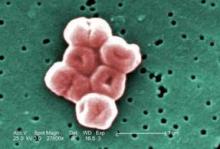
After terminal cleaning of ICU rooms that were contaminated with the multidrug-resistant Acinetobacter baumannii, half the rooms still contained the pathogen, primarily on the floor, bedside tables, call buttons, door handles, and a supply cart, according to a study published in the December issue of American Journal of Infection Control.
Even rooms of patients who had not had a culture test positive for A. baumannii in more than a month had samples test positive for the bacterium, "suggesting a potential longevity of contamination on surfaces in patient rooms," Paula Strassle and her associates at the University of Maryland, Baltimore, reported (Am. J. Infect. Control 2012;40:1005-7).
At the University of Maryland Medical Center, investigators collected 487 cultures from 32 medical, surgery, and cardiac surgery ICU rooms of patients who had a known infection or history of colonization with strains of A. baumannii that are resistant to at least two classes of antibiotics. Between March 2009 and April 2011, the samples were collected when a patient was scheduled to be discharged and then after terminal cleaning by hospital environmental services staff before a new patient was admitted.
The cleaning staff, who were not aware of the study, removed curtains, infusion pumps, and respiratory equipment from the rooms and cleaned rooms from the top down using Virex II 256 wipes and mopping from back to front with an 8- to 10-minute dwell time.
The team collected samples from the rooms’ sink drains, edges of basins, bed rail buttons, bedside table handles, vital sign monitor buttons, call buttons/remotes, supply cart drawer handles, door handles (interior and exterior), infusion pump buttons, ventilator machine buttons, and floor around the beds.
Before cleaning, 15 of the 32 rooms (46.9%) and 41 of the 268 swabbed sites (15.3%) were found positive for the pathogen. The sites with the highest rates of contamination before cleaning included the floor (12/32, 37.5%); supply carts (7/30, 23.3%); bed rails (5/24, 20.8%); and ventilators (3/15, 20%).
After cleaning, 8 of the 32 rooms (25%, all of which had been contaminated before cleaning) and 12 of the 219 swabbed sites (5.5%) tested positive for A. baumannii. The contaminated sites included the floor (4/32, 12.5%); the bedside table (2/27, 7.4%); the call buttons (2/20, 10%); the door handles (3/32, 9.4%); and a supply cart (1/26, 3.8%).
The fact that half of the originally contaminated rooms had persistent contamination after cleaning led the researchers to conclude that current cleaning techniques may be inadequate to fully remove this pathogen. Noting the stronger effectiveness of methods such as hydrogen peroxide vapor and ultraviolet light, the authors acknowledged these methods may be difficult to implement because of the extra time involved with their use.
The authors also acknowledged that their study was limited because the cleaning staff were not observed, which meant that possibly poor cleaning techniques that could be improved with better communication with and training of cleaning staffs were not observed. The A. baumannii samples were not compared using molecular typing, so the researchers also could not unequivocally state that the post- and precleaning contamination was with identical strains within each room.
The study was funded by the National Institutes of Health. The authors said they had no relevant financial disclosures.