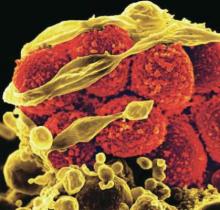
About half of individuals infected with methicillin-resistant Staphylococcus aureus report feeling stigmatized in interactions with hospital staff, data from a survey of 61 adult patients show.
“Hospital care for people who carry MRSA calls for a dedicated and patient-centered approach in both the way the care is delivered ... as well as the way the care is organized at the institutional level,” wrote Babette Rump, MD, of the Regional Health Service Utrecht region, Zeist, the Netherlands, and her coauthors (J Hosp Infect. 2016. doi: 10.1016/j.jhin.2016.09.010). “Prevention of unnecessary intrusive measures, while as the same time applying appropriate precautionary measures, is key to successful and respectful MRSA management.”
Dr. Rump and her associates set out to identify and quantify stigma tied to MRSA and “explore its association with mental health within a country with a MRSA ‘search and destroy’ policy.” In the Netherlands and Scandinavian countries, this policy includes isolating MRSA carriers, wearing personal protective equipment, and disinfecting the room after patients are discharged (Antimicrob Resist Infect Control. 2014 Jan 15;3[1]3). The U.S. Centers for Disease Control and Prevention, in its 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings, recommends similar methods, including application of infection control precautions during patient care and environmental measures, such as cleaning and disinfection of the patient care environment and dedicated single-patient use of noncritical equipment.
In the current study, 60-item questionnaires were provided to all adult patients at two hospitals and two regional health services who had acquired MRSA between Oct. 1, 2013, and April 1, 2014. Stigma was assessed using the 40-item Berger HIV Stigma Scale, reported Dr. Rump.
Overall, 56% of survey respondents reported stigma, including 14% who reported clear stigma and 42% who reported suggestive stigma. The remaining 44% reported no stigma. A total of 80% of the patients received MRSA eradication treatment, which was strongly associated with higher stigma, the researchers noted.
Written comments provided by 40 patients (68%) along with the questionnaires “offer valuable insights to set the focus for improvement,” the researchers said.
The most frequent comments involved patients’ perceived organizational problems with the hospital (8 patients), lack of staff knowledge (4 patients), as well as little attention paid to patient perspectives (4 patients) and unnecessarily intrusive treatments (3 patients). Also of note, 5 patients blamed and 2 “shamed” the hospital as their source of MRSA.
The results were limited by several factors, including the small study size, the researchers wrote. However, the findings suggest that “a substantial proportion of people that carry MRSA experience signs of stigma and that anticipation on MRSA-associated stigma is warranted,” they said.
The researchers had no financial conflicts to disclose.