An upset in the body’s natural balance of gut bacteria that may lead to life-threatening bloodstream infections can be reversed by enhancing an
immune response, according to research published in Nature Medicine.
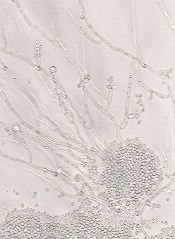
Researchers found that a transcription factor known as HIF-1α works with LL-37, a naturally occurring antibiotic, to kill the infection-causing fungi Candida albicans.
And this response can be enhanced with a drug called L-mimosine.
The researchers noted that Candida albicans can be lethal if it invades the bloodstream from the gut. And stem cell transplant recipients and immunosuppressed cancer patients have a high risk for this type of infection.
“For a cancer patient with a Candida bloodstream infection, the fatality rate is about 30%, [and] Candida is the number 1 fungal pathogen,” said study author Andrew Koh, MD, of the University of Texas Southwestern Medical Center in Dallas.
With that in mind, he and his colleagues set out to determine how the body’s natural immune defense system might be enhanced to fight a Candida infection. By studying how mice infected with Candida responded in different scenarios, the team found their answer.
“The commensal bacteria stimulate gut tissue to make a transcription factor and a natural antibiotic, which then kills the Candida fungus,” Dr Koh explained.
“When we gave the mice a pharmacologic agent called L-mimosine that stimulates the transcription factor, the agent knocked down Candida 100-fold, which translated into a 50% reduction in mortality from invasive Candida infection.”
Specifically, the researchers found that enhancing the transcription factor HIF-1α with L-mimosine led to increased production of the natural antibiotic peptide LL-37, which, in turn, killed the fungi. L-mimosine is a natural product derived from seeds of the koa haole tree that is known to boost HIF-1α activity.
The study also suggested that certain gut bacteria—Clostridial Firmicutes and Bacteroidetes—may be important in producing short-chain fatty acids that help fight infection.
The researchers said more work is needed to pinpoint the optimal method of inducing the body’s gut defense system, whether through use of an agent like L-mimosine or by administering short-chain fatty acids such as vinegar.
“Can we modulate the gut system to maintain balance so that it never gets to the point of pathogens invading the bloodstream?” Dr Koh asked. “Boosting [gastrointestinal] mucosal immune effectors to reduce fungal burden may be the key to tipping the balance back toward normal and preventing invasive fungal disease.”


