User login
ESR1 mutations found prognostic but not predictive in metastatic breast cancer
CHICAGO – Mutation of the estrogen receptor 1 (ESR1) gene, one of the mechanisms whereby tumors become resistant to endocrine therapy, may be prognostic but not predictive in women with hormone receptor–positive advanced breast cancer that has progressed on this therapy, two studies showed.
In a cohort of women who had experienced progression on a first-line aromatase inhibitor, those with ESR1 mutations detected in circulating cell-free DNA at the time of progression had a 70% higher risk of progression-free survival events and a 90% higher risk of death thereafter. But the presence of this mutation did not predict benefit from subsequent therapy.
Similarly, in an analysis of women who had experienced progression on prior endocrine therapy and were treated on the randomized PALOMA-3 trial with fulvestrant plus either palbociclib (a cyclin-dependent kinase inhibitor) or placebo, adding the drug reduced the risk of progression-free survival events similarly, by about 50%, regardless of the presence of ESR1 mutations before starting therapy.
Findings in context
These new findings can help guide decisions about which patients should be tested for ESR1 mutations, according to invited discussant Sarat Chandarlapaty, MD, PhD, a medical oncologist at the Memorial Sloan Kettering Cancer Center in New York.
“Putting it all together … we see ESR1 mutations arise in the metastatic setting subclonally with prolonged exposure to low-estrogen environments,” he said. “If we are going to do testing, it makes sense to do it in the setting in which there is prior exposure to an aromatase inhibitor in metastatic ER-positive breast cancer.”
The studies’ results also help clarify what the finding of an ESR1 mutation means for patient prognosis and choice of next therapy, Dr. Chandarlapaty said at the annual meeting of the American Society of Clinical Oncology.
“It’s clear from two large studies that ESR1 mutation prognosticates poorer and shorter survival, so just the finding alone may aid as sort of a clinical risk assessment for physicians,” he said. “For the question of prediction, I would say the weight of evidence—even though the clinical studies are small—all the way from biology to clinic is that ESR1-mutant patients are unlikely to benefit from a second-line aromatase inhibitor.”
However, “the question of whether testing should be made available in practice on the basis of this particular clinical decision is more complicated,” Dr. Chandarlapaty said. “For one, is second-line aromatase inhibitor alone a widely used option? Secondly, does the adoption now of palbociclib in the first-line setting change the biology and the nature of resistance at this later line – in other words, are we going to see patients going on to a second-line aromatase inhibitor after they’ve had a prior aromatase inhibitor plus palbociclib?”
Mutations after progression on first-line aromatase inhibitors
In the first study, Florian Clatot, MD, PhD, a medical oncologist at the Centre Henri Becquerel, University of Normandy, Rouen, France, and colleagues retrospectively studied 144 women who had experienced progression on a first-line aromatase inhibitor.
The investigators used digital droplet polymerase chain reaction (PCR) testing to screen for four ESR-1 mutations in circulating cell-free DNA collected before, at the time of, and after the progression.
Overall, 30.6% of women were found to have at least one of these mutations at the time of progression, Dr. Clatot reported. The prevalence was higher the longer women had been on the aromatase inhibitor.
After progression, most women went on to receive chemotherapy or alternative endocrine therapy with either the selective estrogen receptor modulator tamoxifen or the estrogen receptor antagonist fulvestrant (Faslodex). With a median follow-up of 40 months, multivariate analyses showed that the group with ESR1 mutations at progression had higher risks of subsequent progression-free survival events (hazard ratio, 1.7; P = .008) and death (hazard ratio, 1.9; P = .002).
However, the mutations were not predictive: Women having one fared more poorly, whether given chemotherapy or given tamoxifen or fulvestrant.
Kinetic analyses showed that 75% of the ESR1 mutations seen at progression were already detectable in the 3 and even 6 months before that event. “Most of the mutations detected before progression increased while aromatase inhibitor therapy was ongoing,” Dr. Clatot commented. “These results suggest that the preclinical detection of ESR1 circulating mutation may [be of] clinical interest.”
Most women who had mutations at progression saw a decrease in the amount detectable over the subsequent 3 months with therapy, including to the point of not being detectable in about half of cases with a reduction. All of those having an increase in mutational burden had progression on their next therapy, compared with only about 40% of those having a decrease in burden.
“Taken together, these results suggest that the selection pressure provided by aromatase inhibitor exposure is one of the main mechanisms of ESR1 mutation increase,” concluded Dr. Clatot. “ESR1 mutations are a strong and independent marker of poor prognosis but do not have any predictive value with the treatments used in our cohort.”
Mutations after progression on prior endocrine therapy
In the second study, Nicholas C. Turner, MD, PhD, a medical oncologist at the Royal Marsden Hospital and Institute of Cancer Research, London, and colleagues analyzed data from a subset of 395 women from PALOMA-3.
The randomized phase III trial tested fulvestrant combined with palbociclib (Ibrance), an oral inhibitor of cyclin-dependent kinases 4 and 6, or placebo. All of the women enrolled had experienced progression on prior endocrine therapy in the adjuvant, advanced, or metastatic setting.
The investigators looked for 12 ESR1 mutations in circulating tumor DNA from baseline plasma samples using the BEAMing (beads, emulsion, amplification, magnetics) digital PCR technique and droplet digital PCR screening.
Overall, 27% of the women had ESR1 mutations before starting therapy on the trial, Dr. Turner reported. Mutations were seen in those who had received a prior aromatase inhibitor, but not in those who had received only prior tamoxifen. “So it’s quite clear these mutations are not a mechanism of resistance to tamoxifen, suggesting that tamoxifen must have at least some activity against these mutations,” he commented.
In addition, ESR1 mutations were more common in patients who had been sensitive versus not to prior endocrine therapy of any type (30.3% vs. 12.8%) and in patients who had been sensitive versus not specifically to prior aromatase inhibitor therapy (34.6% vs. 11.1%).
Stratified analyses showed that palbociclib was similarly superior to placebo in terms of progression-free survival whether patients were positive for an ESR1 mutation (9.4 vs. 4.1 months; hazard ratio, 0.52; P = .0052) or negative (9.5 vs. 3.8 months; hazard ratio, 0.44; P less than .0001).
“Detection of estrogen receptor mutations was strongly associated with acquired resistance to prior aromatase inhibitors,” Dr. Turner said.
“Palbociclib offered high efficacy regardless of the estrogen receptor mutation status,” he added. “And because in this patient population estrogen receptor mutations are detected frequently, the combination of palbociclib and fulvestrant presents an attractive treatment option for patients who have been previously treated with and progressed on aromatase inhibitors.”
CHICAGO – Mutation of the estrogen receptor 1 (ESR1) gene, one of the mechanisms whereby tumors become resistant to endocrine therapy, may be prognostic but not predictive in women with hormone receptor–positive advanced breast cancer that has progressed on this therapy, two studies showed.
In a cohort of women who had experienced progression on a first-line aromatase inhibitor, those with ESR1 mutations detected in circulating cell-free DNA at the time of progression had a 70% higher risk of progression-free survival events and a 90% higher risk of death thereafter. But the presence of this mutation did not predict benefit from subsequent therapy.
Similarly, in an analysis of women who had experienced progression on prior endocrine therapy and were treated on the randomized PALOMA-3 trial with fulvestrant plus either palbociclib (a cyclin-dependent kinase inhibitor) or placebo, adding the drug reduced the risk of progression-free survival events similarly, by about 50%, regardless of the presence of ESR1 mutations before starting therapy.
Findings in context
These new findings can help guide decisions about which patients should be tested for ESR1 mutations, according to invited discussant Sarat Chandarlapaty, MD, PhD, a medical oncologist at the Memorial Sloan Kettering Cancer Center in New York.
“Putting it all together … we see ESR1 mutations arise in the metastatic setting subclonally with prolonged exposure to low-estrogen environments,” he said. “If we are going to do testing, it makes sense to do it in the setting in which there is prior exposure to an aromatase inhibitor in metastatic ER-positive breast cancer.”
The studies’ results also help clarify what the finding of an ESR1 mutation means for patient prognosis and choice of next therapy, Dr. Chandarlapaty said at the annual meeting of the American Society of Clinical Oncology.
“It’s clear from two large studies that ESR1 mutation prognosticates poorer and shorter survival, so just the finding alone may aid as sort of a clinical risk assessment for physicians,” he said. “For the question of prediction, I would say the weight of evidence—even though the clinical studies are small—all the way from biology to clinic is that ESR1-mutant patients are unlikely to benefit from a second-line aromatase inhibitor.”
However, “the question of whether testing should be made available in practice on the basis of this particular clinical decision is more complicated,” Dr. Chandarlapaty said. “For one, is second-line aromatase inhibitor alone a widely used option? Secondly, does the adoption now of palbociclib in the first-line setting change the biology and the nature of resistance at this later line – in other words, are we going to see patients going on to a second-line aromatase inhibitor after they’ve had a prior aromatase inhibitor plus palbociclib?”
Mutations after progression on first-line aromatase inhibitors
In the first study, Florian Clatot, MD, PhD, a medical oncologist at the Centre Henri Becquerel, University of Normandy, Rouen, France, and colleagues retrospectively studied 144 women who had experienced progression on a first-line aromatase inhibitor.
The investigators used digital droplet polymerase chain reaction (PCR) testing to screen for four ESR-1 mutations in circulating cell-free DNA collected before, at the time of, and after the progression.
Overall, 30.6% of women were found to have at least one of these mutations at the time of progression, Dr. Clatot reported. The prevalence was higher the longer women had been on the aromatase inhibitor.
After progression, most women went on to receive chemotherapy or alternative endocrine therapy with either the selective estrogen receptor modulator tamoxifen or the estrogen receptor antagonist fulvestrant (Faslodex). With a median follow-up of 40 months, multivariate analyses showed that the group with ESR1 mutations at progression had higher risks of subsequent progression-free survival events (hazard ratio, 1.7; P = .008) and death (hazard ratio, 1.9; P = .002).
However, the mutations were not predictive: Women having one fared more poorly, whether given chemotherapy or given tamoxifen or fulvestrant.
Kinetic analyses showed that 75% of the ESR1 mutations seen at progression were already detectable in the 3 and even 6 months before that event. “Most of the mutations detected before progression increased while aromatase inhibitor therapy was ongoing,” Dr. Clatot commented. “These results suggest that the preclinical detection of ESR1 circulating mutation may [be of] clinical interest.”
Most women who had mutations at progression saw a decrease in the amount detectable over the subsequent 3 months with therapy, including to the point of not being detectable in about half of cases with a reduction. All of those having an increase in mutational burden had progression on their next therapy, compared with only about 40% of those having a decrease in burden.
“Taken together, these results suggest that the selection pressure provided by aromatase inhibitor exposure is one of the main mechanisms of ESR1 mutation increase,” concluded Dr. Clatot. “ESR1 mutations are a strong and independent marker of poor prognosis but do not have any predictive value with the treatments used in our cohort.”
Mutations after progression on prior endocrine therapy
In the second study, Nicholas C. Turner, MD, PhD, a medical oncologist at the Royal Marsden Hospital and Institute of Cancer Research, London, and colleagues analyzed data from a subset of 395 women from PALOMA-3.
The randomized phase III trial tested fulvestrant combined with palbociclib (Ibrance), an oral inhibitor of cyclin-dependent kinases 4 and 6, or placebo. All of the women enrolled had experienced progression on prior endocrine therapy in the adjuvant, advanced, or metastatic setting.
The investigators looked for 12 ESR1 mutations in circulating tumor DNA from baseline plasma samples using the BEAMing (beads, emulsion, amplification, magnetics) digital PCR technique and droplet digital PCR screening.
Overall, 27% of the women had ESR1 mutations before starting therapy on the trial, Dr. Turner reported. Mutations were seen in those who had received a prior aromatase inhibitor, but not in those who had received only prior tamoxifen. “So it’s quite clear these mutations are not a mechanism of resistance to tamoxifen, suggesting that tamoxifen must have at least some activity against these mutations,” he commented.
In addition, ESR1 mutations were more common in patients who had been sensitive versus not to prior endocrine therapy of any type (30.3% vs. 12.8%) and in patients who had been sensitive versus not specifically to prior aromatase inhibitor therapy (34.6% vs. 11.1%).
Stratified analyses showed that palbociclib was similarly superior to placebo in terms of progression-free survival whether patients were positive for an ESR1 mutation (9.4 vs. 4.1 months; hazard ratio, 0.52; P = .0052) or negative (9.5 vs. 3.8 months; hazard ratio, 0.44; P less than .0001).
“Detection of estrogen receptor mutations was strongly associated with acquired resistance to prior aromatase inhibitors,” Dr. Turner said.
“Palbociclib offered high efficacy regardless of the estrogen receptor mutation status,” he added. “And because in this patient population estrogen receptor mutations are detected frequently, the combination of palbociclib and fulvestrant presents an attractive treatment option for patients who have been previously treated with and progressed on aromatase inhibitors.”
CHICAGO – Mutation of the estrogen receptor 1 (ESR1) gene, one of the mechanisms whereby tumors become resistant to endocrine therapy, may be prognostic but not predictive in women with hormone receptor–positive advanced breast cancer that has progressed on this therapy, two studies showed.
In a cohort of women who had experienced progression on a first-line aromatase inhibitor, those with ESR1 mutations detected in circulating cell-free DNA at the time of progression had a 70% higher risk of progression-free survival events and a 90% higher risk of death thereafter. But the presence of this mutation did not predict benefit from subsequent therapy.
Similarly, in an analysis of women who had experienced progression on prior endocrine therapy and were treated on the randomized PALOMA-3 trial with fulvestrant plus either palbociclib (a cyclin-dependent kinase inhibitor) or placebo, adding the drug reduced the risk of progression-free survival events similarly, by about 50%, regardless of the presence of ESR1 mutations before starting therapy.
Findings in context
These new findings can help guide decisions about which patients should be tested for ESR1 mutations, according to invited discussant Sarat Chandarlapaty, MD, PhD, a medical oncologist at the Memorial Sloan Kettering Cancer Center in New York.
“Putting it all together … we see ESR1 mutations arise in the metastatic setting subclonally with prolonged exposure to low-estrogen environments,” he said. “If we are going to do testing, it makes sense to do it in the setting in which there is prior exposure to an aromatase inhibitor in metastatic ER-positive breast cancer.”
The studies’ results also help clarify what the finding of an ESR1 mutation means for patient prognosis and choice of next therapy, Dr. Chandarlapaty said at the annual meeting of the American Society of Clinical Oncology.
“It’s clear from two large studies that ESR1 mutation prognosticates poorer and shorter survival, so just the finding alone may aid as sort of a clinical risk assessment for physicians,” he said. “For the question of prediction, I would say the weight of evidence—even though the clinical studies are small—all the way from biology to clinic is that ESR1-mutant patients are unlikely to benefit from a second-line aromatase inhibitor.”
However, “the question of whether testing should be made available in practice on the basis of this particular clinical decision is more complicated,” Dr. Chandarlapaty said. “For one, is second-line aromatase inhibitor alone a widely used option? Secondly, does the adoption now of palbociclib in the first-line setting change the biology and the nature of resistance at this later line – in other words, are we going to see patients going on to a second-line aromatase inhibitor after they’ve had a prior aromatase inhibitor plus palbociclib?”
Mutations after progression on first-line aromatase inhibitors
In the first study, Florian Clatot, MD, PhD, a medical oncologist at the Centre Henri Becquerel, University of Normandy, Rouen, France, and colleagues retrospectively studied 144 women who had experienced progression on a first-line aromatase inhibitor.
The investigators used digital droplet polymerase chain reaction (PCR) testing to screen for four ESR-1 mutations in circulating cell-free DNA collected before, at the time of, and after the progression.
Overall, 30.6% of women were found to have at least one of these mutations at the time of progression, Dr. Clatot reported. The prevalence was higher the longer women had been on the aromatase inhibitor.
After progression, most women went on to receive chemotherapy or alternative endocrine therapy with either the selective estrogen receptor modulator tamoxifen or the estrogen receptor antagonist fulvestrant (Faslodex). With a median follow-up of 40 months, multivariate analyses showed that the group with ESR1 mutations at progression had higher risks of subsequent progression-free survival events (hazard ratio, 1.7; P = .008) and death (hazard ratio, 1.9; P = .002).
However, the mutations were not predictive: Women having one fared more poorly, whether given chemotherapy or given tamoxifen or fulvestrant.
Kinetic analyses showed that 75% of the ESR1 mutations seen at progression were already detectable in the 3 and even 6 months before that event. “Most of the mutations detected before progression increased while aromatase inhibitor therapy was ongoing,” Dr. Clatot commented. “These results suggest that the preclinical detection of ESR1 circulating mutation may [be of] clinical interest.”
Most women who had mutations at progression saw a decrease in the amount detectable over the subsequent 3 months with therapy, including to the point of not being detectable in about half of cases with a reduction. All of those having an increase in mutational burden had progression on their next therapy, compared with only about 40% of those having a decrease in burden.
“Taken together, these results suggest that the selection pressure provided by aromatase inhibitor exposure is one of the main mechanisms of ESR1 mutation increase,” concluded Dr. Clatot. “ESR1 mutations are a strong and independent marker of poor prognosis but do not have any predictive value with the treatments used in our cohort.”
Mutations after progression on prior endocrine therapy
In the second study, Nicholas C. Turner, MD, PhD, a medical oncologist at the Royal Marsden Hospital and Institute of Cancer Research, London, and colleagues analyzed data from a subset of 395 women from PALOMA-3.
The randomized phase III trial tested fulvestrant combined with palbociclib (Ibrance), an oral inhibitor of cyclin-dependent kinases 4 and 6, or placebo. All of the women enrolled had experienced progression on prior endocrine therapy in the adjuvant, advanced, or metastatic setting.
The investigators looked for 12 ESR1 mutations in circulating tumor DNA from baseline plasma samples using the BEAMing (beads, emulsion, amplification, magnetics) digital PCR technique and droplet digital PCR screening.
Overall, 27% of the women had ESR1 mutations before starting therapy on the trial, Dr. Turner reported. Mutations were seen in those who had received a prior aromatase inhibitor, but not in those who had received only prior tamoxifen. “So it’s quite clear these mutations are not a mechanism of resistance to tamoxifen, suggesting that tamoxifen must have at least some activity against these mutations,” he commented.
In addition, ESR1 mutations were more common in patients who had been sensitive versus not to prior endocrine therapy of any type (30.3% vs. 12.8%) and in patients who had been sensitive versus not specifically to prior aromatase inhibitor therapy (34.6% vs. 11.1%).
Stratified analyses showed that palbociclib was similarly superior to placebo in terms of progression-free survival whether patients were positive for an ESR1 mutation (9.4 vs. 4.1 months; hazard ratio, 0.52; P = .0052) or negative (9.5 vs. 3.8 months; hazard ratio, 0.44; P less than .0001).
“Detection of estrogen receptor mutations was strongly associated with acquired resistance to prior aromatase inhibitors,” Dr. Turner said.
“Palbociclib offered high efficacy regardless of the estrogen receptor mutation status,” he added. “And because in this patient population estrogen receptor mutations are detected frequently, the combination of palbociclib and fulvestrant presents an attractive treatment option for patients who have been previously treated with and progressed on aromatase inhibitors.”
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: An ESR1 mutation in circulating DNA after progression on endocrine therapy was a marker for poor prognosis but did not predict benefit from subsequent therapy.
Major finding: Women with ESR1 mutations had poorer progression-free and overall survival (hazard ratios, 1.7 and 1.9). Adding palbociclib to fulvestrant halved the risk of progression-free survival events, regardless of the presence of an ESR1 mutation.
Data source: A retrospective cohort study of 144 women with metastatic breast cancer who had experienced progression on a first-line aromatase inhibitor, and an analysis of 395 women with advanced breast cancer from a randomized trial testing addition of palbociclib to fulvestrant after progression on prior endocrine therapy (PALOMA-3 trial).
Disclosures: Dr. Clatot disclosed that he receives research funding from Novartis. Dr. Turner disclosed that he receives honoraria from and has a consulting or advisory role with AstraZeneca, Pfizer, and Roche Pharma; Pfizer sponsored PALOMA-3, and AstraZeneca provided the fulvestrant.
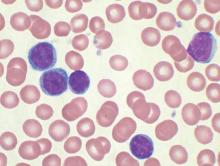
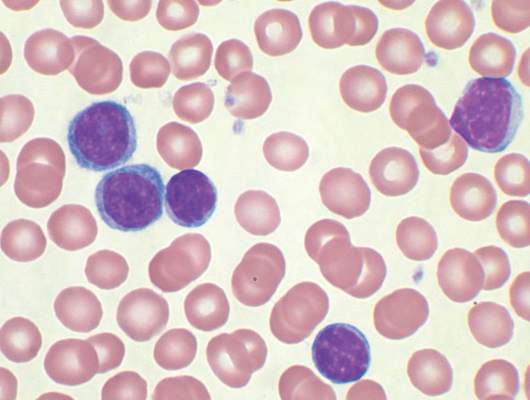
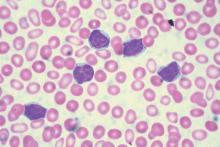
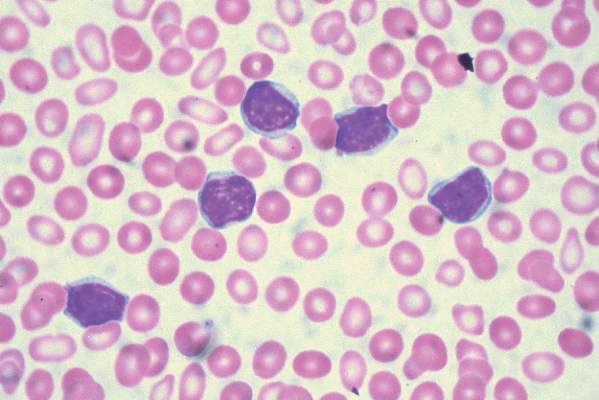
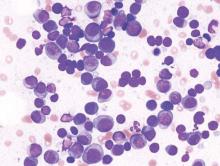
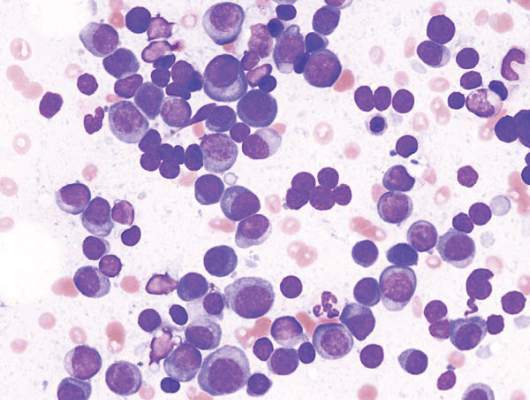
CAR T-cell therapy eyed for CLL patients with residual disease
Four of eight patients with residual chronic lymphocytic leukemia (CLL) following initial chemotherapy had complete or partial responses to an outpatient therapy that used autologous T cells genetically targeted to the B cell–specific antigen CD19, Mark Blaine Geyer, MD, of Memorial Sloan Kettering Cancer Center, New York, reported at the annual meeting of the American Society of Clinical Oncology.
The therapy employing T cells genetically modified to express CD19-targeted 19-28z chimeric antigen receptors (CARs) was well tolerated but had limited observed efficacy, especially in patients with enlarged lymph nodes. The study goal was to find a safe dose of modified T cells for patients who have disease remaining after initial chemotherapy.
For the phase I dose escalation study (NCT01416974), Dr. Geyer and his associates enrolled eight CLL patients who had residual disease after upfront therapy consisting of six cycles of pentostatin, cyclophosphamide, and rituximab.
Five patients had clearly enlarged lymph nodes prior to T cell infusion.
Patients received cyclophosphamide 600 mg/m2 followed 2 days later by escalating doses of 19-28z T cells. Four of the five patients who received at least a 1 × 107 dose of 19-28z T cells/kg were admitted with fevers and mild cytokine release syndrome.
Maximal levels of CAR T cell persistence were detected at 8 weeks. With a median patient follow-up of 32 months, clinical complete response has been seen in two patients, partial response in two patients, and stable disease in one patient. Disease has progressed in three patients: one had a rising absolute lymphocyte count by the time of infusion and two had marrow response with progressive disease in lymph nodes. The median time to disease progression was 13.6 months, Dr. Geyer said.
Five of seven evaluable patients have received further CLL-directed therapy.
The researchers speculated that low-dose cyclophosphamide monotherapy, used before the CAR T-cell therapy, may be insufficient for lymphodepletion. Additionally, CAR T cell expansion and antitumor efficacy may be limited by a hostile CLL microenvironment. Strategies to enhance CAR T cell expansion and efficacy in patients with CLL are in preparation, Dr. Geyer reported.
Dr. Geyer had no financial disclosures. His colleagues reported various financial relationships with Juno Therapeutics, a developer of CAR technology.
On Twitter @maryjodales
Four of eight patients with residual chronic lymphocytic leukemia (CLL) following initial chemotherapy had complete or partial responses to an outpatient therapy that used autologous T cells genetically targeted to the B cell–specific antigen CD19, Mark Blaine Geyer, MD, of Memorial Sloan Kettering Cancer Center, New York, reported at the annual meeting of the American Society of Clinical Oncology.
The therapy employing T cells genetically modified to express CD19-targeted 19-28z chimeric antigen receptors (CARs) was well tolerated but had limited observed efficacy, especially in patients with enlarged lymph nodes. The study goal was to find a safe dose of modified T cells for patients who have disease remaining after initial chemotherapy.
For the phase I dose escalation study (NCT01416974), Dr. Geyer and his associates enrolled eight CLL patients who had residual disease after upfront therapy consisting of six cycles of pentostatin, cyclophosphamide, and rituximab.
Five patients had clearly enlarged lymph nodes prior to T cell infusion.
Patients received cyclophosphamide 600 mg/m2 followed 2 days later by escalating doses of 19-28z T cells. Four of the five patients who received at least a 1 × 107 dose of 19-28z T cells/kg were admitted with fevers and mild cytokine release syndrome.
Maximal levels of CAR T cell persistence were detected at 8 weeks. With a median patient follow-up of 32 months, clinical complete response has been seen in two patients, partial response in two patients, and stable disease in one patient. Disease has progressed in three patients: one had a rising absolute lymphocyte count by the time of infusion and two had marrow response with progressive disease in lymph nodes. The median time to disease progression was 13.6 months, Dr. Geyer said.
Five of seven evaluable patients have received further CLL-directed therapy.
The researchers speculated that low-dose cyclophosphamide monotherapy, used before the CAR T-cell therapy, may be insufficient for lymphodepletion. Additionally, CAR T cell expansion and antitumor efficacy may be limited by a hostile CLL microenvironment. Strategies to enhance CAR T cell expansion and efficacy in patients with CLL are in preparation, Dr. Geyer reported.
Dr. Geyer had no financial disclosures. His colleagues reported various financial relationships with Juno Therapeutics, a developer of CAR technology.
On Twitter @maryjodales
Four of eight patients with residual chronic lymphocytic leukemia (CLL) following initial chemotherapy had complete or partial responses to an outpatient therapy that used autologous T cells genetically targeted to the B cell–specific antigen CD19, Mark Blaine Geyer, MD, of Memorial Sloan Kettering Cancer Center, New York, reported at the annual meeting of the American Society of Clinical Oncology.
The therapy employing T cells genetically modified to express CD19-targeted 19-28z chimeric antigen receptors (CARs) was well tolerated but had limited observed efficacy, especially in patients with enlarged lymph nodes. The study goal was to find a safe dose of modified T cells for patients who have disease remaining after initial chemotherapy.
For the phase I dose escalation study (NCT01416974), Dr. Geyer and his associates enrolled eight CLL patients who had residual disease after upfront therapy consisting of six cycles of pentostatin, cyclophosphamide, and rituximab.
Five patients had clearly enlarged lymph nodes prior to T cell infusion.
Patients received cyclophosphamide 600 mg/m2 followed 2 days later by escalating doses of 19-28z T cells. Four of the five patients who received at least a 1 × 107 dose of 19-28z T cells/kg were admitted with fevers and mild cytokine release syndrome.
Maximal levels of CAR T cell persistence were detected at 8 weeks. With a median patient follow-up of 32 months, clinical complete response has been seen in two patients, partial response in two patients, and stable disease in one patient. Disease has progressed in three patients: one had a rising absolute lymphocyte count by the time of infusion and two had marrow response with progressive disease in lymph nodes. The median time to disease progression was 13.6 months, Dr. Geyer said.
Five of seven evaluable patients have received further CLL-directed therapy.
The researchers speculated that low-dose cyclophosphamide monotherapy, used before the CAR T-cell therapy, may be insufficient for lymphodepletion. Additionally, CAR T cell expansion and antitumor efficacy may be limited by a hostile CLL microenvironment. Strategies to enhance CAR T cell expansion and efficacy in patients with CLL are in preparation, Dr. Geyer reported.
Dr. Geyer had no financial disclosures. His colleagues reported various financial relationships with Juno Therapeutics, a developer of CAR technology.
On Twitter @maryjodales
FROM THE 2016 ASCO ANNUAL MEETING
Key clinical point: CAR T-cell therapy may be an option for chronic lymphocytic leukemia patients with residual disease after upfront therapy.
Major finding: Four of eight patients with residual CLL following initial chemotherapy had complete or partial responses to an outpatient therapy that used autologous T cells genetically targeted to the B cell–specific antigen CD19.
Data source: A phase I dose-finding and efficacy study in 8 patients with CLL.
Disclosures: Dr. Geyer had no financial disclosures. His colleagues reported various financial relationships with Juno Therapeutics, a developer of CAR technology.
First-in-class agent shows early promise in treating clear cell renal cell carcinoma
CHICAGO – Investigational agent PT2385, an inhibitor of hypoxia-inducible factor 2-alpha (HIF-2alpha), appears safe and tolerable and demonstrated early evidence of clinical activity in heavily pretreated patients with advanced clear cell renal cell carcinoma, investigators reported at the annual meeting of the American Society of Clinical Oncology.
In a small, phase I dose-escalation study, 39% of patients in the study achieved complete response, partial response, or stable disease lasting at least 16 weeks.
PT2385 is a first-in-class, orally administered selective small molecule inhibitor of HIF-2alpha, a transcription factor with a role in clear cell renal cell carcinoma.
“Hypoxia-inducible factor 2-alpha is a key oncogenic driver of clear cell renal cell carcinoma,” Kevin Courtney, MD, PhD, of the University of Texas Southwestern Medical Center, Dallas, said at the meeting.
A total of 51 patients (n = 26 for dose escalation cohort and n = 25 in dose expansion cohort) met the study’s eligibility requirements of having a diagnosis of clear cell renal cell carcinoma, an Eastern Cooperative Oncology Group score ranging from 0 to 1, and at least one prior anticancer therapy. The median age of the cohort was 65 years with the youngest participant being 29 years and the oldest being 80 years old. The majority of patients were male (71%), had received four or more prior systemic therapies (53%), and had undergone vascular endothelial growth factor therapy (98%). Patients were treated with continuous twice-daily oral dosing of PT2385 until progression or toxicity. A total of three patients were treated at the 100-mg dose, three at the 200-mg dose, four at the 400-mg dose, seven at the 800-mg dose, six at a dose of 1,200 mg, and three at a dose of 1,800 mg.
“No dose-limiting toxicity was observed at any dose level,” Dr. Courtney said.
Based on safety, pharmokinetic and pharmodynamic data, 800 mg twice daily was the selected dose for the expansion cohort, he reported.
Of 51 patients treated, 1 patient had a complete response, 3 achieved partial responses, and 16 patients achieved stable disease for at least 16 weeks. The most common grade one or two adverse events were anemia (n = 18), peripheral edema (n = 18), fatigue (n = 18), nausea (n = 15), and back pain (n = 12). Only two grade four adverse events (low lymphocyte count) were reported.
“Notably, hypertension was not seen,” Dr. Courtney said.
At the time the study concluded, the four patients who achieved complete or partial responses remained on the treatment, and five had received treatment for a year or longer.
The study was funded by Peloton Therapeutics. Dr. Courtney reported having stock and ownership interest in, serving in advisory roles for, or receiving research funding from multiple companies. Several coinvestigators reported receiving research funding from or holding patents with multiple companies including Peloton Therapeutics.
On Twitter @jessnicolecraig
CHICAGO – Investigational agent PT2385, an inhibitor of hypoxia-inducible factor 2-alpha (HIF-2alpha), appears safe and tolerable and demonstrated early evidence of clinical activity in heavily pretreated patients with advanced clear cell renal cell carcinoma, investigators reported at the annual meeting of the American Society of Clinical Oncology.
In a small, phase I dose-escalation study, 39% of patients in the study achieved complete response, partial response, or stable disease lasting at least 16 weeks.
PT2385 is a first-in-class, orally administered selective small molecule inhibitor of HIF-2alpha, a transcription factor with a role in clear cell renal cell carcinoma.
“Hypoxia-inducible factor 2-alpha is a key oncogenic driver of clear cell renal cell carcinoma,” Kevin Courtney, MD, PhD, of the University of Texas Southwestern Medical Center, Dallas, said at the meeting.
A total of 51 patients (n = 26 for dose escalation cohort and n = 25 in dose expansion cohort) met the study’s eligibility requirements of having a diagnosis of clear cell renal cell carcinoma, an Eastern Cooperative Oncology Group score ranging from 0 to 1, and at least one prior anticancer therapy. The median age of the cohort was 65 years with the youngest participant being 29 years and the oldest being 80 years old. The majority of patients were male (71%), had received four or more prior systemic therapies (53%), and had undergone vascular endothelial growth factor therapy (98%). Patients were treated with continuous twice-daily oral dosing of PT2385 until progression or toxicity. A total of three patients were treated at the 100-mg dose, three at the 200-mg dose, four at the 400-mg dose, seven at the 800-mg dose, six at a dose of 1,200 mg, and three at a dose of 1,800 mg.
“No dose-limiting toxicity was observed at any dose level,” Dr. Courtney said.
Based on safety, pharmokinetic and pharmodynamic data, 800 mg twice daily was the selected dose for the expansion cohort, he reported.
Of 51 patients treated, 1 patient had a complete response, 3 achieved partial responses, and 16 patients achieved stable disease for at least 16 weeks. The most common grade one or two adverse events were anemia (n = 18), peripheral edema (n = 18), fatigue (n = 18), nausea (n = 15), and back pain (n = 12). Only two grade four adverse events (low lymphocyte count) were reported.
“Notably, hypertension was not seen,” Dr. Courtney said.
At the time the study concluded, the four patients who achieved complete or partial responses remained on the treatment, and five had received treatment for a year or longer.
The study was funded by Peloton Therapeutics. Dr. Courtney reported having stock and ownership interest in, serving in advisory roles for, or receiving research funding from multiple companies. Several coinvestigators reported receiving research funding from or holding patents with multiple companies including Peloton Therapeutics.
On Twitter @jessnicolecraig
CHICAGO – Investigational agent PT2385, an inhibitor of hypoxia-inducible factor 2-alpha (HIF-2alpha), appears safe and tolerable and demonstrated early evidence of clinical activity in heavily pretreated patients with advanced clear cell renal cell carcinoma, investigators reported at the annual meeting of the American Society of Clinical Oncology.
In a small, phase I dose-escalation study, 39% of patients in the study achieved complete response, partial response, or stable disease lasting at least 16 weeks.
PT2385 is a first-in-class, orally administered selective small molecule inhibitor of HIF-2alpha, a transcription factor with a role in clear cell renal cell carcinoma.
“Hypoxia-inducible factor 2-alpha is a key oncogenic driver of clear cell renal cell carcinoma,” Kevin Courtney, MD, PhD, of the University of Texas Southwestern Medical Center, Dallas, said at the meeting.
A total of 51 patients (n = 26 for dose escalation cohort and n = 25 in dose expansion cohort) met the study’s eligibility requirements of having a diagnosis of clear cell renal cell carcinoma, an Eastern Cooperative Oncology Group score ranging from 0 to 1, and at least one prior anticancer therapy. The median age of the cohort was 65 years with the youngest participant being 29 years and the oldest being 80 years old. The majority of patients were male (71%), had received four or more prior systemic therapies (53%), and had undergone vascular endothelial growth factor therapy (98%). Patients were treated with continuous twice-daily oral dosing of PT2385 until progression or toxicity. A total of three patients were treated at the 100-mg dose, three at the 200-mg dose, four at the 400-mg dose, seven at the 800-mg dose, six at a dose of 1,200 mg, and three at a dose of 1,800 mg.
“No dose-limiting toxicity was observed at any dose level,” Dr. Courtney said.
Based on safety, pharmokinetic and pharmodynamic data, 800 mg twice daily was the selected dose for the expansion cohort, he reported.
Of 51 patients treated, 1 patient had a complete response, 3 achieved partial responses, and 16 patients achieved stable disease for at least 16 weeks. The most common grade one or two adverse events were anemia (n = 18), peripheral edema (n = 18), fatigue (n = 18), nausea (n = 15), and back pain (n = 12). Only two grade four adverse events (low lymphocyte count) were reported.
“Notably, hypertension was not seen,” Dr. Courtney said.
At the time the study concluded, the four patients who achieved complete or partial responses remained on the treatment, and five had received treatment for a year or longer.
The study was funded by Peloton Therapeutics. Dr. Courtney reported having stock and ownership interest in, serving in advisory roles for, or receiving research funding from multiple companies. Several coinvestigators reported receiving research funding from or holding patents with multiple companies including Peloton Therapeutics.
On Twitter @jessnicolecraig
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: The first-in-class oral HIF-2alpha inhibitor PT2385 demonstrated early evidence of clinical activity in patients with advanced clear cell renal cell carcinoma. The drug also appears safe and tolerable.
Major finding: Overall, one patient had a complete response, three achieved partial responses, and 16 patients achieved stable disease for at least 16 weeks.
Data source: A phase I dose-escalation and expansion study of 51 heavily pretreated patients with advanced clear cell renal cell carcinoma.
Disclosures: The study was funded by Peloton Therapeutics. Dr. Courtney reported having stock and ownership interest in, serving in advisory roles for, or receiving research funding from multiple companies. Several coinvestigators reported receiving research funding from or holding patents with multiple companies including Peloton Therapeutics.
Anthracycline benefit for high-risk breast cancer confirmed in joint analysis
CHICAGO – Docetaxel plus cyclophosphamide was significantly inferior to treatment with anthracycline/taxane-based chemotherapy, according to an interim joint analysis of the ABC (anthracyclines in early breast cancer) trials.
The ABC trials are three sequential trials from the US Oncology Research and National Surgical Adjuvant Breast and Bowel Project that randomized women with resected high-risk, early-stage breast cancer to receive docetaxel plus cyclophosphamide (TC) or one of several standard anthracycline/taxane-based chemotherapy (TaxAC) regimens.
A total of 4,130 patients met the ABC trials’ eligibility requirements and were randomly assigned to receive either TC therapy (n = 2,078) or TaxAC therapy (n = 2,052), Joanne Blum, MD, PhD, of the Texas Oncology-Baylor Charles A. Sammons Cancer Center, Dallas, reported at the annual meeting of the American Society of Clinical Oncology.
Patient and tumor characteristics were balanced among the two treatment arms, and the median follow-up time was 3.2 years.
Inferiority was predefined as a Cox model hazard ratio (HR) score of 1.18 or higher when the cohort was stratified by nodal status, hormone-receptor status, and parent trial, Dr. Blum said.
The HR for the initial 334 events was 1.2, which exceeded the threshold and demonstrated that TC was inferior to TaxAC.
At the interim analysis, 399 events had occurred: 220 in the TC treatment arm and 179 in the TaxAC arm. Overall, the 4-year invasive disease-free survival was 88.2% for the TC treatment arm and 90.7% for the TaxAC treatment arm (HR, 1.23; 95% confidence interval, 1.01-1.50; P = .04). TaxAC was equal or superior to TC when the cohort was stratified by parent trial, hormone status, and nodal status. TC regimen was favored only in ER-positive patients with zero nodes.
There was no difference in overall survival between the two treatment arms.
Exploratory subgroup analyses suggest that TaxAC provides little benefit in ER-positive, node-negative cohorts, small benefit in ER-positive one-to-three node and ER-negative node-negative cohorts, and the most benefit for patients who were ER-positive with more than four nodes or ER-negative node-positive, Dr. Blum said.
Acute leukemia occurred in 0.24% of patients in the TaxAC group and in none of the patients in the TC treatment arm.
“Additional follow-up and correlative studies to identify biomarkers of anthracycline benefit will be crucial for fully determining the utility of anthracyclines across this heterogeneous patient population,” Dr. Blum concluded.
Dr. Blum had no disclosures to report. Sanofi, Genentech, and CTEP funded the ABC trials.
On Twitter @jessnicolecraig
CHICAGO – Docetaxel plus cyclophosphamide was significantly inferior to treatment with anthracycline/taxane-based chemotherapy, according to an interim joint analysis of the ABC (anthracyclines in early breast cancer) trials.
The ABC trials are three sequential trials from the US Oncology Research and National Surgical Adjuvant Breast and Bowel Project that randomized women with resected high-risk, early-stage breast cancer to receive docetaxel plus cyclophosphamide (TC) or one of several standard anthracycline/taxane-based chemotherapy (TaxAC) regimens.
A total of 4,130 patients met the ABC trials’ eligibility requirements and were randomly assigned to receive either TC therapy (n = 2,078) or TaxAC therapy (n = 2,052), Joanne Blum, MD, PhD, of the Texas Oncology-Baylor Charles A. Sammons Cancer Center, Dallas, reported at the annual meeting of the American Society of Clinical Oncology.
Patient and tumor characteristics were balanced among the two treatment arms, and the median follow-up time was 3.2 years.
Inferiority was predefined as a Cox model hazard ratio (HR) score of 1.18 or higher when the cohort was stratified by nodal status, hormone-receptor status, and parent trial, Dr. Blum said.
The HR for the initial 334 events was 1.2, which exceeded the threshold and demonstrated that TC was inferior to TaxAC.
At the interim analysis, 399 events had occurred: 220 in the TC treatment arm and 179 in the TaxAC arm. Overall, the 4-year invasive disease-free survival was 88.2% for the TC treatment arm and 90.7% for the TaxAC treatment arm (HR, 1.23; 95% confidence interval, 1.01-1.50; P = .04). TaxAC was equal or superior to TC when the cohort was stratified by parent trial, hormone status, and nodal status. TC regimen was favored only in ER-positive patients with zero nodes.
There was no difference in overall survival between the two treatment arms.
Exploratory subgroup analyses suggest that TaxAC provides little benefit in ER-positive, node-negative cohorts, small benefit in ER-positive one-to-three node and ER-negative node-negative cohorts, and the most benefit for patients who were ER-positive with more than four nodes or ER-negative node-positive, Dr. Blum said.
Acute leukemia occurred in 0.24% of patients in the TaxAC group and in none of the patients in the TC treatment arm.
“Additional follow-up and correlative studies to identify biomarkers of anthracycline benefit will be crucial for fully determining the utility of anthracyclines across this heterogeneous patient population,” Dr. Blum concluded.
Dr. Blum had no disclosures to report. Sanofi, Genentech, and CTEP funded the ABC trials.
On Twitter @jessnicolecraig
CHICAGO – Docetaxel plus cyclophosphamide was significantly inferior to treatment with anthracycline/taxane-based chemotherapy, according to an interim joint analysis of the ABC (anthracyclines in early breast cancer) trials.
The ABC trials are three sequential trials from the US Oncology Research and National Surgical Adjuvant Breast and Bowel Project that randomized women with resected high-risk, early-stage breast cancer to receive docetaxel plus cyclophosphamide (TC) or one of several standard anthracycline/taxane-based chemotherapy (TaxAC) regimens.
A total of 4,130 patients met the ABC trials’ eligibility requirements and were randomly assigned to receive either TC therapy (n = 2,078) or TaxAC therapy (n = 2,052), Joanne Blum, MD, PhD, of the Texas Oncology-Baylor Charles A. Sammons Cancer Center, Dallas, reported at the annual meeting of the American Society of Clinical Oncology.
Patient and tumor characteristics were balanced among the two treatment arms, and the median follow-up time was 3.2 years.
Inferiority was predefined as a Cox model hazard ratio (HR) score of 1.18 or higher when the cohort was stratified by nodal status, hormone-receptor status, and parent trial, Dr. Blum said.
The HR for the initial 334 events was 1.2, which exceeded the threshold and demonstrated that TC was inferior to TaxAC.
At the interim analysis, 399 events had occurred: 220 in the TC treatment arm and 179 in the TaxAC arm. Overall, the 4-year invasive disease-free survival was 88.2% for the TC treatment arm and 90.7% for the TaxAC treatment arm (HR, 1.23; 95% confidence interval, 1.01-1.50; P = .04). TaxAC was equal or superior to TC when the cohort was stratified by parent trial, hormone status, and nodal status. TC regimen was favored only in ER-positive patients with zero nodes.
There was no difference in overall survival between the two treatment arms.
Exploratory subgroup analyses suggest that TaxAC provides little benefit in ER-positive, node-negative cohorts, small benefit in ER-positive one-to-three node and ER-negative node-negative cohorts, and the most benefit for patients who were ER-positive with more than four nodes or ER-negative node-positive, Dr. Blum said.
Acute leukemia occurred in 0.24% of patients in the TaxAC group and in none of the patients in the TC treatment arm.
“Additional follow-up and correlative studies to identify biomarkers of anthracycline benefit will be crucial for fully determining the utility of anthracyclines across this heterogeneous patient population,” Dr. Blum concluded.
Dr. Blum had no disclosures to report. Sanofi, Genentech, and CTEP funded the ABC trials.
On Twitter @jessnicolecraig
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Anthracyclines continue to have a role in the treatment of high-risk, HER2-negative breast cancer.
Major finding: 4-year invasive disease-free survival was 88.2% for the TC treatment arm and 90.7% for the TaxAC treatment arm (HR, 1.23; 95% CI, 1.01-1.50; P = .04).
Data source: An interim analysis of the ABC trials involved a total of 4,130 patients with breast cancer.
Disclosures: Dr. Blum had no disclosures to report. Sanofi, Genentech, and CTEP funded the ABC trials.
New data shed light on impact of resecting the primary tumor in stage IV breast cancer
CHICAGO – The survival impact of resecting the primary tumor in women with de novo stage IV breast cancer depends on receipt of and response to prior systemic therapy, suggested a pair of studies reported at the annual meeting of the American Society of Clinical Oncology.
A randomized trial conducted in Turkey found that, relative to peers who received initial systemic therapy, women who underwent initial resection of the primary tumor had a one-third lower risk of death at 5 years. But a prospective registry study conducted in the United States found that elective resection after a response to first-line therapy did not significantly improve overall survival, with patients living roughly 6 years regardless of whether they had the surgery or not.
Findings in context
“I think these studies have just confirmed what we know, and that is that tumor biology is critical,” said invited discussant Elizabeth A. Mittendorf, MD, PhD, of University of Texas MD Anderson Cancer Center, Houston. “Patients who do not respond to systemic therapy will do poorly, so I don’t think it’s unwise to consider a biologic ‘stress test’ with initiation of first-line therapy, knowing that patients who do not respond will not benefit from surgery.”
Those with hormone receptor–positive or HER2-positive disease are most likely to benefit from targeted therapy and may see even higher response rates as novel targeted agents are introduced. “But despite the increase in response to therapy, we really have no data at this time to suggest any benefit from surgery,” she added. “There may be some utility in continuing to enroll these patients in a clinical trial. I would suggest that it would need to be a subtype-specific trial and would question whether we have the appetite to conduct such a study.”
More information on managing de novo stage IV breast cancer is expected from ongoing trials such as the Eastern Cooperative Oncology Group’s 2108 trial, which is randomizing patients having a response or stable disease with first-line therapy to either early local therapy or delayed local therapy only at the time of progression, according to Dr. Mittendorf.
Poor accrual necessitated redesign of the trial. “As part of that redesign, there was a decrease in the target enrollment, which causes me concern that the trial will not be powered to inform its primary endpoint of overall survival,” she commented. However, “it’s interesting to note that in early 2014, shortly after the report of the trials from India and Turkey at the San Antonio Breast Cancer Symposium, there was a significant increase in enrollment, suggesting that this is a clinically important question.”
Turkish study: MF07-01
The first study – trial MF07-01 of the Turkish Federation of Breast Diseases Societies – was presented by Atilla Soran, MD, of Magee-Womens Hospital of University of Pittsburgh Medical Center.
He and his colleagues enrolled in the trial women with de novo stage IV breast cancer whose primary tumor was amenable to complete surgical resection and who were healthy enough to be treated.
The women were randomized evenly either to initial systemic therapy followed by local therapy only if local progression occurred, or to initial local therapy, consisting of surgery with or without radiation therapy of the breast and axilla, followed by systemic therapy.
Among the 274 evaluable women having a median follow-up of about 40 months, the 3-year rate of overall survival did not differ significantly between the two groups, Dr. Soran reported.
However, the 5-year rate of overall survival was 41.6% in the initial surgery group and 24.4% in the initial systemic therapy group, a difference translating to a significant reduction in the risk of death (hazard ratio, 0.66; P = .005). Median survival was 46 months and 37 months, respectively.
The benefit was similar in women whose tumors had hormone receptors, whose tumors were negative for HER2, and who were younger than age 55. There was no significant benefit of up-front surgery for women with bone-only metastases, “but we believe that when we follow these patients longer, the difference is going to be statistically significant,” he said.
On the other hand, there was a trend among women who had multiple pulmonary and/or liver metastases whereby they were more likely to die if they initially had surgery instead of systemic therapy.
Locoregional progression/relapse occurred in 1% of the initial surgery group but 11% of the initial systemic therapy group. Among women who did not have locoregional progression/relapse, surgery still had a survival benefit (HR, 0.61; P = .001).
“We know that with systemic therapy, immunotherapy, radiation therapy, and imaging as developments, patients are living longer when you compare to a decade ago or 20 years ago,” said Dr. Soran. “But we also believe that there is a role for surgery of the primary tumor in those patients.”
“Performance status, age, and comorbidities must be taken into account, and the burden of metastatic disease needs to be considered,” he maintained. “The benefit of surgery at presentation is dependent on the completeness of resection, and axillary surgery and locoregional radiation therapy should be considered regardless of the metastasis.”
U.S. study: TBCRC 013
The second study – the Translational Breast Cancer Research Consortium’s study 013 – was presented by Tari A. King, MD, chief of breast surgery at the Dana-Farber Cancer Institute, associate division chief for breast surgery at Brigham and Women’s Hospital, and associate professor of surgery at Harvard Medical School, all in Boston.
The investigators analyzed data from the study’s cohort A, consisting of 112 patients with de novo stage IV breast cancer who had an intact primary tumor. All patients were given first-line systemic therapy; those who had a response were additionally offered elective resection of their primary tumor.
The median duration of follow-up was 54 months. Overall, 85% of the women had a response to their first-line therapy, Dr. King reported.
Some 43% of responders opted to undergo elective surgery to resect their primary tumor, defined as surgery performed in the absence of local symptoms or the need for local control, with specific type and extent left up to the treating physician.
In a multivariate analysis among responders surviving at least 6 months, median survival was 71 months with elective surgery and 65 months without it, a nonsignificant difference.
Findings were similar among subsets of women having estrogen receptor–positive tumors or HER2-positive tumors, and various combinations of these features.
In recursive partitioning analysis, response to first-line therapy, HER2 status, and age were the major determinants of survival.
“Importantly, although we were not able to demonstrate a survival benefit with the use of surgery, surgery also did not impact progression-free survival,” noted Dr. King.
Ultimately, 4% of responders who did not have elective surgery and 18% of nonresponders went on to have palliative resection of their primary.
“As this was a registry study, patients selected for surgery were more likely to have single-organ metastatic disease and to have received first-line chemotherapy, yet despite this selection bias, surgery did not impact survival in any tumor subtype,” Dr. King summarized. “Among patients who responded to therapy, HER2 status and patient age remained strong prognostic factors. Further investigation is needed to determine if subsets of patients will ultimately benefit from surgery.”
“In the absence of additional prospective data, our findings do not support surgery for the primary tumor outside of a clinical trial,” she concluded.
CHICAGO – The survival impact of resecting the primary tumor in women with de novo stage IV breast cancer depends on receipt of and response to prior systemic therapy, suggested a pair of studies reported at the annual meeting of the American Society of Clinical Oncology.
A randomized trial conducted in Turkey found that, relative to peers who received initial systemic therapy, women who underwent initial resection of the primary tumor had a one-third lower risk of death at 5 years. But a prospective registry study conducted in the United States found that elective resection after a response to first-line therapy did not significantly improve overall survival, with patients living roughly 6 years regardless of whether they had the surgery or not.
Findings in context
“I think these studies have just confirmed what we know, and that is that tumor biology is critical,” said invited discussant Elizabeth A. Mittendorf, MD, PhD, of University of Texas MD Anderson Cancer Center, Houston. “Patients who do not respond to systemic therapy will do poorly, so I don’t think it’s unwise to consider a biologic ‘stress test’ with initiation of first-line therapy, knowing that patients who do not respond will not benefit from surgery.”
Those with hormone receptor–positive or HER2-positive disease are most likely to benefit from targeted therapy and may see even higher response rates as novel targeted agents are introduced. “But despite the increase in response to therapy, we really have no data at this time to suggest any benefit from surgery,” she added. “There may be some utility in continuing to enroll these patients in a clinical trial. I would suggest that it would need to be a subtype-specific trial and would question whether we have the appetite to conduct such a study.”
More information on managing de novo stage IV breast cancer is expected from ongoing trials such as the Eastern Cooperative Oncology Group’s 2108 trial, which is randomizing patients having a response or stable disease with first-line therapy to either early local therapy or delayed local therapy only at the time of progression, according to Dr. Mittendorf.
Poor accrual necessitated redesign of the trial. “As part of that redesign, there was a decrease in the target enrollment, which causes me concern that the trial will not be powered to inform its primary endpoint of overall survival,” she commented. However, “it’s interesting to note that in early 2014, shortly after the report of the trials from India and Turkey at the San Antonio Breast Cancer Symposium, there was a significant increase in enrollment, suggesting that this is a clinically important question.”
Turkish study: MF07-01
The first study – trial MF07-01 of the Turkish Federation of Breast Diseases Societies – was presented by Atilla Soran, MD, of Magee-Womens Hospital of University of Pittsburgh Medical Center.
He and his colleagues enrolled in the trial women with de novo stage IV breast cancer whose primary tumor was amenable to complete surgical resection and who were healthy enough to be treated.
The women were randomized evenly either to initial systemic therapy followed by local therapy only if local progression occurred, or to initial local therapy, consisting of surgery with or without radiation therapy of the breast and axilla, followed by systemic therapy.
Among the 274 evaluable women having a median follow-up of about 40 months, the 3-year rate of overall survival did not differ significantly between the two groups, Dr. Soran reported.
However, the 5-year rate of overall survival was 41.6% in the initial surgery group and 24.4% in the initial systemic therapy group, a difference translating to a significant reduction in the risk of death (hazard ratio, 0.66; P = .005). Median survival was 46 months and 37 months, respectively.
The benefit was similar in women whose tumors had hormone receptors, whose tumors were negative for HER2, and who were younger than age 55. There was no significant benefit of up-front surgery for women with bone-only metastases, “but we believe that when we follow these patients longer, the difference is going to be statistically significant,” he said.
On the other hand, there was a trend among women who had multiple pulmonary and/or liver metastases whereby they were more likely to die if they initially had surgery instead of systemic therapy.
Locoregional progression/relapse occurred in 1% of the initial surgery group but 11% of the initial systemic therapy group. Among women who did not have locoregional progression/relapse, surgery still had a survival benefit (HR, 0.61; P = .001).
“We know that with systemic therapy, immunotherapy, radiation therapy, and imaging as developments, patients are living longer when you compare to a decade ago or 20 years ago,” said Dr. Soran. “But we also believe that there is a role for surgery of the primary tumor in those patients.”
“Performance status, age, and comorbidities must be taken into account, and the burden of metastatic disease needs to be considered,” he maintained. “The benefit of surgery at presentation is dependent on the completeness of resection, and axillary surgery and locoregional radiation therapy should be considered regardless of the metastasis.”
U.S. study: TBCRC 013
The second study – the Translational Breast Cancer Research Consortium’s study 013 – was presented by Tari A. King, MD, chief of breast surgery at the Dana-Farber Cancer Institute, associate division chief for breast surgery at Brigham and Women’s Hospital, and associate professor of surgery at Harvard Medical School, all in Boston.
The investigators analyzed data from the study’s cohort A, consisting of 112 patients with de novo stage IV breast cancer who had an intact primary tumor. All patients were given first-line systemic therapy; those who had a response were additionally offered elective resection of their primary tumor.
The median duration of follow-up was 54 months. Overall, 85% of the women had a response to their first-line therapy, Dr. King reported.
Some 43% of responders opted to undergo elective surgery to resect their primary tumor, defined as surgery performed in the absence of local symptoms or the need for local control, with specific type and extent left up to the treating physician.
In a multivariate analysis among responders surviving at least 6 months, median survival was 71 months with elective surgery and 65 months without it, a nonsignificant difference.
Findings were similar among subsets of women having estrogen receptor–positive tumors or HER2-positive tumors, and various combinations of these features.
In recursive partitioning analysis, response to first-line therapy, HER2 status, and age were the major determinants of survival.
“Importantly, although we were not able to demonstrate a survival benefit with the use of surgery, surgery also did not impact progression-free survival,” noted Dr. King.
Ultimately, 4% of responders who did not have elective surgery and 18% of nonresponders went on to have palliative resection of their primary.
“As this was a registry study, patients selected for surgery were more likely to have single-organ metastatic disease and to have received first-line chemotherapy, yet despite this selection bias, surgery did not impact survival in any tumor subtype,” Dr. King summarized. “Among patients who responded to therapy, HER2 status and patient age remained strong prognostic factors. Further investigation is needed to determine if subsets of patients will ultimately benefit from surgery.”
“In the absence of additional prospective data, our findings do not support surgery for the primary tumor outside of a clinical trial,” she concluded.
CHICAGO – The survival impact of resecting the primary tumor in women with de novo stage IV breast cancer depends on receipt of and response to prior systemic therapy, suggested a pair of studies reported at the annual meeting of the American Society of Clinical Oncology.
A randomized trial conducted in Turkey found that, relative to peers who received initial systemic therapy, women who underwent initial resection of the primary tumor had a one-third lower risk of death at 5 years. But a prospective registry study conducted in the United States found that elective resection after a response to first-line therapy did not significantly improve overall survival, with patients living roughly 6 years regardless of whether they had the surgery or not.
Findings in context
“I think these studies have just confirmed what we know, and that is that tumor biology is critical,” said invited discussant Elizabeth A. Mittendorf, MD, PhD, of University of Texas MD Anderson Cancer Center, Houston. “Patients who do not respond to systemic therapy will do poorly, so I don’t think it’s unwise to consider a biologic ‘stress test’ with initiation of first-line therapy, knowing that patients who do not respond will not benefit from surgery.”
Those with hormone receptor–positive or HER2-positive disease are most likely to benefit from targeted therapy and may see even higher response rates as novel targeted agents are introduced. “But despite the increase in response to therapy, we really have no data at this time to suggest any benefit from surgery,” she added. “There may be some utility in continuing to enroll these patients in a clinical trial. I would suggest that it would need to be a subtype-specific trial and would question whether we have the appetite to conduct such a study.”
More information on managing de novo stage IV breast cancer is expected from ongoing trials such as the Eastern Cooperative Oncology Group’s 2108 trial, which is randomizing patients having a response or stable disease with first-line therapy to either early local therapy or delayed local therapy only at the time of progression, according to Dr. Mittendorf.
Poor accrual necessitated redesign of the trial. “As part of that redesign, there was a decrease in the target enrollment, which causes me concern that the trial will not be powered to inform its primary endpoint of overall survival,” she commented. However, “it’s interesting to note that in early 2014, shortly after the report of the trials from India and Turkey at the San Antonio Breast Cancer Symposium, there was a significant increase in enrollment, suggesting that this is a clinically important question.”
Turkish study: MF07-01
The first study – trial MF07-01 of the Turkish Federation of Breast Diseases Societies – was presented by Atilla Soran, MD, of Magee-Womens Hospital of University of Pittsburgh Medical Center.
He and his colleagues enrolled in the trial women with de novo stage IV breast cancer whose primary tumor was amenable to complete surgical resection and who were healthy enough to be treated.
The women were randomized evenly either to initial systemic therapy followed by local therapy only if local progression occurred, or to initial local therapy, consisting of surgery with or without radiation therapy of the breast and axilla, followed by systemic therapy.
Among the 274 evaluable women having a median follow-up of about 40 months, the 3-year rate of overall survival did not differ significantly between the two groups, Dr. Soran reported.
However, the 5-year rate of overall survival was 41.6% in the initial surgery group and 24.4% in the initial systemic therapy group, a difference translating to a significant reduction in the risk of death (hazard ratio, 0.66; P = .005). Median survival was 46 months and 37 months, respectively.
The benefit was similar in women whose tumors had hormone receptors, whose tumors were negative for HER2, and who were younger than age 55. There was no significant benefit of up-front surgery for women with bone-only metastases, “but we believe that when we follow these patients longer, the difference is going to be statistically significant,” he said.
On the other hand, there was a trend among women who had multiple pulmonary and/or liver metastases whereby they were more likely to die if they initially had surgery instead of systemic therapy.
Locoregional progression/relapse occurred in 1% of the initial surgery group but 11% of the initial systemic therapy group. Among women who did not have locoregional progression/relapse, surgery still had a survival benefit (HR, 0.61; P = .001).
“We know that with systemic therapy, immunotherapy, radiation therapy, and imaging as developments, patients are living longer when you compare to a decade ago or 20 years ago,” said Dr. Soran. “But we also believe that there is a role for surgery of the primary tumor in those patients.”
“Performance status, age, and comorbidities must be taken into account, and the burden of metastatic disease needs to be considered,” he maintained. “The benefit of surgery at presentation is dependent on the completeness of resection, and axillary surgery and locoregional radiation therapy should be considered regardless of the metastasis.”
U.S. study: TBCRC 013
The second study – the Translational Breast Cancer Research Consortium’s study 013 – was presented by Tari A. King, MD, chief of breast surgery at the Dana-Farber Cancer Institute, associate division chief for breast surgery at Brigham and Women’s Hospital, and associate professor of surgery at Harvard Medical School, all in Boston.
The investigators analyzed data from the study’s cohort A, consisting of 112 patients with de novo stage IV breast cancer who had an intact primary tumor. All patients were given first-line systemic therapy; those who had a response were additionally offered elective resection of their primary tumor.
The median duration of follow-up was 54 months. Overall, 85% of the women had a response to their first-line therapy, Dr. King reported.
Some 43% of responders opted to undergo elective surgery to resect their primary tumor, defined as surgery performed in the absence of local symptoms or the need for local control, with specific type and extent left up to the treating physician.
In a multivariate analysis among responders surviving at least 6 months, median survival was 71 months with elective surgery and 65 months without it, a nonsignificant difference.
Findings were similar among subsets of women having estrogen receptor–positive tumors or HER2-positive tumors, and various combinations of these features.
In recursive partitioning analysis, response to first-line therapy, HER2 status, and age were the major determinants of survival.
“Importantly, although we were not able to demonstrate a survival benefit with the use of surgery, surgery also did not impact progression-free survival,” noted Dr. King.
Ultimately, 4% of responders who did not have elective surgery and 18% of nonresponders went on to have palliative resection of their primary.
“As this was a registry study, patients selected for surgery were more likely to have single-organ metastatic disease and to have received first-line chemotherapy, yet despite this selection bias, surgery did not impact survival in any tumor subtype,” Dr. King summarized. “Among patients who responded to therapy, HER2 status and patient age remained strong prognostic factors. Further investigation is needed to determine if subsets of patients will ultimately benefit from surgery.”
“In the absence of additional prospective data, our findings do not support surgery for the primary tumor outside of a clinical trial,” she concluded.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Resecting the primary tumor up front had a survival benefit, whereas resecting it after a response to systemic therapy did not.
Major finding: Compared with initial systemic therapy, initial resection of the primary tumor reduced the risk of death (HR, 0.66). But after a response to first-line therapy, median survival with elective resection was not significantly superior to that without it (71 vs. 65 months).
Data source: A randomized, controlled trial among 274 women with de novo stage IV breast cancer (MF07-01 trial) and a prospective registry study among 112 women with de novo stage IV breast cancer (TBCRC 013 study).
Disclosures: Dr. Soran disclosed that he has a consulting or advisory role with NanoVision. Dr. King disclosed that she had no relevant conflicts of interest.
Cabozantinib improves overall survival in renal cell carcinoma
CHICAGO – The oral multitargeted tyrosine kinase inhibitor cabozantinib confers an overall survival benefit to patients with previously treated renal cell carcinoma, compared with everolimus, according to the final survival analysis of the phase III METEOR trial.
An analysis of the 658 patients enrolled in the study revealed that “treatment with cabozantinib significantly improved overall survival, compared to everolimus. The median overall survival was 21.4 months in the cabozantinib group, compared to 16.5 months in the everolimus group,” Toni Choueiri, M.D., of the Dana-Farber Cancer Institute in Boston reported at the annual meeting of the American Society of Clinical Oncology.
”The hazard ratio of 0.66 does represent a 34% reduction in the rate of deaths,” he said.
An overall survival benefit associated with cabozantinib was consistently observed in all prespecified groups including the groups stratified by Memorial Sloan Kettering Cancer Center (MSKCC) risk criteria, the number and duration of prior vascular endothelial growth factor receptor tyrosine kinase inhibitor therapies, and tumor MET status.
An analysis of the same 658 patients enrolled in the METEOR trial, presented at the Genitourinary Cancers Symposium in early 2016, indicated cabozantinib improved progression-free survival, compared with everolimus (7.4 months vs. 3.9 months, HR, 0.52; P less than .001).
Cabozantinib is the only agent to demonstrate a significant benefit in overall survival, progression-free survival, and overall response rate in a phase III trial in previously treated patients with advanced renal cell carcinoma, according to Dr. Choueiri. “Cabozantinib is an important new treatment option for these patients,” he said.
This study was funded by Exelixis. Dr. Choueiri reported serving in advisory roles and receiving research funding and honoraria from multiple companies.
On Twitter @jessicolecraig
CHICAGO – The oral multitargeted tyrosine kinase inhibitor cabozantinib confers an overall survival benefit to patients with previously treated renal cell carcinoma, compared with everolimus, according to the final survival analysis of the phase III METEOR trial.
An analysis of the 658 patients enrolled in the study revealed that “treatment with cabozantinib significantly improved overall survival, compared to everolimus. The median overall survival was 21.4 months in the cabozantinib group, compared to 16.5 months in the everolimus group,” Toni Choueiri, M.D., of the Dana-Farber Cancer Institute in Boston reported at the annual meeting of the American Society of Clinical Oncology.
”The hazard ratio of 0.66 does represent a 34% reduction in the rate of deaths,” he said.
An overall survival benefit associated with cabozantinib was consistently observed in all prespecified groups including the groups stratified by Memorial Sloan Kettering Cancer Center (MSKCC) risk criteria, the number and duration of prior vascular endothelial growth factor receptor tyrosine kinase inhibitor therapies, and tumor MET status.
An analysis of the same 658 patients enrolled in the METEOR trial, presented at the Genitourinary Cancers Symposium in early 2016, indicated cabozantinib improved progression-free survival, compared with everolimus (7.4 months vs. 3.9 months, HR, 0.52; P less than .001).
Cabozantinib is the only agent to demonstrate a significant benefit in overall survival, progression-free survival, and overall response rate in a phase III trial in previously treated patients with advanced renal cell carcinoma, according to Dr. Choueiri. “Cabozantinib is an important new treatment option for these patients,” he said.
This study was funded by Exelixis. Dr. Choueiri reported serving in advisory roles and receiving research funding and honoraria from multiple companies.
On Twitter @jessicolecraig
CHICAGO – The oral multitargeted tyrosine kinase inhibitor cabozantinib confers an overall survival benefit to patients with previously treated renal cell carcinoma, compared with everolimus, according to the final survival analysis of the phase III METEOR trial.
An analysis of the 658 patients enrolled in the study revealed that “treatment with cabozantinib significantly improved overall survival, compared to everolimus. The median overall survival was 21.4 months in the cabozantinib group, compared to 16.5 months in the everolimus group,” Toni Choueiri, M.D., of the Dana-Farber Cancer Institute in Boston reported at the annual meeting of the American Society of Clinical Oncology.
”The hazard ratio of 0.66 does represent a 34% reduction in the rate of deaths,” he said.
An overall survival benefit associated with cabozantinib was consistently observed in all prespecified groups including the groups stratified by Memorial Sloan Kettering Cancer Center (MSKCC) risk criteria, the number and duration of prior vascular endothelial growth factor receptor tyrosine kinase inhibitor therapies, and tumor MET status.
An analysis of the same 658 patients enrolled in the METEOR trial, presented at the Genitourinary Cancers Symposium in early 2016, indicated cabozantinib improved progression-free survival, compared with everolimus (7.4 months vs. 3.9 months, HR, 0.52; P less than .001).
Cabozantinib is the only agent to demonstrate a significant benefit in overall survival, progression-free survival, and overall response rate in a phase III trial in previously treated patients with advanced renal cell carcinoma, according to Dr. Choueiri. “Cabozantinib is an important new treatment option for these patients,” he said.
This study was funded by Exelixis. Dr. Choueiri reported serving in advisory roles and receiving research funding and honoraria from multiple companies.
On Twitter @jessicolecraig
FROM 2016 ASCO ANNUAL MEETING
Key clinical point: Cabozantinib significantly improved overall survival, compared with everolimus in patients with renal cell carcinoma.
Major finding: For cabozantinib the median overall survival was 21.4 months, compared with 16.5 months in the everolimus group (HR, 0.66; 95% CI, 0.53-0.83; P = .0003).
Data source: A survival analysis of 658 patients with previously treated advanced renal cell carcinoma enrolled in the randomized phase III METEOR trial.
Disclosures: This study was funded by Exelixis. Dr. Choueiri reported serving in advisory roles and receiving research funding and honoraria from multiple companies.
Pembrolizumab-ipilimumab combo is highly active in advanced melanoma
CHICAGO – The combination of pembrolizumab, an antibody to the human cell surface receptor programmed death-1 (PD-1), and ipilimumab, an antibody to the human T-cell receptor cytotoxic T-lymphocyte-associated antigen 4 (CTLA4), is highly active against advanced melanoma and has acceptable safety, finds the KEYNOTE 029 trial’s expansion cohort.
The 153 patients in the cohort received a standard dose of pembrolizumab (2 mg/kg every 3 weeks) with a reduced dose of ipilimumab (1 mg/kg every 3 weeks for four doses) on the basis of earlier data showing substantial toxicity when a standard dose of ipilimumab was combined with other immune checkpoint inhibitors.
Results reported at the annual meeting of the American Society of Clinical Oncology showed that the overall response rate was 57%, and the disease control rate was 78%. Although 42% of patients experienced grade 3 or 4 treatment-related adverse events, most of these events resolved, and there were no treatment-related deaths.
“Pembrolizumab 2 mg/kg in combination with four doses of ipilimumab 1 mg/kg has a manageable toxicity profile and provides robust antitumor activity in patients with advanced melanoma,” concluded the investigators, who were led by Georgina Long, PhD, MBBS, chair of Melanoma Medical Oncology and Translational Research at the Melanoma Institute Australia and Royal North Shore Hospital, University of Sydney.
The response rate seen in KEYNOTE 029 was almost identical to that seen in the CheckMate 067 trial with the combination of nivolumab and standard-dose ipilimumab (3 mg/kg every 3 weeks for four doses), noted invited discussant Marc S. Ernstoff, MD, professor and chair of the department of medicine at the Roswell Park Cancer Institute in Buffalo, N.Y. It was also “remarkably comparable” to the 69% seen in the COMBI-d melanoma trial with the combination of dabrafenib (a BRAF inhibitor) and trametinib (an inhibitor of MEK MAPK/ERK kinase).
“There is a significant amount of grade 3 and 4 toxicity, but the dose of ipilimumab appeared to decrease this in the pembrolizumab-ipilimumab study compared to the nivolumab-ipilimumab study,” he noted. “There was a high percent of low-grade toxicities reported in all of these studies, and I would argue that as we are seeing patients survive longer, these low-grade toxicities are going to become more of an issue for us as oncologists to be able to deal with in terms of quality of life for patients surviving.”
There is good rationale for combining CTLA4 blockade and PD1 (or PD-L1) blockade in melanoma, Dr. Long maintained when introducing the research. “We know that CTLA inhibition at the priming phase in the periphery, at antigen presentation, is effective, as is PD-1 or PD-L1 [inhibition] at the effector phase down in the tumor bed,” she elaborated.
The patients with advanced melanoma enrolled in the expansion cohort could have received any number of prior therapies other than immune checkpoint inhibitors. However, in 87%, the study regimen was their first therapy.
At the time of data cutoff, 72% of patients had received all four planned doses of ipilimumab (Yervoy), and 56% were continuing on pembrolizumab (Keytruda).
The rates of any-grade and grade 3 or 4 treatment-related adverse events were 95% and 42%, respectively. The corresponding rates of immune-mediated adverse events were 58% and 25%.
The most common grade 3 or 4 treatment-related adverse events were lipase elevation (14%) and rash (3%). The former was asymptomatic and had no sequelae in the majority of cases, Dr. Long reported.
Hepatitis, colitis, and skin reactions were the most common grade 3 or 4 immune-mediated adverse events. The majority of immune-mediated adverse events were managed with systemic treatment, usually corticosteroids, and resolved.
When it came to efficacy, the overall response rate with the combination was similar across subgroups of patients stratified by PD-L1 status in the tumor and adjacent immune tissue, treatment history, baseline lactate dehydrogenase level, and BRAF mutational status.
Responses were ongoing in 98% of patients at data cutoff, with the duration of response ranging from about 6 weeks to 43 weeks, Dr. Long said. The disease control rate was 78%.
With a median follow-up of 10.0 months, median progression-free survival and overall survival were not yet reached. However, the 6-month rates of these outcomes were 70% and 93%, respectively.
Dr. Long disclosed that she is a consultant/adviser to Amgen, Bristol-Myers Squibb, Merck, Novartis, Provectus, and Roche, and that she has received honoraria from Bristol-Myers Squibb, Merck, and Novartis. The trial was supported by Merck.
CHICAGO – The combination of pembrolizumab, an antibody to the human cell surface receptor programmed death-1 (PD-1), and ipilimumab, an antibody to the human T-cell receptor cytotoxic T-lymphocyte-associated antigen 4 (CTLA4), is highly active against advanced melanoma and has acceptable safety, finds the KEYNOTE 029 trial’s expansion cohort.
The 153 patients in the cohort received a standard dose of pembrolizumab (2 mg/kg every 3 weeks) with a reduced dose of ipilimumab (1 mg/kg every 3 weeks for four doses) on the basis of earlier data showing substantial toxicity when a standard dose of ipilimumab was combined with other immune checkpoint inhibitors.
Results reported at the annual meeting of the American Society of Clinical Oncology showed that the overall response rate was 57%, and the disease control rate was 78%. Although 42% of patients experienced grade 3 or 4 treatment-related adverse events, most of these events resolved, and there were no treatment-related deaths.
“Pembrolizumab 2 mg/kg in combination with four doses of ipilimumab 1 mg/kg has a manageable toxicity profile and provides robust antitumor activity in patients with advanced melanoma,” concluded the investigators, who were led by Georgina Long, PhD, MBBS, chair of Melanoma Medical Oncology and Translational Research at the Melanoma Institute Australia and Royal North Shore Hospital, University of Sydney.
The response rate seen in KEYNOTE 029 was almost identical to that seen in the CheckMate 067 trial with the combination of nivolumab and standard-dose ipilimumab (3 mg/kg every 3 weeks for four doses), noted invited discussant Marc S. Ernstoff, MD, professor and chair of the department of medicine at the Roswell Park Cancer Institute in Buffalo, N.Y. It was also “remarkably comparable” to the 69% seen in the COMBI-d melanoma trial with the combination of dabrafenib (a BRAF inhibitor) and trametinib (an inhibitor of MEK MAPK/ERK kinase).
“There is a significant amount of grade 3 and 4 toxicity, but the dose of ipilimumab appeared to decrease this in the pembrolizumab-ipilimumab study compared to the nivolumab-ipilimumab study,” he noted. “There was a high percent of low-grade toxicities reported in all of these studies, and I would argue that as we are seeing patients survive longer, these low-grade toxicities are going to become more of an issue for us as oncologists to be able to deal with in terms of quality of life for patients surviving.”
There is good rationale for combining CTLA4 blockade and PD1 (or PD-L1) blockade in melanoma, Dr. Long maintained when introducing the research. “We know that CTLA inhibition at the priming phase in the periphery, at antigen presentation, is effective, as is PD-1 or PD-L1 [inhibition] at the effector phase down in the tumor bed,” she elaborated.
The patients with advanced melanoma enrolled in the expansion cohort could have received any number of prior therapies other than immune checkpoint inhibitors. However, in 87%, the study regimen was their first therapy.
At the time of data cutoff, 72% of patients had received all four planned doses of ipilimumab (Yervoy), and 56% were continuing on pembrolizumab (Keytruda).
The rates of any-grade and grade 3 or 4 treatment-related adverse events were 95% and 42%, respectively. The corresponding rates of immune-mediated adverse events were 58% and 25%.
The most common grade 3 or 4 treatment-related adverse events were lipase elevation (14%) and rash (3%). The former was asymptomatic and had no sequelae in the majority of cases, Dr. Long reported.
Hepatitis, colitis, and skin reactions were the most common grade 3 or 4 immune-mediated adverse events. The majority of immune-mediated adverse events were managed with systemic treatment, usually corticosteroids, and resolved.
When it came to efficacy, the overall response rate with the combination was similar across subgroups of patients stratified by PD-L1 status in the tumor and adjacent immune tissue, treatment history, baseline lactate dehydrogenase level, and BRAF mutational status.
Responses were ongoing in 98% of patients at data cutoff, with the duration of response ranging from about 6 weeks to 43 weeks, Dr. Long said. The disease control rate was 78%.
With a median follow-up of 10.0 months, median progression-free survival and overall survival were not yet reached. However, the 6-month rates of these outcomes were 70% and 93%, respectively.
Dr. Long disclosed that she is a consultant/adviser to Amgen, Bristol-Myers Squibb, Merck, Novartis, Provectus, and Roche, and that she has received honoraria from Bristol-Myers Squibb, Merck, and Novartis. The trial was supported by Merck.
CHICAGO – The combination of pembrolizumab, an antibody to the human cell surface receptor programmed death-1 (PD-1), and ipilimumab, an antibody to the human T-cell receptor cytotoxic T-lymphocyte-associated antigen 4 (CTLA4), is highly active against advanced melanoma and has acceptable safety, finds the KEYNOTE 029 trial’s expansion cohort.
The 153 patients in the cohort received a standard dose of pembrolizumab (2 mg/kg every 3 weeks) with a reduced dose of ipilimumab (1 mg/kg every 3 weeks for four doses) on the basis of earlier data showing substantial toxicity when a standard dose of ipilimumab was combined with other immune checkpoint inhibitors.
Results reported at the annual meeting of the American Society of Clinical Oncology showed that the overall response rate was 57%, and the disease control rate was 78%. Although 42% of patients experienced grade 3 or 4 treatment-related adverse events, most of these events resolved, and there were no treatment-related deaths.
“Pembrolizumab 2 mg/kg in combination with four doses of ipilimumab 1 mg/kg has a manageable toxicity profile and provides robust antitumor activity in patients with advanced melanoma,” concluded the investigators, who were led by Georgina Long, PhD, MBBS, chair of Melanoma Medical Oncology and Translational Research at the Melanoma Institute Australia and Royal North Shore Hospital, University of Sydney.
The response rate seen in KEYNOTE 029 was almost identical to that seen in the CheckMate 067 trial with the combination of nivolumab and standard-dose ipilimumab (3 mg/kg every 3 weeks for four doses), noted invited discussant Marc S. Ernstoff, MD, professor and chair of the department of medicine at the Roswell Park Cancer Institute in Buffalo, N.Y. It was also “remarkably comparable” to the 69% seen in the COMBI-d melanoma trial with the combination of dabrafenib (a BRAF inhibitor) and trametinib (an inhibitor of MEK MAPK/ERK kinase).
“There is a significant amount of grade 3 and 4 toxicity, but the dose of ipilimumab appeared to decrease this in the pembrolizumab-ipilimumab study compared to the nivolumab-ipilimumab study,” he noted. “There was a high percent of low-grade toxicities reported in all of these studies, and I would argue that as we are seeing patients survive longer, these low-grade toxicities are going to become more of an issue for us as oncologists to be able to deal with in terms of quality of life for patients surviving.”
There is good rationale for combining CTLA4 blockade and PD1 (or PD-L1) blockade in melanoma, Dr. Long maintained when introducing the research. “We know that CTLA inhibition at the priming phase in the periphery, at antigen presentation, is effective, as is PD-1 or PD-L1 [inhibition] at the effector phase down in the tumor bed,” she elaborated.
The patients with advanced melanoma enrolled in the expansion cohort could have received any number of prior therapies other than immune checkpoint inhibitors. However, in 87%, the study regimen was their first therapy.
At the time of data cutoff, 72% of patients had received all four planned doses of ipilimumab (Yervoy), and 56% were continuing on pembrolizumab (Keytruda).
The rates of any-grade and grade 3 or 4 treatment-related adverse events were 95% and 42%, respectively. The corresponding rates of immune-mediated adverse events were 58% and 25%.
The most common grade 3 or 4 treatment-related adverse events were lipase elevation (14%) and rash (3%). The former was asymptomatic and had no sequelae in the majority of cases, Dr. Long reported.
Hepatitis, colitis, and skin reactions were the most common grade 3 or 4 immune-mediated adverse events. The majority of immune-mediated adverse events were managed with systemic treatment, usually corticosteroids, and resolved.
When it came to efficacy, the overall response rate with the combination was similar across subgroups of patients stratified by PD-L1 status in the tumor and adjacent immune tissue, treatment history, baseline lactate dehydrogenase level, and BRAF mutational status.
Responses were ongoing in 98% of patients at data cutoff, with the duration of response ranging from about 6 weeks to 43 weeks, Dr. Long said. The disease control rate was 78%.
With a median follow-up of 10.0 months, median progression-free survival and overall survival were not yet reached. However, the 6-month rates of these outcomes were 70% and 93%, respectively.
Dr. Long disclosed that she is a consultant/adviser to Amgen, Bristol-Myers Squibb, Merck, Novartis, Provectus, and Roche, and that she has received honoraria from Bristol-Myers Squibb, Merck, and Novartis. The trial was supported by Merck.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Dual immune checkpoint blockade with pembrolizumab and ipilimumab is efficacious in advanced melanoma.
Major finding: The overall response rate was 57%, and the disease control rate was 78%.
Data source: An expansion cohort from a phase I/II trial among 153 patients with advanced melanoma (KEYNOTE 029).
Disclosures: Dr. Long disclosed that she is a consultant/advisor to Amgen, Bristol-Myers Squibb, Merck, Novartis, Provectus, and Roche, and that she has received honoraria from Bristol-Myers Squibb, Merck, and Novartis. The trial was supported by Merck.
Three-drug regimen boosts progression-free survival in patients with relapsed CLL and adverse prognostic features
Progression-free survival was improved for poor prognosis patients with relapsed chronic lymphocytic leukemia when idelalisib was added to bendamustine and rituximab, based on the results of a randomized, double-blind, placebo-controlled phase III study.
The findings support the three-drug approach as an important treatment option for patients with relapsed CLL and adverse prognostic features, but the regimen also was associated with more grade 3 or greater adverse events, primarily neutropenia and opportunistic infections, that led to more study drug discontinuation, Jacqueline Claudia Barrientos, M.D., and her colleagues reported at the annual meeting of the American Society of Clinical Oncology.
The overall response rates were 68% in the three-drug group and 45% in the two-drug plus placebo group.
For the study, 416 patients were stratified based on whether they had 17p deletions or TP53 mutations, their IGHV mutation status, and whether they had refractory or relapsed disease. The 207 patients who received idelalisib, bendamustine, and rituximab had consistently better progression-free survival than the 209 patients who received placebo, bendamustine, and rituximab. The median progression-free survival was 23 months in the group that received idelalisib and 11 months in the group that received placebo, with an overall hazard ratio of 0.33 at a median follow-up of 12 months.
For those with 17p deletions or TP53 mutations, the median progression-free survival was 11 months with the three-drug regimen and 8 months for the two-drug plus placebo regimen. For those with neither of these abnormalities, progression-free survival was more than 24 months for patients given the three active drugs and 11 months for patients given two drugs plus placebo.
For those with the 11q deletion, median progression-free survival was 23 months with idelalisib, bendamustine, and rituximab and 9 months with placebo, bendamustine, and rituximab, said Dr. Barrientos of Hofstra University, Hempstead, N.Y.
For those with IGHV mutations, the median progression-free survival has not been reached in the idelalisib, bendamustine, and rituximab group and was 11 months in the placebo, bendamustine, and rituximab group.
Among patients with tumor burdens exceeding 5 cm, median progression-free survival was 23 months with idelalisib, bendamustine, and rituximab and about 10 months with placebo, bendamustine, and rituximab.
Grade 3 or greater adverse events affected 97% of patients given the three active drugs and 76% of patients given bendamustine and rituximab plus placebo. Adverse events resulted in drug dose reductions in 11% of those given the three active drugs and in 6% of those given bendamustine and rituximab plus placebo. The study drug was discontinued in 26% of those in the idelalisib, bendamustine, and rituximab group and in 13% of the placebo, bendamustine, and rituximab group. Death occurred in 10% of the study patients given idelalisib, bendamustine, and rituximab and in 7% of the patients given placebo, bendamustine, and rituximab.
To be eligible for the study (NCT01569295), patients needed to have previously treated recurrent CLL, have measurable lymphadenopathy, require therapy for CLL, and have experienced CLL progression for less than 36 months since the completion of their last prior therapy.
The treatment regimen consisted of 6 cycles every 28 days of bendamustine (70 mg/m2 on day 1 and day 2 of each cycle), rituximab (375 mg/m2 in cycle 1 and 500 mg/m2 in cycles 2-6), and idelalisib (150 mg twice daily) or placebo. Idelalisib or placebo was continued until an independent review committee confirmed disease progression, death, intolerable toxicity, or withdrawal of consent.
The study was sponsored by Gilead Sciences, the maker of idelalisib (Zydelig). Dr. Barrientos receives research funding from Gilead Sciences and Abbvie, and serves as a consultant or adviser to Celgene, Genentech, and Pharmacyclics.
On Twitter @maryjodales
Progression-free survival was improved for poor prognosis patients with relapsed chronic lymphocytic leukemia when idelalisib was added to bendamustine and rituximab, based on the results of a randomized, double-blind, placebo-controlled phase III study.
The findings support the three-drug approach as an important treatment option for patients with relapsed CLL and adverse prognostic features, but the regimen also was associated with more grade 3 or greater adverse events, primarily neutropenia and opportunistic infections, that led to more study drug discontinuation, Jacqueline Claudia Barrientos, M.D., and her colleagues reported at the annual meeting of the American Society of Clinical Oncology.
The overall response rates were 68% in the three-drug group and 45% in the two-drug plus placebo group.
For the study, 416 patients were stratified based on whether they had 17p deletions or TP53 mutations, their IGHV mutation status, and whether they had refractory or relapsed disease. The 207 patients who received idelalisib, bendamustine, and rituximab had consistently better progression-free survival than the 209 patients who received placebo, bendamustine, and rituximab. The median progression-free survival was 23 months in the group that received idelalisib and 11 months in the group that received placebo, with an overall hazard ratio of 0.33 at a median follow-up of 12 months.
For those with 17p deletions or TP53 mutations, the median progression-free survival was 11 months with the three-drug regimen and 8 months for the two-drug plus placebo regimen. For those with neither of these abnormalities, progression-free survival was more than 24 months for patients given the three active drugs and 11 months for patients given two drugs plus placebo.
For those with the 11q deletion, median progression-free survival was 23 months with idelalisib, bendamustine, and rituximab and 9 months with placebo, bendamustine, and rituximab, said Dr. Barrientos of Hofstra University, Hempstead, N.Y.
For those with IGHV mutations, the median progression-free survival has not been reached in the idelalisib, bendamustine, and rituximab group and was 11 months in the placebo, bendamustine, and rituximab group.
Among patients with tumor burdens exceeding 5 cm, median progression-free survival was 23 months with idelalisib, bendamustine, and rituximab and about 10 months with placebo, bendamustine, and rituximab.
Grade 3 or greater adverse events affected 97% of patients given the three active drugs and 76% of patients given bendamustine and rituximab plus placebo. Adverse events resulted in drug dose reductions in 11% of those given the three active drugs and in 6% of those given bendamustine and rituximab plus placebo. The study drug was discontinued in 26% of those in the idelalisib, bendamustine, and rituximab group and in 13% of the placebo, bendamustine, and rituximab group. Death occurred in 10% of the study patients given idelalisib, bendamustine, and rituximab and in 7% of the patients given placebo, bendamustine, and rituximab.
To be eligible for the study (NCT01569295), patients needed to have previously treated recurrent CLL, have measurable lymphadenopathy, require therapy for CLL, and have experienced CLL progression for less than 36 months since the completion of their last prior therapy.
The treatment regimen consisted of 6 cycles every 28 days of bendamustine (70 mg/m2 on day 1 and day 2 of each cycle), rituximab (375 mg/m2 in cycle 1 and 500 mg/m2 in cycles 2-6), and idelalisib (150 mg twice daily) or placebo. Idelalisib or placebo was continued until an independent review committee confirmed disease progression, death, intolerable toxicity, or withdrawal of consent.
The study was sponsored by Gilead Sciences, the maker of idelalisib (Zydelig). Dr. Barrientos receives research funding from Gilead Sciences and Abbvie, and serves as a consultant or adviser to Celgene, Genentech, and Pharmacyclics.
On Twitter @maryjodales
Progression-free survival was improved for poor prognosis patients with relapsed chronic lymphocytic leukemia when idelalisib was added to bendamustine and rituximab, based on the results of a randomized, double-blind, placebo-controlled phase III study.
The findings support the three-drug approach as an important treatment option for patients with relapsed CLL and adverse prognostic features, but the regimen also was associated with more grade 3 or greater adverse events, primarily neutropenia and opportunistic infections, that led to more study drug discontinuation, Jacqueline Claudia Barrientos, M.D., and her colleagues reported at the annual meeting of the American Society of Clinical Oncology.
The overall response rates were 68% in the three-drug group and 45% in the two-drug plus placebo group.
For the study, 416 patients were stratified based on whether they had 17p deletions or TP53 mutations, their IGHV mutation status, and whether they had refractory or relapsed disease. The 207 patients who received idelalisib, bendamustine, and rituximab had consistently better progression-free survival than the 209 patients who received placebo, bendamustine, and rituximab. The median progression-free survival was 23 months in the group that received idelalisib and 11 months in the group that received placebo, with an overall hazard ratio of 0.33 at a median follow-up of 12 months.
For those with 17p deletions or TP53 mutations, the median progression-free survival was 11 months with the three-drug regimen and 8 months for the two-drug plus placebo regimen. For those with neither of these abnormalities, progression-free survival was more than 24 months for patients given the three active drugs and 11 months for patients given two drugs plus placebo.
For those with the 11q deletion, median progression-free survival was 23 months with idelalisib, bendamustine, and rituximab and 9 months with placebo, bendamustine, and rituximab, said Dr. Barrientos of Hofstra University, Hempstead, N.Y.
For those with IGHV mutations, the median progression-free survival has not been reached in the idelalisib, bendamustine, and rituximab group and was 11 months in the placebo, bendamustine, and rituximab group.
Among patients with tumor burdens exceeding 5 cm, median progression-free survival was 23 months with idelalisib, bendamustine, and rituximab and about 10 months with placebo, bendamustine, and rituximab.
Grade 3 or greater adverse events affected 97% of patients given the three active drugs and 76% of patients given bendamustine and rituximab plus placebo. Adverse events resulted in drug dose reductions in 11% of those given the three active drugs and in 6% of those given bendamustine and rituximab plus placebo. The study drug was discontinued in 26% of those in the idelalisib, bendamustine, and rituximab group and in 13% of the placebo, bendamustine, and rituximab group. Death occurred in 10% of the study patients given idelalisib, bendamustine, and rituximab and in 7% of the patients given placebo, bendamustine, and rituximab.
To be eligible for the study (NCT01569295), patients needed to have previously treated recurrent CLL, have measurable lymphadenopathy, require therapy for CLL, and have experienced CLL progression for less than 36 months since the completion of their last prior therapy.
The treatment regimen consisted of 6 cycles every 28 days of bendamustine (70 mg/m2 on day 1 and day 2 of each cycle), rituximab (375 mg/m2 in cycle 1 and 500 mg/m2 in cycles 2-6), and idelalisib (150 mg twice daily) or placebo. Idelalisib or placebo was continued until an independent review committee confirmed disease progression, death, intolerable toxicity, or withdrawal of consent.
The study was sponsored by Gilead Sciences, the maker of idelalisib (Zydelig). Dr. Barrientos receives research funding from Gilead Sciences and Abbvie, and serves as a consultant or adviser to Celgene, Genentech, and Pharmacyclics.
On Twitter @maryjodales
FROM 2016 ASCO ANNUAL MEETING
Key clinical point: Progression-free survival was improved for poor prognosis patients with relapsed chronic lymphocytic leukemia when idelalisib was added to bendamustine, and rituximab.
Major finding: The median progression-free survival was 23 months in the group that received idelalisib and 11 months in the group that received placebo, with an overall hazard ratio of 0.33 at a median follow-up of 12 months.
Data source: A randomized, double-blind, placebo-controlled phase III study of 416 patients stratified on the basis of 17p deletions or TP53 mutations, IGHV mutation status, and whether they had refractory or relapsed disease.
Disclosures: The study was sponsored by Gilead Sciences, the maker of idelalisib (Zydelig). Dr. Barrientos receives research funding from Gilead Sciences and Abbvie, and serves as a consultant or adviser to Celgene, Genentech, and Pharmacyclics.
Safety of sentinel node dissection alone holds up a decade out
CHICAGO – Women with clinical early-stage breast cancer and a positive sentinel lymph node who receive breast-conserving therapy can safely skip an axillary lymph node dissection (ALND), and therefore avoid its associated morbidity, confirms long-term follow-up of the Z0011 trial conducted by the American College of Surgeons Oncology Group and the Alliance for Clinical Trials in Oncology.
The phase III trial enrolled 891 women with clinical T1-2,N0,M0 disease who underwent lumpectomy and were found to have sentinel node involvement. They were randomized to ALND or no further surgery, followed by whole-breast radiation therapy and, in most cases, systemic adjuvant therapy.
The trial was closed early because of low rates of accrual and events. Results at 6.3 years of follow-up showed that compared with peers who had an ALND, the women who skipped this surgery did not have inferior 5-year rates of locoregional recurrence or overall survival (JAMA. 2011;305:569-75).
“The study, however, like most breast cancer studies, contained mostly postmenopausal women with hormone receptor–positive tumors who are known to have late recurrences, and it was criticized for short follow-up,” commented first author Armando E. Giuliano, MD, executive vice chair of surgical oncology in the department of surgery, and associate director of surgical oncology in the Samuel Oschin Comprehensive Cancer Institute, Los Angeles.
In an update of the findings, now with a median follow-up of 9.3 years, the groups were statistically indistinguishable with respect to 10-year rates of the same outcomes, he reported at the annual meeting of the American Society of Clinical Oncology.
“This study... shows that sentinel node biopsy alone provides excellent 10-year locoregional control and survival comparable to completion axillary lymph node dissection for these patients, even with long-term follow-up,” he maintained. “Routine use of axillary lymph node dissection should be abandoned.”
“This was designed as a noninferiority trial, and I would suggest that based on the data we have seen, even if they had hit their target accrual, the outcomes would not be different,” said invited discussant Elizabeth A. Mittendorf, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston. “Clearly, even before today’s presentation, Z0011 has been identified as a practice-changing trial, as evidenced by the NCCN guidelines.”
In fact, a study last year showed that among patients in the general U.S. population meeting the trial’s enrollment criteria, the use of sentinel lymph node dissection alone has increased significantly since the Z0011 results were first reported (J Am Coll Surg. 2015;221:71-81).
“However, I would highlight that we have also seen an increase in omission of axillary lymph node dissection for patients who do not meet the Z0011 criteria to include those not planned for radiotherapy, those receiving APBI [accelerated partial breast irradiation], and those undergoing mastectomy,” she added. “I highlight these examples specifically because it’s been suggested that one of the reasons the patients on the trial have outstanding regional control is because of the radiation administered as part of their breast-conserving therapy.”
“We will obtain additional data on the locoregional management of these early-stage patients with clinically node-negative breast cancer,” Dr. Mittendorf predicted, pointing to the similar POSNOC trial (which is comparing systemic therapy with versus without axillary treatment) and SOUND trial (which is comparing sentinel node dissection versus no axillary surgery).
In Z0011, all women had tumor in sentinel nodes detected with hematoxylin and eosin staining. Those with sentinel node tumor detected only by immunohistochemistry were excluded, as were those who had matted nodes, three or more involved sentinel nodes, or planned third-field (nodal) irradiation.
Overall, 27.4% of the patients in the ALND group had additional positive nodes removed beyond their sentinel nodes. “There is no reason to suspect that women with sentinel node biopsy [only] had fewer involved nodes than the women treated with axillary lymph node dissection,” Dr. Giuliano commented; thus, a similar share of the former group likely had residual axillary disease that went unresected.
The updated findings showed that the women received ALND and the women who did not were statistically indistinguishable with respect to the 10-year rate of locoregional recurrence (6.2% and 5.3%). Of note, only a single regional recurrence was seen after the initial 5 years of follow-up, and it occurred in the group that did not have ALND.
The groups treated with and without ALND were also statistically indistinguishable with respect to 10-year rates of disease-free survival (78.2% and 80.2%), locoregional recurrence–free survival (81.2% and 83.0%), and overall survival (83.6% and 86.3%).
In multivariate analysis, omission of ALND did not significantly predict locoregional recurrence or overall survival, reported Dr. Giuliano. Additionally, stratified analysis showed that the lack of difference in overall survival between study groups was the same whether tumors had hormone receptors or not.
In a related analysis of radiation protocol deviations in a subset of women from the trial, 11% did not receive any radiation therapy, while 18.9% received third-field radiation, with equal distribution of the latter between study groups (J Clin Oncol. 2014;32:3600-6). Omission of radiation was associated with an increased risk of local recurrence and death, but it did not affect nodal recurrences. Receipt of third-field radiation did not influence survival.
CHICAGO – Women with clinical early-stage breast cancer and a positive sentinel lymph node who receive breast-conserving therapy can safely skip an axillary lymph node dissection (ALND), and therefore avoid its associated morbidity, confirms long-term follow-up of the Z0011 trial conducted by the American College of Surgeons Oncology Group and the Alliance for Clinical Trials in Oncology.
The phase III trial enrolled 891 women with clinical T1-2,N0,M0 disease who underwent lumpectomy and were found to have sentinel node involvement. They were randomized to ALND or no further surgery, followed by whole-breast radiation therapy and, in most cases, systemic adjuvant therapy.
The trial was closed early because of low rates of accrual and events. Results at 6.3 years of follow-up showed that compared with peers who had an ALND, the women who skipped this surgery did not have inferior 5-year rates of locoregional recurrence or overall survival (JAMA. 2011;305:569-75).
“The study, however, like most breast cancer studies, contained mostly postmenopausal women with hormone receptor–positive tumors who are known to have late recurrences, and it was criticized for short follow-up,” commented first author Armando E. Giuliano, MD, executive vice chair of surgical oncology in the department of surgery, and associate director of surgical oncology in the Samuel Oschin Comprehensive Cancer Institute, Los Angeles.
In an update of the findings, now with a median follow-up of 9.3 years, the groups were statistically indistinguishable with respect to 10-year rates of the same outcomes, he reported at the annual meeting of the American Society of Clinical Oncology.
“This study... shows that sentinel node biopsy alone provides excellent 10-year locoregional control and survival comparable to completion axillary lymph node dissection for these patients, even with long-term follow-up,” he maintained. “Routine use of axillary lymph node dissection should be abandoned.”
“This was designed as a noninferiority trial, and I would suggest that based on the data we have seen, even if they had hit their target accrual, the outcomes would not be different,” said invited discussant Elizabeth A. Mittendorf, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston. “Clearly, even before today’s presentation, Z0011 has been identified as a practice-changing trial, as evidenced by the NCCN guidelines.”
In fact, a study last year showed that among patients in the general U.S. population meeting the trial’s enrollment criteria, the use of sentinel lymph node dissection alone has increased significantly since the Z0011 results were first reported (J Am Coll Surg. 2015;221:71-81).
“However, I would highlight that we have also seen an increase in omission of axillary lymph node dissection for patients who do not meet the Z0011 criteria to include those not planned for radiotherapy, those receiving APBI [accelerated partial breast irradiation], and those undergoing mastectomy,” she added. “I highlight these examples specifically because it’s been suggested that one of the reasons the patients on the trial have outstanding regional control is because of the radiation administered as part of their breast-conserving therapy.”
“We will obtain additional data on the locoregional management of these early-stage patients with clinically node-negative breast cancer,” Dr. Mittendorf predicted, pointing to the similar POSNOC trial (which is comparing systemic therapy with versus without axillary treatment) and SOUND trial (which is comparing sentinel node dissection versus no axillary surgery).
In Z0011, all women had tumor in sentinel nodes detected with hematoxylin and eosin staining. Those with sentinel node tumor detected only by immunohistochemistry were excluded, as were those who had matted nodes, three or more involved sentinel nodes, or planned third-field (nodal) irradiation.
Overall, 27.4% of the patients in the ALND group had additional positive nodes removed beyond their sentinel nodes. “There is no reason to suspect that women with sentinel node biopsy [only] had fewer involved nodes than the women treated with axillary lymph node dissection,” Dr. Giuliano commented; thus, a similar share of the former group likely had residual axillary disease that went unresected.
The updated findings showed that the women received ALND and the women who did not were statistically indistinguishable with respect to the 10-year rate of locoregional recurrence (6.2% and 5.3%). Of note, only a single regional recurrence was seen after the initial 5 years of follow-up, and it occurred in the group that did not have ALND.
The groups treated with and without ALND were also statistically indistinguishable with respect to 10-year rates of disease-free survival (78.2% and 80.2%), locoregional recurrence–free survival (81.2% and 83.0%), and overall survival (83.6% and 86.3%).
In multivariate analysis, omission of ALND did not significantly predict locoregional recurrence or overall survival, reported Dr. Giuliano. Additionally, stratified analysis showed that the lack of difference in overall survival between study groups was the same whether tumors had hormone receptors or not.
In a related analysis of radiation protocol deviations in a subset of women from the trial, 11% did not receive any radiation therapy, while 18.9% received third-field radiation, with equal distribution of the latter between study groups (J Clin Oncol. 2014;32:3600-6). Omission of radiation was associated with an increased risk of local recurrence and death, but it did not affect nodal recurrences. Receipt of third-field radiation did not influence survival.
CHICAGO – Women with clinical early-stage breast cancer and a positive sentinel lymph node who receive breast-conserving therapy can safely skip an axillary lymph node dissection (ALND), and therefore avoid its associated morbidity, confirms long-term follow-up of the Z0011 trial conducted by the American College of Surgeons Oncology Group and the Alliance for Clinical Trials in Oncology.
The phase III trial enrolled 891 women with clinical T1-2,N0,M0 disease who underwent lumpectomy and were found to have sentinel node involvement. They were randomized to ALND or no further surgery, followed by whole-breast radiation therapy and, in most cases, systemic adjuvant therapy.
The trial was closed early because of low rates of accrual and events. Results at 6.3 years of follow-up showed that compared with peers who had an ALND, the women who skipped this surgery did not have inferior 5-year rates of locoregional recurrence or overall survival (JAMA. 2011;305:569-75).
“The study, however, like most breast cancer studies, contained mostly postmenopausal women with hormone receptor–positive tumors who are known to have late recurrences, and it was criticized for short follow-up,” commented first author Armando E. Giuliano, MD, executive vice chair of surgical oncology in the department of surgery, and associate director of surgical oncology in the Samuel Oschin Comprehensive Cancer Institute, Los Angeles.
In an update of the findings, now with a median follow-up of 9.3 years, the groups were statistically indistinguishable with respect to 10-year rates of the same outcomes, he reported at the annual meeting of the American Society of Clinical Oncology.
“This study... shows that sentinel node biopsy alone provides excellent 10-year locoregional control and survival comparable to completion axillary lymph node dissection for these patients, even with long-term follow-up,” he maintained. “Routine use of axillary lymph node dissection should be abandoned.”
“This was designed as a noninferiority trial, and I would suggest that based on the data we have seen, even if they had hit their target accrual, the outcomes would not be different,” said invited discussant Elizabeth A. Mittendorf, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston. “Clearly, even before today’s presentation, Z0011 has been identified as a practice-changing trial, as evidenced by the NCCN guidelines.”
In fact, a study last year showed that among patients in the general U.S. population meeting the trial’s enrollment criteria, the use of sentinel lymph node dissection alone has increased significantly since the Z0011 results were first reported (J Am Coll Surg. 2015;221:71-81).
“However, I would highlight that we have also seen an increase in omission of axillary lymph node dissection for patients who do not meet the Z0011 criteria to include those not planned for radiotherapy, those receiving APBI [accelerated partial breast irradiation], and those undergoing mastectomy,” she added. “I highlight these examples specifically because it’s been suggested that one of the reasons the patients on the trial have outstanding regional control is because of the radiation administered as part of their breast-conserving therapy.”
“We will obtain additional data on the locoregional management of these early-stage patients with clinically node-negative breast cancer,” Dr. Mittendorf predicted, pointing to the similar POSNOC trial (which is comparing systemic therapy with versus without axillary treatment) and SOUND trial (which is comparing sentinel node dissection versus no axillary surgery).
In Z0011, all women had tumor in sentinel nodes detected with hematoxylin and eosin staining. Those with sentinel node tumor detected only by immunohistochemistry were excluded, as were those who had matted nodes, three or more involved sentinel nodes, or planned third-field (nodal) irradiation.
Overall, 27.4% of the patients in the ALND group had additional positive nodes removed beyond their sentinel nodes. “There is no reason to suspect that women with sentinel node biopsy [only] had fewer involved nodes than the women treated with axillary lymph node dissection,” Dr. Giuliano commented; thus, a similar share of the former group likely had residual axillary disease that went unresected.
The updated findings showed that the women received ALND and the women who did not were statistically indistinguishable with respect to the 10-year rate of locoregional recurrence (6.2% and 5.3%). Of note, only a single regional recurrence was seen after the initial 5 years of follow-up, and it occurred in the group that did not have ALND.
The groups treated with and without ALND were also statistically indistinguishable with respect to 10-year rates of disease-free survival (78.2% and 80.2%), locoregional recurrence–free survival (81.2% and 83.0%), and overall survival (83.6% and 86.3%).
In multivariate analysis, omission of ALND did not significantly predict locoregional recurrence or overall survival, reported Dr. Giuliano. Additionally, stratified analysis showed that the lack of difference in overall survival between study groups was the same whether tumors had hormone receptors or not.
In a related analysis of radiation protocol deviations in a subset of women from the trial, 11% did not receive any radiation therapy, while 18.9% received third-field radiation, with equal distribution of the latter between study groups (J Clin Oncol. 2014;32:3600-6). Omission of radiation was associated with an increased risk of local recurrence and death, but it did not affect nodal recurrences. Receipt of third-field radiation did not influence survival.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: In women with clinical early-stage breast cancer who have a positive sentinel node and undergo breast-conserving therapy, skipping ALND does not compromise outcomes.
Major finding: Women treated with and without ALND were statistically indistinguishable with respect to 10-year rates of locoregional recurrence (6.2% and 5.3%), disease-free survival (78.2% and 80.2%), and overall survival (83.6% and 86.3%).
Data source: A randomized phase III trial among 891 women with clinical T1-2,N0,M0 breast cancer and positive sentinel nodes treated with breast-conserving therapy and usually adjuvant systemic therapy (ACOSOG Z0011).
Disclosures: Dr. Giuliano disclosed that he had no relevant conflicts of interest.
Smoldering multiple myeloma affects 1 in 7 patients
About 1 in 7 cases of multiple myeloma diagnosed in the United States are cases of smoldering disease, according to an analysis of data from the National Cancer Data Base, which represents 70% of cancer cases.
The prevalence of smoldering multiple myeloma varied among various socio- and geodemographic subgroups, but overall survival did not, Aishwarya Ravindran, MBBS, of Mayo Clinic, Rochester, Minn., and colleagues reported at the annual meeting of the American Society of Clinical Oncology. “Our results can be used in the future to study the health care impact of SMM,” the researchers wrote in a poster presentation.
Epidemiologic studies of smoldering multiple myeloma have been limited by the lack of International Classification of Diseases codes specific for smoldering status, the researchers said.
They analyzed 86,327 cases of multiple myeloma, considering socio- and geodemographic subgroups and type of treatment facility. Overall survival was compared for smoldering and active multiple myeloma. The researchers included patients enrolled in the database during 2003-2011; records were examined from the time to initial treatment and they considered reasons for patients not receiving treatment.
Patients who did not require treatment within the first 120 days after diagnosis were considered to have smoldering disease. This group comprised almost 14% of the cases.
The proportion of cases that were smoldering disease did not change significantly during the study period (P = .23 and .34, respectively). Smoldering disease was more likely to be diagnosed among women, black patients, older patients (median age at diagnosis was 67 years), and less educated patients. Smoldering disease was more common in patients with fewer medical comorbidities, those living closer to a treatment facility, and those evaluated for their disease in the Northeast United States. The proportions of cases diagnosed at academic and nonacademic facilities were similar.
The median overall survival for smoldering disease was 63 months; for active disease, 33 months. Overall survival in those with smoldering disease did not differ among the racial groups (P = .27).
The researchers had no financial conflicts.
On Twitter @maryjodales
About 1 in 7 cases of multiple myeloma diagnosed in the United States are cases of smoldering disease, according to an analysis of data from the National Cancer Data Base, which represents 70% of cancer cases.
The prevalence of smoldering multiple myeloma varied among various socio- and geodemographic subgroups, but overall survival did not, Aishwarya Ravindran, MBBS, of Mayo Clinic, Rochester, Minn., and colleagues reported at the annual meeting of the American Society of Clinical Oncology. “Our results can be used in the future to study the health care impact of SMM,” the researchers wrote in a poster presentation.
Epidemiologic studies of smoldering multiple myeloma have been limited by the lack of International Classification of Diseases codes specific for smoldering status, the researchers said.
They analyzed 86,327 cases of multiple myeloma, considering socio- and geodemographic subgroups and type of treatment facility. Overall survival was compared for smoldering and active multiple myeloma. The researchers included patients enrolled in the database during 2003-2011; records were examined from the time to initial treatment and they considered reasons for patients not receiving treatment.
Patients who did not require treatment within the first 120 days after diagnosis were considered to have smoldering disease. This group comprised almost 14% of the cases.
The proportion of cases that were smoldering disease did not change significantly during the study period (P = .23 and .34, respectively). Smoldering disease was more likely to be diagnosed among women, black patients, older patients (median age at diagnosis was 67 years), and less educated patients. Smoldering disease was more common in patients with fewer medical comorbidities, those living closer to a treatment facility, and those evaluated for their disease in the Northeast United States. The proportions of cases diagnosed at academic and nonacademic facilities were similar.
The median overall survival for smoldering disease was 63 months; for active disease, 33 months. Overall survival in those with smoldering disease did not differ among the racial groups (P = .27).
The researchers had no financial conflicts.
On Twitter @maryjodales
About 1 in 7 cases of multiple myeloma diagnosed in the United States are cases of smoldering disease, according to an analysis of data from the National Cancer Data Base, which represents 70% of cancer cases.
The prevalence of smoldering multiple myeloma varied among various socio- and geodemographic subgroups, but overall survival did not, Aishwarya Ravindran, MBBS, of Mayo Clinic, Rochester, Minn., and colleagues reported at the annual meeting of the American Society of Clinical Oncology. “Our results can be used in the future to study the health care impact of SMM,” the researchers wrote in a poster presentation.
Epidemiologic studies of smoldering multiple myeloma have been limited by the lack of International Classification of Diseases codes specific for smoldering status, the researchers said.
They analyzed 86,327 cases of multiple myeloma, considering socio- and geodemographic subgroups and type of treatment facility. Overall survival was compared for smoldering and active multiple myeloma. The researchers included patients enrolled in the database during 2003-2011; records were examined from the time to initial treatment and they considered reasons for patients not receiving treatment.
Patients who did not require treatment within the first 120 days after diagnosis were considered to have smoldering disease. This group comprised almost 14% of the cases.
The proportion of cases that were smoldering disease did not change significantly during the study period (P = .23 and .34, respectively). Smoldering disease was more likely to be diagnosed among women, black patients, older patients (median age at diagnosis was 67 years), and less educated patients. Smoldering disease was more common in patients with fewer medical comorbidities, those living closer to a treatment facility, and those evaluated for their disease in the Northeast United States. The proportions of cases diagnosed at academic and nonacademic facilities were similar.
The median overall survival for smoldering disease was 63 months; for active disease, 33 months. Overall survival in those with smoldering disease did not differ among the racial groups (P = .27).
The researchers had no financial conflicts.
On Twitter @maryjodales
FROM ASCO 2016
Key clinical point: The prevalence of smoldering multiple myeloma varied among various socio- and geodemographic subgroups, but overall survival did not.
Major finding: About 1 in 7 cases of multiple myeloma diagnosed in the United States are cases of smoldering disease.
Data source: At total of 86,327 cases of multiple myeloma from the National Cancer Data Base, which represents 70% of cancer cases.
Disclosures: The researchers had no financial conflicts.