and 1 in 10 said it was serious enough to make them consider leaving medicine.
Yet, responses to the Medscape Family Medicine Physician Lifestyle, Happiness & Burnout Report 2021 also indicate that family physicians are in the middle of the pack again this year in rankings by specialty of physician happiness outside work. Overall, more than 12,000 physicians from more than 29 specialties responded to this year’s survey, conducted between Aug. 30 and Nov. 5, 2020.
Happiness levels sink for physicians
In light of the COVID-19 pandemic, happiness levels took a sharp drop among physicians across the board. Last year, for instance, the happiness level was highest for physicians practicing in diabetes and endocrinology, at 89%. They remain the happiest this year, but the proportion saying they were happy dropped to 73%. Infectious disease physicians were the least happy outside work both last year and this year, with the proportion reporting they were happy dropping from 69% to 45%.
For family physicians, happiness levels outside work plunged from 79% last year to 57% this year.
Burnout and depression levels, however, remained steady. The portion saying they were either burned out or burned out and depressed was up only 1 percentage point, rising to 47%.
Fifteen percent of family physicians have had thoughts of suicide, and 1% said they had attempted it, according to the survey responses.
The most common strategy for coping with burnout, reported by 48% of family physicians, is talking with family members and close friends, followed closely by exercise, reported by 46%.
Sixty-eight percent of family physicians say they exercise at least twice a week, and 12% exercise every day.
However, not all coping strategies were as positive: Forty-five percent said they cope by isolating themselves from others; 40% turned to junk food; and 23%-24% said they drank alcohol or were binge-eating to cope. Respondents could choose more than one answer.
Among family physicians, 75% expressed anxiety about their futures, given the pandemic, which is similar to the proportion among physicians overall (77%) who had the same worries.
Work-life balance biggest worry
The survey also asked what workplace issues concern family physicians the most. The biggest concern, by far, was work-life balance, chosen by 51%. Next highest was compensation, at 19%, followed by combining parenthood and work (9%) and relationships with colleagues/staff (6%).
More than half (52%) of family doctors said they would take a cut in pay to have better work-life balance.
A little more than a third (36%) of family physicians – about the same percentage as physicians overall – said they always or most of the time spend enough time on their own health and wellness. One in five said they rarely or never do.
The amount of work required beyond the bedside continues to frustrate family physicians.
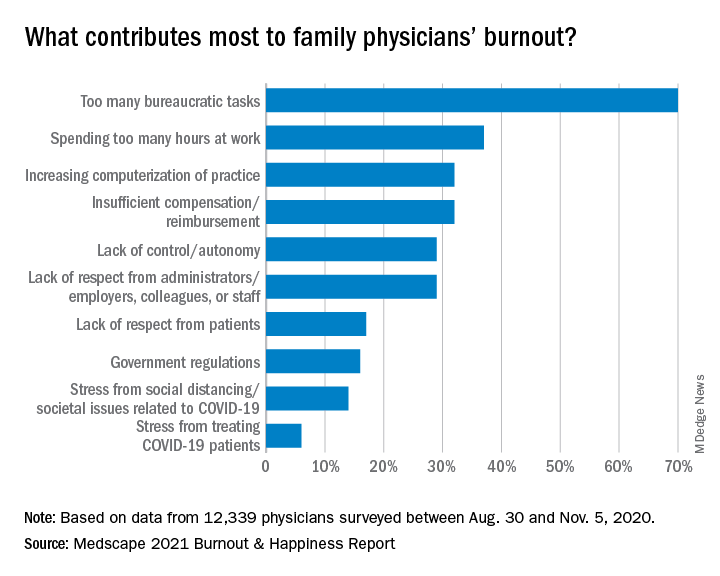
Again this year, the top cause of burnout, chosen by 70% of family physicians, was “too many bureaucratic tasks.” That was followed by “spending too many hours at work” (37%) and “increasing computerization of practice” (32%).
A large majority (82%) of family doctors report that they work online up to 10 hours a week, a number that could increase with the rise of telemedicine; 64% are personally online up to 10 hours a week. But even with combined personal and professional Internet time, family doctors don’t come close to the average time spent online among all Internet users, which Hootsuite and We Are Social report is an average of 7 hours per day.