Dr. Daniel Strbian of the University of Helsinki presented a second score, dubbed SEDAN. Dr. Strbian and his colleagues developed their score based on a cohort of 972 ischemic stroke patients who developed an imaging-proven brain bleed after IV TPA treatment.
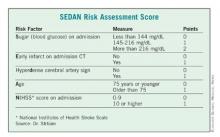
In a multivariate analysis, he and his associates found five factors that were independently associated with a significantly increased risk of symptomatic ICH: blood glucose level on admission, computed tomography (CT) imaging positive for ischemic stroke, cerebral artery hyperdensity, age, and NIHSS score.
Points were assigned based on the relative risk (RR) associated with each factor – the higher the total score, the greater the risk of symptomatic ICH. Each of the five risk-point categories generated a significant risk ratio:1 point, RR 0.19; 2 points, RR 0.40; 3 points, RR 1.85; 4 points, RR 3.7; 5 points, RR 5.6.
The score was validated in two additional groups totaling about 2,000 patients, resulting in an overall accuracy of about 77%.
"If we have a patient with a very high score, there is a very bad prognosis with a high chance of death or institutionalization at 3 months," Dr. Strbian said. "In this case, we know that the patient may die if we do nothing, but perhaps the SEDAN [score] can help us determine if an endovascular approach might be better than thrombolysis."
The SEDAN score is simple, easy, and quick to calculate, he said. But it’s only part of the treatment decision process.
"We can’t treat based on this score alone. If the patient fulfills the indications for TPA, it’s up to the physician and the patient to decide whether they are willing to accept the risk of an intracranial hemorrhage."
Dr. Menon and Dr. Strbian reported having no financial conflicts.