NATIONAL HARBOR, MD – Seeing is believing, especially when enhanced visualization of tumors during surgery helps improve chances for complete resection, investigators said at the annual Society of Surgical Oncology Cancer Symposium.
With near-infrared (NIR) fluorescence imaging and a portable camera that can be used in an operating room, surgeons can eliminate some of the guesswork involved in identifying involved surgical margins or lymph nodes, researchers from the U.S. and the Netherlands reported in oral and poster sessions.
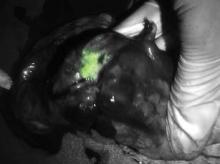
In early human trials, a small, portable infrared camera has been successful at identifying dye-impregnated tumors – including noncontiguous pockets of malignancy – during surgery to resect squamous cell carcinomas and adenocarcinomas of the lung, reported Dr. Sunil Singhal, of the department of surgery at the University of Pennsylvania, Philadelphia.
"Even in this day and age, surgeons leave behind disease in 40% of the cases, and in about a quarter of those cases the tumor was within two centimeters of where the surgeon was working," Dr. Singhal said.
To improve the odds, he and his colleagues have been investigating optical contrast agents that can be delivered safely to tumors and cause them to fluoresce under light in the near-infrared portion of the spectrum. In preclinical studies with dogs, they found that indocyanine green had the right combination of toxicity, photostability, pharmacokinetics, and cost. The dye, currently used in retinal angiography, has an emission profile that makes it easy for observers to discriminate between the fluorescing dye and blood or tissues, Dr. Singhal said.
They also developed an intraoperative device, dubbed the "FloCam," which consists of a light source and near-infrared (NIR) camera that sits above the patient and sends images to a computer monitor showing the operation in NIR.
In animal studies, the system found evidence of residual disease that was not visible to the naked eye or on x-ray microtomography. On pathologic examination, they saw that the dye was "remarkably precise in delineating margins from normal surrounding tissues," particularly in tumors with neovascular features.
Dr. Singhal said that the imaging technique has been effective at identifying tumor sites during surgery in 36 of 38 patients in early human trials, failing only for 1 patient with melanoma, and for 1 with a sarcoma.
One patient was a 64-year-old nonsmoking man who presented with a cough and was found to have a 2.5 cm right upper lobe lung tumor. Evaluation of the mediastinum with imaging and pathology samples was negative for malignancy, but during surgery, the dye highlighted previously undetected tumor hotspots in the right lower lobe.
"This is another patient who would have gone home [with a diagnosis of] stage 1A. I would have walked down to the recovery room, say ‘I cured you,’ and he would come back 1 year later with metastatic disease and die. This patient, who had minimal disease when we discovered it, got chemotherapy and is still alive at the 1-year mark," Dr. Singhal said.
Green hybrid
In a separate study, investigators in the Netherlands reported on improved intraoperative sentinel node identification and harvesting using a novel hybrid radiopharmaceutical tracer combining indocyanine green with technetium-99m in a nanocolloid suspension.
They found that in 96 patients with malignant melanomas of the head and neck, trunk, or extremities, the hybrid tracer, facilitated both preoperative SPECT/CT imaging and intraoperative radio- and fluorescence-guide sentinel node biopsy in all patients.
"The hybrid tracer was found to be particularly useful for the detection of sentinel nodes in the neck, and for sentinel nodes that failed to accumulate patent blue dye," wrote Dr. Oscar R. Brouwer from the division of nuclear medicine at the Netherlands Cancer Institute in Amsterdam, and colleagues in a scientific poster.
Dr. Singhal’s studies were supported by the Society of Surgical Oncology and the University of Pennsylvania. He reported having no financial disclosures. Dr. Brouwer’s study was supported by the Netherlands Cancer Institute. He reported having no financial disclosures.