Closing the GAP in Idiopathic Pulmonary Fibrosis
Humayun Anjum, MD, FCCP
Medical Director, Department of Pulmonary and Critical Care Services
Baylor Scott & White Medical Center
Grapevine, TX
Dr. Anjum has disclosed no relevant financial relationships.

IPF, the most prevalent ILD and one of unknown etiology, affects up to 207,000 Americans and up to 58,000 new patients each year.1 Prognosis is poor; median survival estimates have ranged between 2 and 5 years for the last decade.2,3 Although IPF is not curable, initiating a treatment plan as early as possible is critical to managing symptoms and slowing disease progression.4
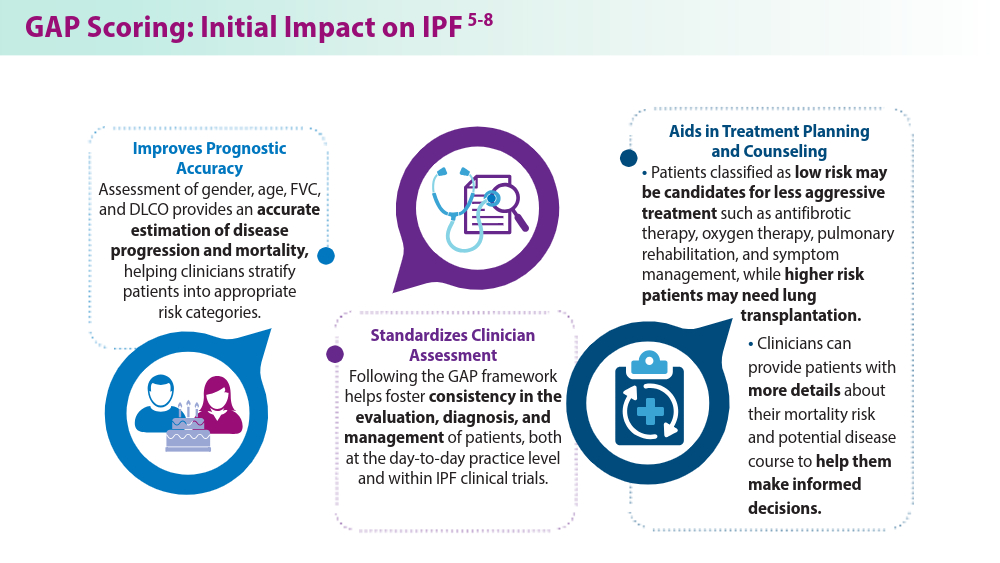
Introduced in 2012, the GAP (gender, age, physiology) prognostic model offers clinicians a framework for assessing mortality risk, with the goal of improving IPF outcomes.5 The GAP model uses a standardized approach to staging patients while also aiding clinicians in tailoring each patient’s treatment approach.5-8 The “physiology” component evaluates forced vital capacity (FVC) to assess lung function and diffusing capacity of the lungs for carbon monoxide (DLCO) to measure gas exchange effciency.
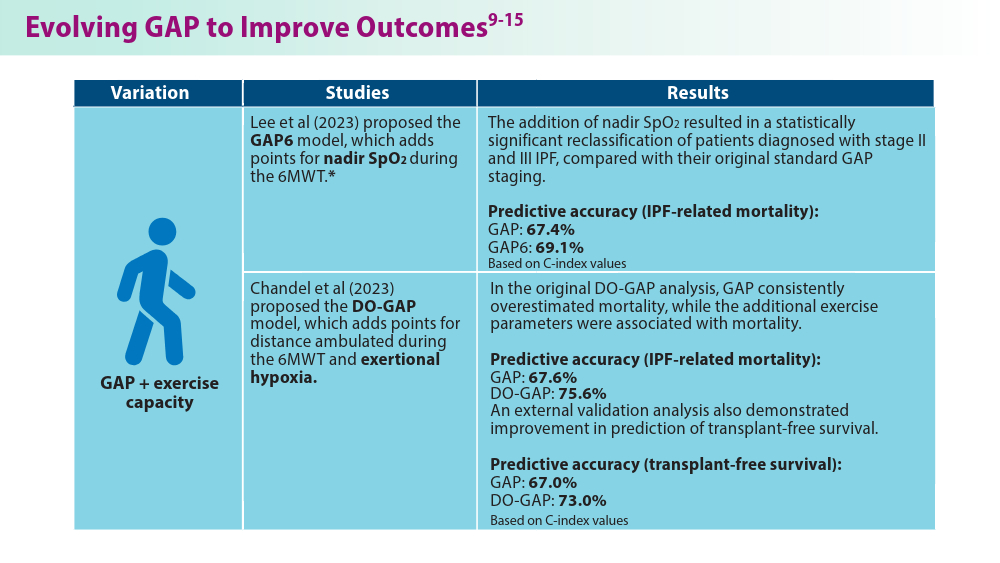
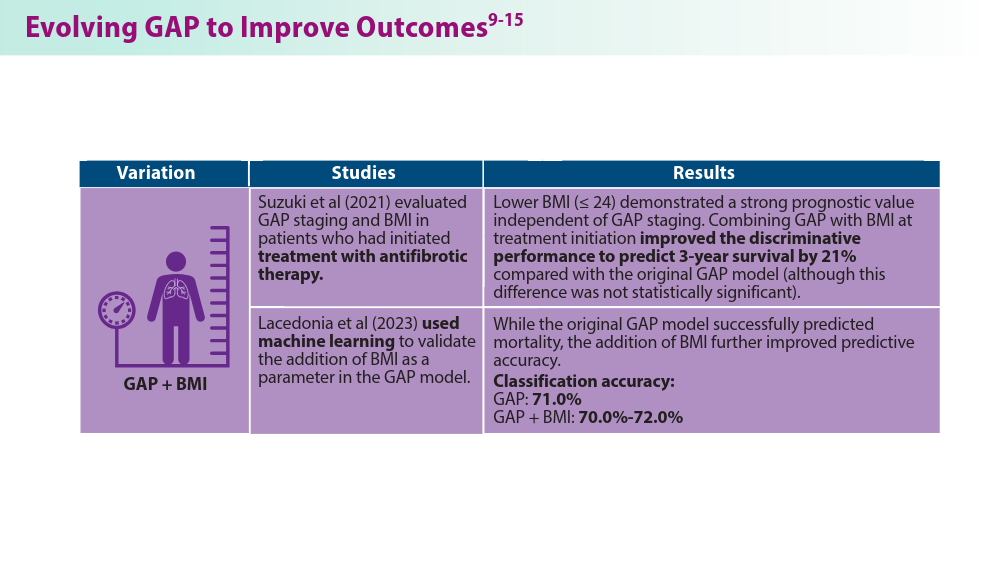
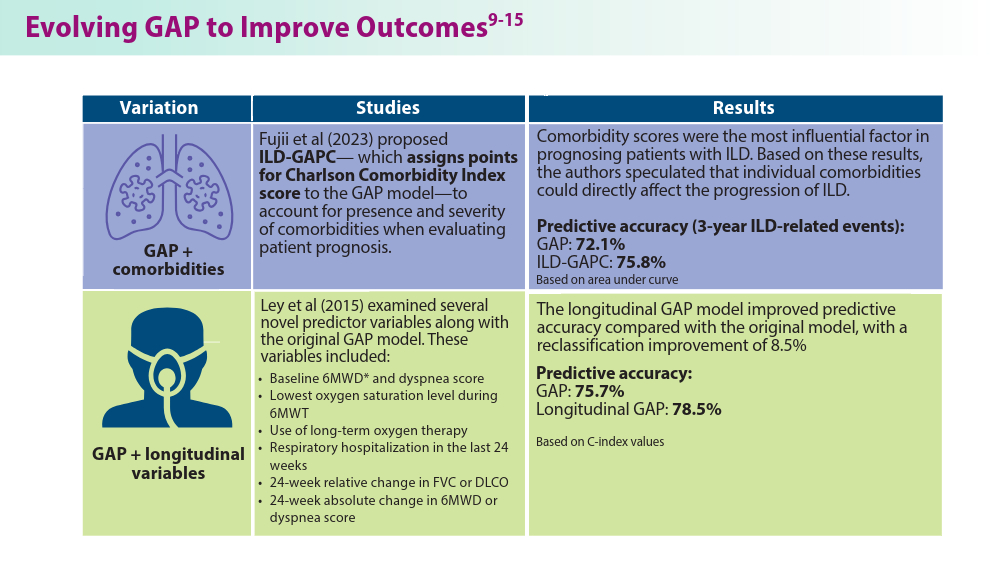
While the integration of FVC and DLCO into the GAP model provided a more comprehensive assessment at the time of its introduction, our understanding of IPF has evolved over the last decade. There has been a recent surge in proposed modications to the original GAP model. Studies have examined the integration of additional criteria, such as comorbidities, body mass index (BMI), exercise capacity, and other factors, into the GAP model to help to improve predictive precision.9-15 The incorporation of additional parameters and biological markers offers promising prospects for more accurate prognostications and personalized treatment strategies. Although these proposed enhancements to the GAP model require further validation, their potential to refine treatment personalization makes them worthy of careful consideration.
1