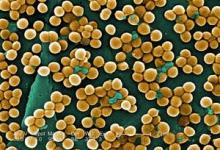
PASADENA, CALIF. – Clinicians should assume community-acquired skin and soft tissue infections are due to methicillin-resistant Staphylococcus aureus infection unless proved otherwise, according to Dr. Paul D. Holtom.
For years, most hospital-associated S. aureus infections have been resistant to methicillin, and now the same has been found for community-acquired S. aureus in studies done mostly in adults, Dr. Holtom of the University of Southern California, Los Angeles, said at the meeting.
At his institution, he said, 70% of people presenting to the emergency department with skin and soft tissue infections have community-acquired MRSA. And a multistate study of 422 patients seen in EDs for skin and soft tissue infections found MRSA in 59%, with rates ranging from 32% to 74% in various states, except for an inexplicably low outlier rate of 15% in New York (N. Engl. J. Med. 2006;355:666-74).
Enough risk factors have been identified for community-acquired MRSA that "you might say that almost everyone is now at risk," he said. Risk factors include intravenous drug use, men having sex with men, residence in correctional institutions, being homeless or marginally housed, various athletic sports, and postinfluenza pneumonia.
A study of 812 U.S. soldiers found that 28% had nasal colonization of methicillin-susceptible S. aureus (MSSA) and 3% had MRSA in their nares. Those colonized with MRSA, however, were significantly more likely to develop soft tissue infection – 9 of 24 soldiers (38%), compared with infections in 8 of 229 soldiers (3%) with MSSA colonization (Clin. Infect. Dis. 2004;39:971-9).
After a "very serious outbreak" of MRSA infections in 928 of 165,000 inmates in the Los Angeles County Jail in 2002, 66 inmates were hospitalized, most with skin and soft tissue infections, and 10 had invasive disease. Subsequent implementation of preventive measures was ineffective, Dr. Holtom said. The number of MRSA infections increased to 1,849 in 2003 and 2,480 in 2004. "It’s not only being spread in the jail, but it’s being brought in. It is throughout the community," he said.
There have been many reports of MRSA infections being spread among competitive athletes, including wrestlers, fencers, and collegiate football players. "This has continued to be a problem. It’s not only collegiate teams but now has moved to high school teams as well," Dr. Holtom said.
Assume that skin and soft tissue infections are due to MRSA, he advised, and get culture and sensitivity testing if you want to understand the epidemiology in your area. When appropriate, treat with surgical drainage of the infection site. Studies suggest that adding antibiotics for patients treated with irrigation and drainage does not improve rates of healing but may help the abscesses heal faster, he said.
When treating suspected S. aureus infection with empiric antibiotics, choose carefully, he added. The infection most likely is due to MRSA, so drugs like cephalexin and dicloxacillin probably will not be effective.
"The good news is that unlike hospital-associated MRSA, community-associated MRSA is frequently sensitive to multiple old-fashioned, inexpensive drugs," including trimethoprim/sulfamethoxazole (TMP/SMX), tetracyclines, or clindamycin, Dr. Holtom said.
TMP/SMX is not very active against Streptococcus pyogenes, the other most likely cause of skin and soft tissue infections and abscesses, so many clinicians combine TMP/SMX with rifampin for synergistic activity against S. aureus and activity against S. pyogenes. Others use TMP/SMX and cephalexin, he said.
The tetracycline drugs doxycycline and minocycline are active against S. aureus. Clindamycin also is a popular choice, but rates of resistance are increasing. At Dr. Holtom’s institution, he said, 8%-10% of S. aureus infections are now resistant to clindamycin.
Dr. Holtom reported having no disclosures or conflicts of interest.