KEYSTONE, COLO. – Six novel phenotypes have been defined that can be used to personalize therapy for difficult-to-treat, refractory asthma.
"There’s no doubt in my mind now, we need to identify the exact phenotype, so as to treat [refractory asthma] with personalized, directed therapy," Dr. Richard J. Martin said at an allergy and pulmonary diseases meeting. "This will improve asthma control and lung function."
Bronchoscopic evaluation of the upper and lower airways as well as reflux studies were used to identify the phenotypes, and prompted the researchers to develop a supraglottic index to visually score abnormalities in the upper airway.
"We think this is superior to any GI study for reflux," said Dr. Martin, chair of medicine and the Edelstein chair of pulmonary medicine at National Jewish Health in Denver, which sponsored the meeting. "So many GI studies are falsely negative because they provide only a snapshot in time, whereas the supraglottic index really shows you a history over a long period of time."
The supraglottic index (SGI) uses a scale to score for the presence of edema and erythema/hyperemia in the epiglottis, false vocal cords, and arytenoid cartilage, as well as secretions or mucosal thickening of the piriform recess and posterior commissure. A total score of 0-4 is normal, 5-9 is mild pathology, 10-16 is moderate, and 17-22 is severe pathology. A score of 10 or more is an important clue for clinicians because it is indicative of reflux that is high enough to produce aspiration or to hit the vocal cords.
The SGI was used in 58 patients who met American Thoracic Society criteria for refractory asthma and who had a 12% improvement after bronchial dilation or PC20 (the provocative concentration of methacholine inducing a 20% fall in FEV1 [forced expiratory volume in 1 second]) of 6 mg/mL or less. Patients with more than a 5 pack-years of smoking were excluded.
Notably, 20 patients initially received guideline-based evaluation and treatment with intensified therapy for 4 months, followed by bronchoscopy-directed therapy, and 38 went directly to bronchoscopy.
The cohort’s mean age was 55 years and the mean FEV1 was 60.7%, even on medication. They had very poorly controlled asthma and severe airway hyperresponsiveness, as indicated by a mean asthma control test (ACT) score of 11.5 and a mean PC20 of 1.6 mg/mL.
Based on bronchoscopic evaluation, five mutually exclusive phenotypes emerged: tissue eosinophilia in 4 patients, subacute bacterial infection in 13, gastroesophageal reflux in 22, combination (any two or all three of the above) in 13, and "nonspecific" in 6. A sixth phenotype (tissue mast cells) has since been identified and can be effectively treated with something as simple as cromolyn, Dr. Martin said.
In all, 44 of the 58 patients (76%) had an SGI of 10 or more. Of these, 43 also had reflux testing, and 34 had documented gastroesophageal reflux disease (GERD). Some 14 patients (24%) had an SGI less than 10, with 8 of the 9 patients who also underwent reflux testing being negative for GERD.
Patients with a positive GERD test had a significantly higher mean SGI score than did those with a negative GERD test (15.8 vs. 8.9; P less than .0001), he said, but later noted that bronchoscopists were blinded to some – but not all – of the reflux test results.
When the investigators looked at treatment outcomes, they found "absolutely no change" in FEV1 or ACT scores after 4 months of intensified, guideline-directed standard therapy in the 20 control patients. In contrast, after bronchoscopic-directed therapy, ACT improved almost into the well-controlled range, and FEV1 increased from 64% of predicted to 76% of predicted, Dr. Martin said.
"So this internal control group shows us we really have to phenotype and direct asthma therapy," he said.
 Courtesy Dr. Richard J. Martin and Dr. James T. Good
Courtesy Dr. Richard J. Martin and Dr. James T. Good
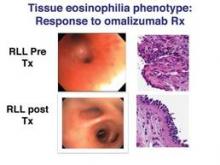
Visualization of the right lower lobe and middle lobe is demonstrated before and after six month of treatment with omalizumab. Prior to treatment, there is marker narrowing of the airways due to edema as well as areas of hyperemia and bleeding. This is resolved with treatment. The histologic pictures demonstrate marked inflammation and epithelial sloughing before treatment which is resolved with therapy.
Among the 38 patients who went directly to bronchoscopic-directed evaluation and therapy, significant increases in ACT and FEV1 were observed 6 months post treatment among all but the nonspecific phenotype. Dr. Martin pointed out that patients in the tissue eosinophilia group experienced "tremendous improvement" in FEV1 with the use of omalizumab (Xolair), whereas no benefit was seen in the nonspecific group.

