A counseling and shared decision-making visit improved patient knowledge of the eligibility criteria, benefits, and potential risks of lung cancer screening via a low-radiation chest CT scan.
The Center for Medicare & Medicaid Services has added the type of visit addressed in this study to Medicare’s preventive services benefits for individuals meeting certain criteria, but no previous study had looked at how the implementation of such a visit impacted a patient’s knowledge and understanding.
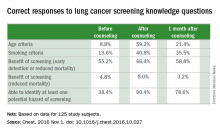
Subjects in this study were initially quizzed for knowledge about screening criteria, hazards, and benefits, and then underwent the counseling program. They were tested again immediately after the session, and then 1 month later.The researchers noted significant improvement in all questions before and after a counseling session (P = .03 to P less than .0001). Those improvements lessened at 1 month, but were still higher than precounseling scores.
The percentages of participants who knew the age criteria for lung cancer screening before counseling, immediately after counseling, and 1 month after counseling, for example, were 8.8% (11 patients), 59.2% (74 patients), and 21.4% (24 patients), respectively. The percentage of participants able to identify at least one of the potential hazards of screening increased by a similar amount immediately after receiving counseling, as did the percentage of participants able to identify the age criteria for lung cancer screening immediately after receiving counseling. The percentages of patients able to identify at least one of the potential hazards of screening were 38.4% before counseling and 90.4% immediately after receiving counseling. One month following counseling, the percentage of patients with such knowledge remained fairly high, dropping to 78.6%.
“Showing the value of these visits is very important to encourage policymakers and payers to continue to support the counseling and shared decision-making visit,” Peter J. Mazzone, MD, MPH, who led the study, said in an interview.
These types of conversations are important because of the uncertainties surrounding lung cancer screening, which leads to about a 20% reduction in mortality risk. That translates to the need to screen about 250 people to save 1 life. “I think the public sometimes doesn’t realize that the effectiveness of some of these preventive screenings may not be as large as they think they are,” said David Grossman, vice chair of the US Preventive Services Task Force and a senior investigator at the Group Health Research Institute, Seattle, who was not involved in the study.
The researchers developed a centralized counseling and shared decision-making visit that included a narrated slide show and individualized risk assessment. They approached 423 consecutive patients who had been identified by their primary care provider or a specialist as potential candidates for screening. Of those 423 patients, 125 agreed to participate in the study (Chest. 2016 Nov 1. doi: 10.1016/j.chest.2016.10.027).
The session delivered expected improvements in patient knowledge, but there were some surprises. “The starting point of knowledge was perhaps less than we would have anticipated, and the gains, though very substantial, weren’t perfect,” said Dr. Mazzone, who is also director of the lung cancer screening program at the Cleveland Clinic.
The drop in knowledge at 1 month suggests that the information needs to be reinforced, possibly each time patients come in for an annual screening visit, Dr. Mazzone added.
Counseling sessions can also help convince patients to quit smoking, if tobacco use is a concern. “It’s not appropriate to screen for lung cancer without making a commitment to try to quit,” said Dr. Grossman.
No funding source was disclosed. Dr. Mazzone and Dr. Grossman reported having no financial disclosures.