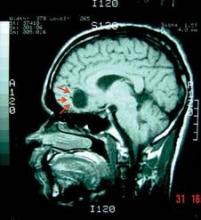
A new evidence-based guideline for both adults and children who have neurocysticercosis – tapeworm larvae seeded in the brain parenchyma – suggests that clinicians should consider treating with albendazole plus either dexamethasone or prednisolone.
It is hoped that the combination of the cysticidal drug albendazole and a corticosteroid will reduce both the number of active brain lesions and the frequency of the seizures they cause, according to lead author Dr. Ruth Ann Baird and her associates on the American Academy of Neurology’s guideline development subcommittee.
 Courtesy Dr. Daniel Ciampi de Andrade
Courtesy Dr. Daniel Ciampi de Andrade
It is hoped that the combination of albendazole and a corticosteroid will reduce both the number of active brain lesions and the frequency of the seizures they cause, according to Dr. Ruth Ann Baird and her associates on the American Academy of Neurology’s guideline development subcommittee.
The optimal treatment for neurocysticercosis has been controversial, with experts debating the usefulness and potential dangers of cysticidal therapy, steroid therapy, and antiepileptic therapy. Dr. Baird of the department of clinical neurology at Indiana University, Indianapolis, and her colleagues performed a systematic review of the English- and Spanish-language medical literature to clarify the issue (Neurology 2013;80:1424-9).
Unfortunately, even a close review of the best 123 articles available did little to resolve the controversy. The studies used widely varying methodologies and different criteria for judging improvement on brain imaging, making comparisons and pooling of the data difficult. Also, the quality of the data in most of the available studies was suboptimal.
The committee, however, was able to reach some conclusions.
"Based on imaging findings in four Class I studies (three concordant, one underpowered study failing to show an effect) and a meta-analysis of two Class I and four Class II studies, albendazole (400 mg b.i.d. for adults or weight-based dosing for either adults or children) is probably safe and effective in reducing both the number of cysts and long-term seizure frequency," they said.
"In most studies, corticosteroids were coadministered, in varying dosages, and this combination appears effective [but] the evidence is insufficient to support or refute the use of steroid treatment alone in patients with intraparenchymal neurocysticercosis," the committee noted.
There also was no evidence on which to base a recommendation regarding optimal timing of steroid therapy, the committee added.
The AAN-sponsored guideline is also endorsed by the American Epilepsy Society.
Historically, the side effect of greatest concern in such cases has been large-scale parasite death induced by antihelminthic agents like albendazole, but this danger was emphasized in only a single study, in which the data are now considered to be only of class-IV quality.
Smaller but better-quality studies have since shown no increase in seizure frequency or other adverse effects with use of albendazole. All such studies, however, excluded patients who had massive cerebral edema or "innumerable" brain lesions, Dr. Baird and her associates noted.
The guideline also stated that, "given the well-established efficacy and safety of a broad range of AEDs [antiepileptic drugs] and the frequency with which neurocysticercosis causes seizures, it is reasonable to treat these patients with AEDs at least until the active lesions have subsided."
The authors concluded the guideline with a call for future researchers to definitively establish whether combination cysticidal and steroid therapy is beneficial, to determine the appropriate use and timing of adjuvant corticosteroids, to address HIV coinfection that can alter the efficacy of antihelminthic drugs or induce significant drug-drug interactions, and to focus on clinical outcomes rather than just brain imaging studies.
The guideline was developed with financial support from the American Academy of Neurology. Dr. Baird reported no financial conflicts of interest. One coauthor reported receiving honoraria from UCB Pharma and another reported formerly serving on a speakers’ bureau for Boehringer Ingelheim.
