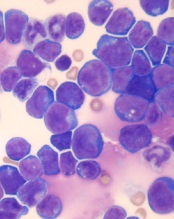
© Hind Medyouf, German
Cancer Research Center
A new study suggests that minimal residual disease (MRD) alone is not predictive of outcomes in children with T-cell acute lymphoblastic leukemia (T-ALL).
Study investigators analyzed a small group of T-ALL patients who received similar treatment regimens, comparing those with and without MRD after induction.
None of the MRD-positive patients relapsed within the follow-up period, despite not receiving intensified treatment to fully eradicate their disease.
These results, published in Pediatric Blood & Cancer, suggest T-ALL patients with MRD may not need intensified treatment and can therefore avoid additional toxicities.
“Until now, the dogma has been that, for patients with leukemia who have minimal residual disease at the end of induction, we need to intensify their treatment, which also increases side effects,” said study author Hisham Abdel-Azim, MD, of Children’s Hospital Los Angeles in California.
“We have found, for T-ALL, patients have excellent outcomes without therapy intensification and its associated toxicities.”
Dr Abdel-Azim and his colleagues studied 33 children (ages 1 to 21) with newly diagnosed T-ALL. Their treatment included induction, augmented consolidation, interim maintenance (high-dose [5 g/m2] or escalating-dose intravenous methotrexate), 1 delayed intensification, and maintenance. Twenty-one patients underwent cranial irradiation, and 1 received a transplant.
After induction, 19 of the 32 patients analyzed had MRD, which was defined as ≥ 0.01% residual leukemia cells. At the end of consolidation, 6 of the 11 patients tested were MRD-positive. And at the end of interim maintenance, 2 of the 4 patients tested were MRD-positive.
The 19 patients who were MRD-positive after induction were in continuous complete remission at a median follow-up of 4 years (range, 1.3-7.1 years). The same was true for 13 of the 14 MRD-negative patients. One of the MRD-negative patients relapsed 18 months after diagnosis but was still alive with refractory disease at last follow-up.
Dr Abdel-Azim and his colleagues noted that there were no significant differences in treatment variables between MRD-positive patients and MRD-negative patients. However, 1 patient did receive a transplant for rising MRD at 5.4 months after diagnosis.
The investigators also said they did not find any associations between MRD positivity after induction and patients’ age, sex, ethnicity, weight, white blood cell count at diagnosis, cytogenetics, immunophenotype, or the type of steroid they received during induction therapy.
The team said these results may be explained by the fact that clearance of leukemia cells from the blood is slower in patients with T-ALL than in those with B-cell ALL. However, the leukemia cells ultimately clear in T-ALL without changes in therapy.


