ORLANDO – Sevuparin, a novel nonanticoagulant heparinoid drug, showed no efficacy for acute vaso-occlusive crisis (VOC) in patients with sickle cell disease (SCD) in the randomized, controlled, phase 2 TVOC01 trial, but its promising safety and broad mechanism of action warrant further exploration in the prodromal VOC setting, according to investigators.
Time to VOC resolution – the primary study endpoint – was similar at about 168 hours in 71 hospitalized patients randomized to receive sevuparin and in 76 who received placebo (intention-to-treat hazard ratio, 0.89), Bart J. Biemond, MD, explained during a presentation of the findings at the annual meeting of the American Society of Hematology.
A per-protocol analysis based on the 69 and 75 patients dosed in the treatment and placebo arms, respectively, showed a similar result (HR, 0.81), said Dr. Biemond of the department of clinical hematology, Amsterdam UMC, Academic Medical Center, the Netherlands.
Secondary endpoints, including mean change in pain intensity from baseline on a visual analogue scale (VAS), duration of severest pain measured as time to achieve a 30% reduction in VAS score from baseline, and cumulative use of parenteral opioids, also did not differ between the treatment and placebo arms, he added.
Patients in the global, double-blind, multicenter trial were aged 12-50 years (median, 22 years) with any type of SCD. They were enrolled from 16 sites in 7 countries to receive a loading dose of 3 mg/kg of sevuparin and continuous 18 mg/kg per day infusions or placebo. Patients in both arms also received standard-of-care and parenteral opioid therapy.
The groups were generally balanced with respect to demographic and baseline characteristics, Dr. Biemond said, noting that the treatment was safe: No serious adverse events occurred, and any mild-to-moderate adverse events were transient.
The findings were disappointing given the lack of approved treatment options other than pain management for acute VOC in hospitalized patients with SCD, and they were somewhat surprising given that preclinical and clinical data in recent years have demonstrated that “you can actually prevent those crises by antiadhesive strategies,” he said.
“So we hypothesized that, if you perform such an antiadhesive strategy in a patient already having a crisis and admitted in the hospital, you may shorten their period of admission and perhaps also shorten the severity of their pain,” he said.
In fact, a single-center, randomized, controlled trial conducted by Qari et al. in 2007 (Thromb Haemost. 2007 Aug;98[2]:392-6) showed that full-dose tinzaparin reduced pain severity and duration of admission among sickle cell patients with acute VOC – perhaps because of the antiadhesive properties of heparin – but that study was never repeated, Dr. Biemond said, noting that those antiadhesive properties have been well documented in animal studies.
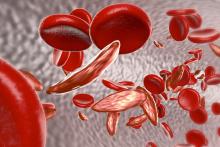
“Heparin is able to inhibit P-selectin, L-selectin, thrombospondin, fibronectin, and von Willebrand activity, which are all involved in vaso-occlusion in patients with sickle cell disease, and very likely also involved during a vaso-occlusive crisis,” he explained, adding that sevuparin, a low-molecular-weight heparin without functional antithrombin binding domain, seemed to be a good candidate for testing that hypothesis.
“It has no anticoagulant effects on factor Xa and IIa,” he said. “It retains, however, its antiadhesive and antiaggregation properties.”
Since it has no anticoagulation activity, it can be dosed at up to 20-fold the therapeutic dose of low-molecular-weight heparin to optimize the antiadhesive effects, he noted.
However, the data indicate that “antiadhesive therapies are clearly not effective in patients with vaso-occlusive crisis,” he said, noting that this was also affirmed by a similar 2019 study of the investigational panselectin inhibitor rivipansel, as reported in a Pfizer press release.
Intriguingly, the difference between the current study and the 2007 study by Qari et al. raises questions about whether anticoagulation, rather than antiadhesion, helped resolve VOC in that study, he said, noting that future studies should focus on whether that is the case.
As for the role of antiadhesive therapy, the mode of action of sevuparin and the current findings taken together suggest that future studies should also assess whether it can be used to prevent VOC.
“Perhaps sevuparin could be administered to patients in a prodromal phase – just before a real vaso-occlusive crisis appears – to prevent such a crisis from happening,” he said. “It would be interesting to use the drug that way.”
Dr. Biemond reported research funding from Sanquin and honoraria from Novartis and GBT.
SOURCE: Biemond B et al. ASH 2019, Abstract 614.