inactivate genes during normal development, can render leukemia cells resistant to BET inhibitors.
By further characterizing these resistant cells, the team found that MYC and other BRD4-regulated genes (which are turned off by BET inhibitors) were back on again. So the leukemia cells had found a way to activate these genes in the absence of BRD4.
The researchers then compared leukemia cells that had acquired resistance during BET inhibitor treatment to leukemia cells that were resistant in the first place.
In both cases, the cells used similar pathways to turn critical genes such as MYC back on and thereby escape the effects of BET inhibition. A pathway that proved particularly important was the Wnt signaling pathway, which is known to activate MYC in cancers.
To determine whether this knowledge could be used to predict which patients will respond to BET inhibitors, the researchers measured Wnt signaling markers in samples from leukemia patients.
The team found that cells with low Wnt activity were sensitive to BET inhibitors, while high Wnt activity was associated with resistance.
Specifically, the researchers quantified 9 Wnt-associated transcripts in sensitive and resistant samples. Three of these transcripts—TCF4, CCND2, and HOXB4—were significantly overexpressed in resistant samples.
So the team used these 3 transcripts to establish a “resistance index” that, they believe, may provide a first step toward developing a predictive biomarker.
The researchers said, collectively, their study reveals that leukemia cells can become resistant to BET inhibitors by rewiring the regulation of critical BRD4 target genes. This transcriptional plasticity highlights an emerging mode of drug resistance that is distinct from established resistance mechanisms such as mutations in binding pockets or drug elimination through efflux pumps.
Dr Zuber and his colleagues believe that a better understanding of these adaptation mechanisms will lead to combination therapies that will ultimately “outsmart” cancer cells.
“We now have learned that cancer cells can adapt to targeted therapies, but their repertoire of escape routes is quite limited,” Dr Zuber said. “A better understanding of the common escape routes will allow us to predict the next effective targeted therapy so that we are always one step ahead of the cancer cell.”


