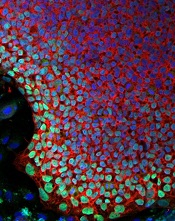
Image courtesy of the Salk
Institute of Biological Studies
Researchers say they have devised a way to correct a genetic defect in cells from a patient with X-linked severe combined immunodeficiency (SCID-X1).
The group generated induced pluripotent stem cells (iPSCs) using a sample from an infant with SCID-X1, then used the gene-editing technique TALEN to correct the defect in those iPSCs.
And this allowed the iPSCs to generate mature natural killer (NK) cells and T-cell precursors.
The researchers said this is the first evidence of genomic correction of iPSCs derived from a patient with SCID-X1 that resulted in the regeneration of mature lymphoid cells in vitro.
And the work, which is published in Cell Stem Cell, holds promise for the development of new treatments for this disease.
“This work demonstrates a new method that could lead to a more effective and less invasive treatment for this devastating disease,” said study author Inder Verma, PhD, of The Salk Institute of Biological Studies in La Jolla, California.
“It also has the potential to lay the foundation to cure other deadly and rare blood disorders.”
Dr Verma and his colleagues began this research by securing a sample of bone marrow from a deceased infant with SCID-X1. The subject harbored a novel splice-site mutation (c.468+3A > C) of the IL-2Rγ gene, which results in a lack of functional NK and T cells.
The researchers used the subject’s sample to create iPSC lines and used TALEN to correct the mutation in those iPSCs.
“We use TALEN-based genome editing to change just one nucleotide in one gene to correct the deficiency,” said study author Tushar Menon, PhD, also of the Salk Institute. “The technique is literally that precise.”
The team then compared the corrected iPSCs to uncorrected SCID-X1 iPSCs and control iPSCs generated from cord-blood-derived endothelial cells and dermal fibroblasts.
Like control cells, the corrected iPSCs were able to differentiate into mature NK cells that expressed both inhibitory and activating receptors (KIR/CD158b and CD16, respectively).
The corrected iPSCs could also differentiate into T-cell precursors but not mature T cells. The researchers are currently working on producing mature T cells.
“Ultimately, we hope these efforts will help lead to the ‘holy grail’ in the field: the ability to create stem cells from iPSCs capable of generating all types of blood and immune cells,” Dr Verma said.
He and his colleagues noted, however, that further improvements of their protocol will be needed to obtain sufficient cells for clinical use.


