Severe Community-Acquired Pneumonia: Diagnostic Criteria, Treatment, and COVID-19
Sujith V. Cherian, MD, FCCP
Associate Professor, Divisions of Critical Care
Pulmonary and Sleep Medicine, Department of Internal Medicine
Director of Interventional Pulmonology and Pleural Diseases
Lyndon B Johnson Hospital
Department of Pulmonary Medicine
University of Texas Health-McGovern Medical School
Houston, TX
Dr. Cherian has disclosed the following relevant financial relationships:
Received income in an amount equal to or greater than $250 from: Taylor and Francis
Receive royalties for published book from: Taylor and Francis publishers

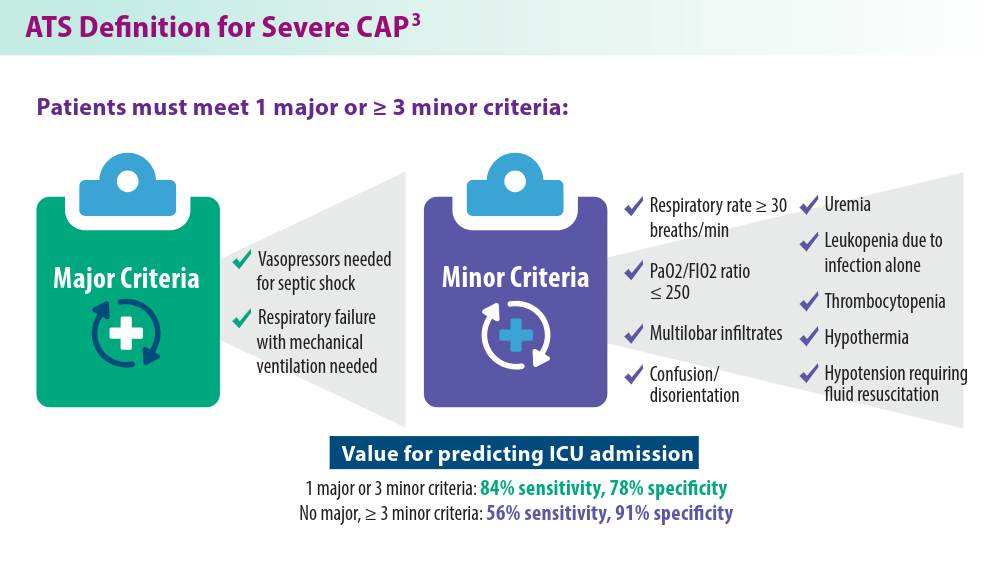
Pneumonia, a common respiratory infection, can be categorized as community-acquired or hospital-acquired pneumonia, which includes ventilator-associated pneumonia.1 Severe community-acquired pneumonia (CAP) poses unique challenges for clinicians, with high mortality and risk for long-term complications.1,2 Severe CAP is defined by the American Thoracic Society (ATS) guidelines as having 1 major criterion of septic shock needing vasopressors or the requirement of mechanical ventilation, or meeting 3 or more minor criteria based on respiration, hemodynamics, and other clinical characteristics.3 Another well-known tool for defining severe CAP is SMART-COP, which includes measures of systolic blood pressure, multilobar infiltrates, albumin, respiratory rate, tachycardia, confusion, oxygen, and pH for determining severity.4
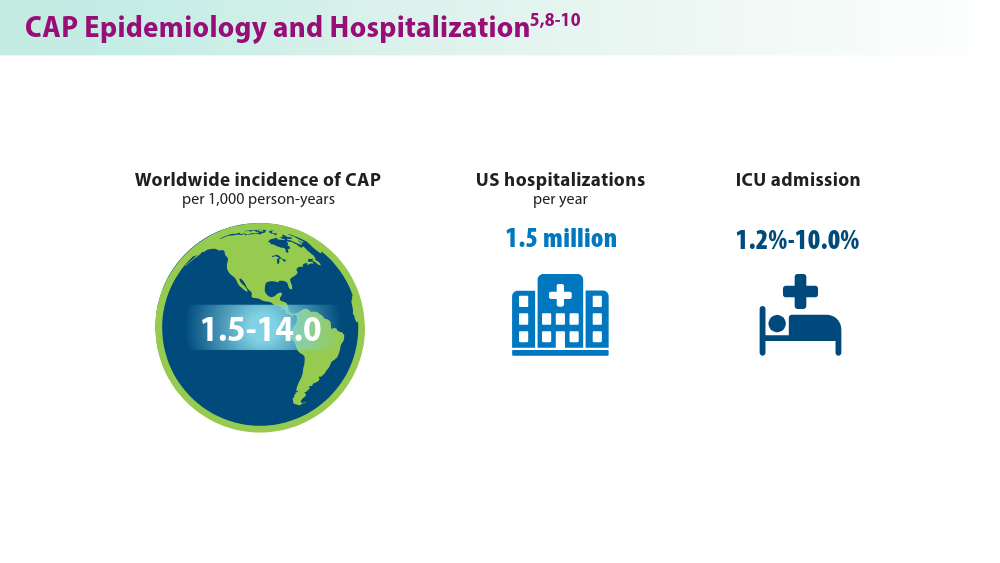
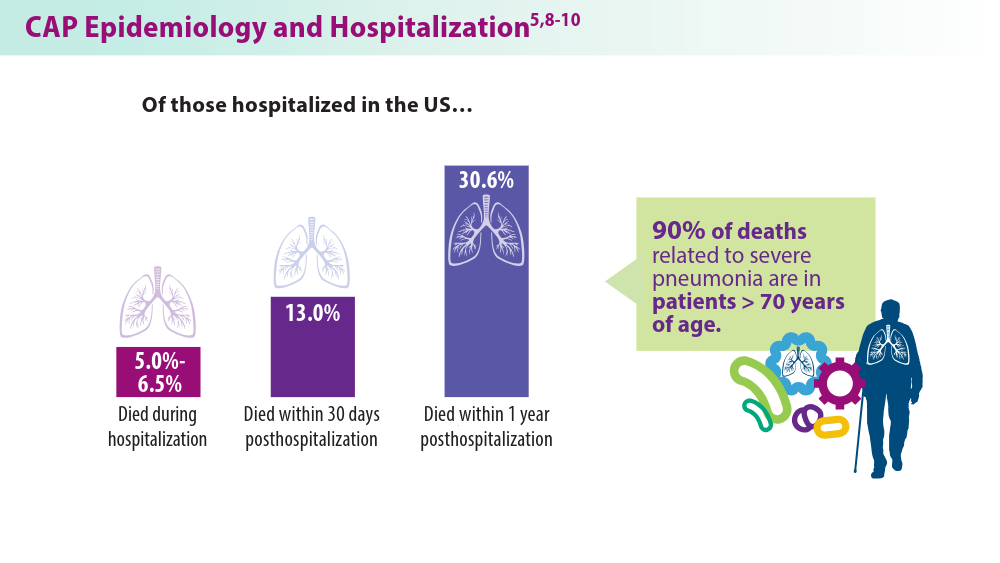
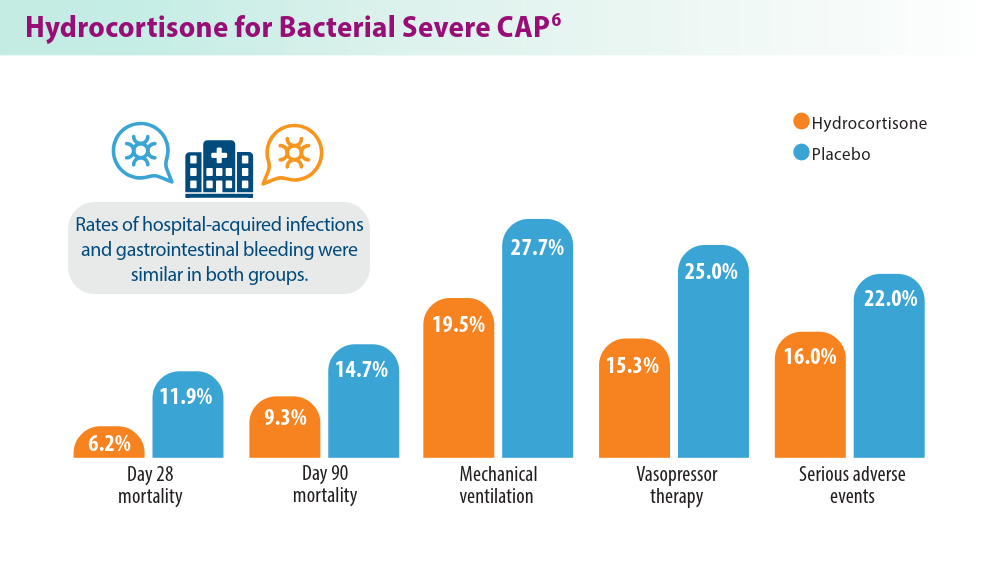
Mortality for severe CAP can be as high as 23%, with 24% of patients requiring invasive mechanical ventilation and 20% requiring noninvasive ventilation.2,5 Advances in treatment, along with antibiotics as the current standard of care, are helping to decrease mortality. Corticosteroids, such as hydrocortisone, have also been shown to decrease mortality in bacterial severe CAP when combined with antibiotics.6
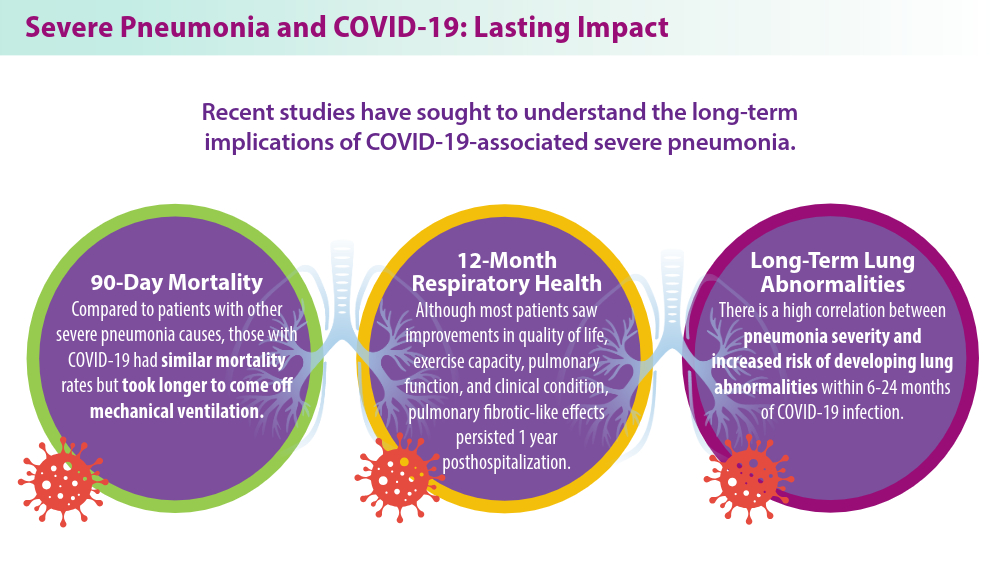
The COVID-19 pandemic complicated the field of severe pneumonia.7 COVID-19-related severe pneumonia has been linked to long-term lung abnormalities, such as decreased lung function, and symptoms such as dyspnea, with other implications still being investigated.7 Severe pneumonia poses a burden to the health care community, but new treatments are helping to combat high mortality and prevent worsening long-term outcomes. Research is needed into other corticosteroids that could help lessen this burden.
1