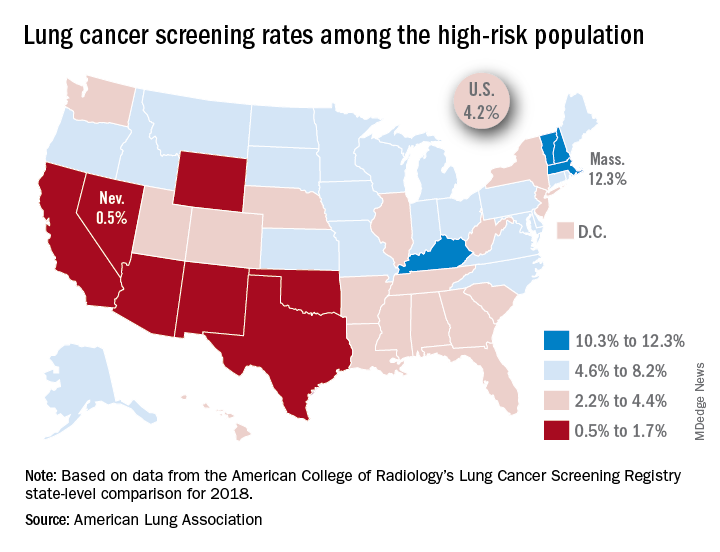
That disparity might suggest that Massachusetts has an exceptionally high rate, but it’s only 12.3%. And that means Nevada’s rate is very low, which it is: Only 0.5% of those at high risk are getting screened with annual low-dose CT scans, the ALA said in its 2019 State of Lung Cancer report.
“[The low rate of screening] may be because of a lack of access or low awareness and knowledge among patients and providers. As rates vary tremendously between states, it is clear that more can be done to increase screening rates,” the ALA stated.
Nationally, the screening rate is 4.2% among those at high risk for lung cancer, but “if everyone currently eligible were screened, close to 48,000 lives could be saved,” the ALA noted in its report.
Six states other than Nevada are below the 2% mark: Arizona, California, New Mexico, Oklahoma, Texas, and Wyoming. Besides Massachusetts, the three other states above 10% are Kentucky, New Hampshire, and Vermont, according to data from the American College of Radiology’s Lung Cancer Screening Registry state-level comparison for 2018.
For individuals at high risk for lung cancer – those aged 55-80 years who have at least a 30 pack-year history and either still smoke or have quit within 15 years – “screening with annual low-dose CT scans can reduce the lung cancer death rate by up to 20% by detecting tumors at early stages when the cancer is more likely to be curable,” the ALA wrote.