SEATTLE – In a phase II trial, an antibody that targets domain 1 of the CD4 receptor maintained viral suppression among patients who had been taking combination antiretroviral therapy (cART). The study lasted up to 16 weeks, and no viral rebound was seen.
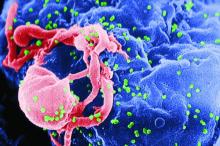
In vitro studies showed that UB-421 can neutralize more than 850 strains of HIV-1, and it binds to the CD4 receptor with an affinity about 100 times greater than that of the gp120, essentially outcompeting the virus for access to T cells.
Most broadly neutralizing antibodies, which target the gp120 protein on the HIV virus, tend to allow viral breakthrough from the development of resistance. “Based on previous studies, in every viral isolate, we get 100% neutralization,” said Dr Liao.
The study included 29 males who had successfully suppressed viral loads on cART. They were assigned to cohort 1 (10 mg/kg weekly, 8-week interruption) or cohort 2 (25 mg/kg weekly, biweekly, 16-week interruption). 27 patients completed all doses.
After the interruption period, 22 of 27 patients who completed treatment restarted cART. There were no viral rebounds during the treatment periods or during the follow-up period among those who restarted cART. The five patients who discontinued cART experienced viral rebound, but all then restarted cART and achieved viral suppression.
During the periods of UB-421 therapy, proviral DNA count dropped (P = .014), suggesting that the antibody may deplete the HIV-1 reservoir and has potential to be curative.
There was no difference in CD4+ T-cell counts before treatment and after the study ended. That’s important, says Dr. Liao, because some researchers expressed concern that blocking CD4 could lead to immunosuppression.
Regulatory T-cell numbers dropped during UB-421 therapy (interquartile range 1.7-3.1; P less than .01), potentially boosting immunity. “Besides being an entry inhibitor, there is also a lot of immunomodulatory activity,” said Dr Liao.
She also believes that the injecting the drug is more convenient than taking daily oral medications, and in fact, some patients refused to go back to cART at the end of the trial, requesting ongoing therapy with UB-421 instead. The company also is working on intramuscular and subcutaneous formulations that could be dosed monthly.
The company is planning a phase III trial in Taiwan and plans to file an IND in the United States soon, she added.