User login
Pulsatile tinnitus looms large in fibromuscular dysplasia
WASHINGTON – Think cerebrovascular fibromuscular dysplasia in a middle-aged woman who presents with a complaint of pulsatile tinnitus.
That’s the take-home message from a new analysis of the United States Registry for Fibromuscular Dysplasia. The data highlight pulsatile tinnitus as an important clinical manifestation of fibromuscular dysplasia (FMD). Indeed, it was a presenting symptom in one-third of 720 patients included in the national registry, Dr. Redah Z. Mahmood reported at the annual meeting of the American College of Cardiology.
FMD is a nonatherosclerotic, noninflammatory form of vascular disease. It is predominantly a disease of middle-aged women: 91% of patients in the registry were women, as were 98% of patients who presented with pulsatile tinnitus. The mean age at symptom onset for registry participants was 48.8 years, although on average another 4.2 years passed before FMD was diagnosed on the basis of angiography or noninvasive imaging, noted Dr. Mahmood of the Cleveland Clinic.
FMD presents a formidable diagnostic challenge because of its potential to appear in virtually any arterial vascular bed and its lack of specific symptoms. The FMD registry was formed in 2008 in an effort to shed new light on the disorder. The association with pulsatile tinnitus is particularly helpful in raising the index of suspicion, he continued.
Patients with pulsatile tinnitus as a presenting symptom of FMD were more likely than those without that complaint to have frequent headaches, by a margin of 71%-47%. Nearly half of FMD patients with pulsatile tinnitus reported neck pain, compared with 19% without pulsatile tinnitus. Dizziness, transient ischemic attacks, cervical bruit, and Horner syndrome also were significantly more common in the pulsatile tinnitus group. This cluster of symptoms reflects the pulsatile tinnitus group’s increased prevalence of FMD of the medial fibroplasia type involving the extracranial carotid and vertebral artery beds. Patients with pulsatile tinnitus were not more likely, however, to present with stroke, which was a presenting symptom in only about 8% of patients.
Patients with pulsatile tinnitus had a reduced likelihood of renal and mesenteric involvement. Fifty-three percent of them had hypertension, compared with 67% of FMD patients without pulsatile tinnitus.
Thirty-two percent of FMD patients with pulsatile tinnitus had a history of an anxiety disorder, a rate twice that of patients without pulsatile tinnitus. Intriguingly, 84% of patients with pulsatile tinnitus had a history of use of oral contraceptives or hormone replacement therapy, compared with 56% of those without pulsatile tinnitus.
This study was sponsored by the Fibromuscular Dysplasia Study of America, a nonprofit organization. Dr. Mahmood reported having no financial conflicts.
WASHINGTON – Think cerebrovascular fibromuscular dysplasia in a middle-aged woman who presents with a complaint of pulsatile tinnitus.
That’s the take-home message from a new analysis of the United States Registry for Fibromuscular Dysplasia. The data highlight pulsatile tinnitus as an important clinical manifestation of fibromuscular dysplasia (FMD). Indeed, it was a presenting symptom in one-third of 720 patients included in the national registry, Dr. Redah Z. Mahmood reported at the annual meeting of the American College of Cardiology.
FMD is a nonatherosclerotic, noninflammatory form of vascular disease. It is predominantly a disease of middle-aged women: 91% of patients in the registry were women, as were 98% of patients who presented with pulsatile tinnitus. The mean age at symptom onset for registry participants was 48.8 years, although on average another 4.2 years passed before FMD was diagnosed on the basis of angiography or noninvasive imaging, noted Dr. Mahmood of the Cleveland Clinic.
FMD presents a formidable diagnostic challenge because of its potential to appear in virtually any arterial vascular bed and its lack of specific symptoms. The FMD registry was formed in 2008 in an effort to shed new light on the disorder. The association with pulsatile tinnitus is particularly helpful in raising the index of suspicion, he continued.
Patients with pulsatile tinnitus as a presenting symptom of FMD were more likely than those without that complaint to have frequent headaches, by a margin of 71%-47%. Nearly half of FMD patients with pulsatile tinnitus reported neck pain, compared with 19% without pulsatile tinnitus. Dizziness, transient ischemic attacks, cervical bruit, and Horner syndrome also were significantly more common in the pulsatile tinnitus group. This cluster of symptoms reflects the pulsatile tinnitus group’s increased prevalence of FMD of the medial fibroplasia type involving the extracranial carotid and vertebral artery beds. Patients with pulsatile tinnitus were not more likely, however, to present with stroke, which was a presenting symptom in only about 8% of patients.
Patients with pulsatile tinnitus had a reduced likelihood of renal and mesenteric involvement. Fifty-three percent of them had hypertension, compared with 67% of FMD patients without pulsatile tinnitus.
Thirty-two percent of FMD patients with pulsatile tinnitus had a history of an anxiety disorder, a rate twice that of patients without pulsatile tinnitus. Intriguingly, 84% of patients with pulsatile tinnitus had a history of use of oral contraceptives or hormone replacement therapy, compared with 56% of those without pulsatile tinnitus.
This study was sponsored by the Fibromuscular Dysplasia Study of America, a nonprofit organization. Dr. Mahmood reported having no financial conflicts.
WASHINGTON – Think cerebrovascular fibromuscular dysplasia in a middle-aged woman who presents with a complaint of pulsatile tinnitus.
That’s the take-home message from a new analysis of the United States Registry for Fibromuscular Dysplasia. The data highlight pulsatile tinnitus as an important clinical manifestation of fibromuscular dysplasia (FMD). Indeed, it was a presenting symptom in one-third of 720 patients included in the national registry, Dr. Redah Z. Mahmood reported at the annual meeting of the American College of Cardiology.
FMD is a nonatherosclerotic, noninflammatory form of vascular disease. It is predominantly a disease of middle-aged women: 91% of patients in the registry were women, as were 98% of patients who presented with pulsatile tinnitus. The mean age at symptom onset for registry participants was 48.8 years, although on average another 4.2 years passed before FMD was diagnosed on the basis of angiography or noninvasive imaging, noted Dr. Mahmood of the Cleveland Clinic.
FMD presents a formidable diagnostic challenge because of its potential to appear in virtually any arterial vascular bed and its lack of specific symptoms. The FMD registry was formed in 2008 in an effort to shed new light on the disorder. The association with pulsatile tinnitus is particularly helpful in raising the index of suspicion, he continued.
Patients with pulsatile tinnitus as a presenting symptom of FMD were more likely than those without that complaint to have frequent headaches, by a margin of 71%-47%. Nearly half of FMD patients with pulsatile tinnitus reported neck pain, compared with 19% without pulsatile tinnitus. Dizziness, transient ischemic attacks, cervical bruit, and Horner syndrome also were significantly more common in the pulsatile tinnitus group. This cluster of symptoms reflects the pulsatile tinnitus group’s increased prevalence of FMD of the medial fibroplasia type involving the extracranial carotid and vertebral artery beds. Patients with pulsatile tinnitus were not more likely, however, to present with stroke, which was a presenting symptom in only about 8% of patients.
Patients with pulsatile tinnitus had a reduced likelihood of renal and mesenteric involvement. Fifty-three percent of them had hypertension, compared with 67% of FMD patients without pulsatile tinnitus.
Thirty-two percent of FMD patients with pulsatile tinnitus had a history of an anxiety disorder, a rate twice that of patients without pulsatile tinnitus. Intriguingly, 84% of patients with pulsatile tinnitus had a history of use of oral contraceptives or hormone replacement therapy, compared with 56% of those without pulsatile tinnitus.
This study was sponsored by the Fibromuscular Dysplasia Study of America, a nonprofit organization. Dr. Mahmood reported having no financial conflicts.
AT ACC 14
Major finding: Pulsatile tinnitus was a presenting symptom in one-third of a large group of patients with fibromuscular dysplasia.
Data source: This was a study of 720 patients with confirmed fibromuscular dysplasia at 11 centers participating in the United States Registry for Fibromuscular Dysplasia.
Disclosures: The study was sponsored by the Fibromuscular Dysplasia Study of America. The presenter reported having no financial conflicts.
Even mild preop sepsis boosts postop thrombosis risk
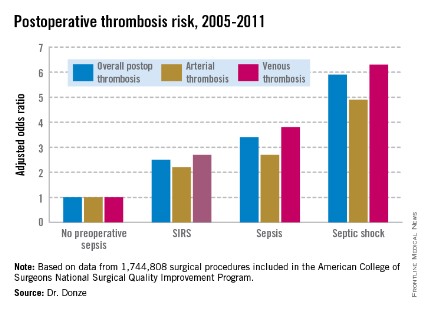
WASHINGTON – Preoperative sepsis proved to be an important independent risk factor for both arterial and venous thrombosis during or after surgery in an analysis of nearly 1.75 million U.S. surgical procedures.
The take-home message here is that the risk-benefit assessment of surgical procedures should take into account the presence of sepsis. And if the surgery can’t be delayed, prophylaxis against arterial as well as venous thrombosis should be employed, Dr. Jacques Donze said at the annual meeting of the American College of Cardiology.

Another key finding in this study was that the risk of postoperative thrombosis varied according to the severity of preoperative sepsis. Even the early form of sepsis known as systemic inflammatory response syndrome, or SIRS, was associated with a 2.5-fold increased risk.
"Include even early signs of sepsis as a risk factor," urged Dr. Donze of Brigham and Women’s Hospital, Boston.
Also, preoperative sepsis was a risk factor for postoperative thrombosis in connection with outpatient elective surgery as well as inpatient operations, he added.
Dr. Donze presented an analysis of 1,744,808 surgical procedures performed during 2005-2011 at 314 U.S. hospitals participating in the American College of Surgeons National Surgical Quality Improvement Program. This large, prospective, observational registry is known for its high-quality data.
Within 48 hours prior to surgery, 7.8% of patients – totaling more than 136,000 – had SIRS, sepsis, or septic shock. Their postoperative thrombosis rate was 4.2%, compared with a 1.2% rate in patients without sepsis. In a multivariate regression analysis adjusted for potential confounding factors, the postoperative thrombosis risk climbed with increasing severity of preoperative sepsis.
SIRS was defined on the basis of temperature, heart rate, respiratory rate, WBC count, and/or the presence of anion gap acidosis. "Sepsis" was defined as SIRS plus infection. And septic shock required the presence of sepsis plus documented organ dysfunction, such as hypotension.
The importance of recognizing this newly spotlighted sepsis/postoperative thrombosis connection is that most of the other known risk factors for thrombosis in surgical patients, including age, cancer, renal failure, and immobilization, are nonmodifiable, Dr. Donze observed.
Among the factors known to contribute to thrombosis are a hypercoagulable state, a proinflammatory state, hypoxemia, hypotension, and endothelial dysfunction. "All of these factors can be triggered by sepsis," Dr. Donze noted.
He reported having no financial conflicts regarding this study.
WASHINGTON – Preoperative sepsis proved to be an important independent risk factor for both arterial and venous thrombosis during or after surgery in an analysis of nearly 1.75 million U.S. surgical procedures.
The take-home message here is that the risk-benefit assessment of surgical procedures should take into account the presence of sepsis. And if the surgery can’t be delayed, prophylaxis against arterial as well as venous thrombosis should be employed, Dr. Jacques Donze said at the annual meeting of the American College of Cardiology.

Another key finding in this study was that the risk of postoperative thrombosis varied according to the severity of preoperative sepsis. Even the early form of sepsis known as systemic inflammatory response syndrome, or SIRS, was associated with a 2.5-fold increased risk.
"Include even early signs of sepsis as a risk factor," urged Dr. Donze of Brigham and Women’s Hospital, Boston.
Also, preoperative sepsis was a risk factor for postoperative thrombosis in connection with outpatient elective surgery as well as inpatient operations, he added.
Dr. Donze presented an analysis of 1,744,808 surgical procedures performed during 2005-2011 at 314 U.S. hospitals participating in the American College of Surgeons National Surgical Quality Improvement Program. This large, prospective, observational registry is known for its high-quality data.
Within 48 hours prior to surgery, 7.8% of patients – totaling more than 136,000 – had SIRS, sepsis, or septic shock. Their postoperative thrombosis rate was 4.2%, compared with a 1.2% rate in patients without sepsis. In a multivariate regression analysis adjusted for potential confounding factors, the postoperative thrombosis risk climbed with increasing severity of preoperative sepsis.
SIRS was defined on the basis of temperature, heart rate, respiratory rate, WBC count, and/or the presence of anion gap acidosis. "Sepsis" was defined as SIRS plus infection. And septic shock required the presence of sepsis plus documented organ dysfunction, such as hypotension.
The importance of recognizing this newly spotlighted sepsis/postoperative thrombosis connection is that most of the other known risk factors for thrombosis in surgical patients, including age, cancer, renal failure, and immobilization, are nonmodifiable, Dr. Donze observed.
Among the factors known to contribute to thrombosis are a hypercoagulable state, a proinflammatory state, hypoxemia, hypotension, and endothelial dysfunction. "All of these factors can be triggered by sepsis," Dr. Donze noted.
He reported having no financial conflicts regarding this study.
WASHINGTON – Preoperative sepsis proved to be an important independent risk factor for both arterial and venous thrombosis during or after surgery in an analysis of nearly 1.75 million U.S. surgical procedures.
The take-home message here is that the risk-benefit assessment of surgical procedures should take into account the presence of sepsis. And if the surgery can’t be delayed, prophylaxis against arterial as well as venous thrombosis should be employed, Dr. Jacques Donze said at the annual meeting of the American College of Cardiology.

Another key finding in this study was that the risk of postoperative thrombosis varied according to the severity of preoperative sepsis. Even the early form of sepsis known as systemic inflammatory response syndrome, or SIRS, was associated with a 2.5-fold increased risk.
"Include even early signs of sepsis as a risk factor," urged Dr. Donze of Brigham and Women’s Hospital, Boston.
Also, preoperative sepsis was a risk factor for postoperative thrombosis in connection with outpatient elective surgery as well as inpatient operations, he added.
Dr. Donze presented an analysis of 1,744,808 surgical procedures performed during 2005-2011 at 314 U.S. hospitals participating in the American College of Surgeons National Surgical Quality Improvement Program. This large, prospective, observational registry is known for its high-quality data.
Within 48 hours prior to surgery, 7.8% of patients – totaling more than 136,000 – had SIRS, sepsis, or septic shock. Their postoperative thrombosis rate was 4.2%, compared with a 1.2% rate in patients without sepsis. In a multivariate regression analysis adjusted for potential confounding factors, the postoperative thrombosis risk climbed with increasing severity of preoperative sepsis.
SIRS was defined on the basis of temperature, heart rate, respiratory rate, WBC count, and/or the presence of anion gap acidosis. "Sepsis" was defined as SIRS plus infection. And septic shock required the presence of sepsis plus documented organ dysfunction, such as hypotension.
The importance of recognizing this newly spotlighted sepsis/postoperative thrombosis connection is that most of the other known risk factors for thrombosis in surgical patients, including age, cancer, renal failure, and immobilization, are nonmodifiable, Dr. Donze observed.
Among the factors known to contribute to thrombosis are a hypercoagulable state, a proinflammatory state, hypoxemia, hypotension, and endothelial dysfunction. "All of these factors can be triggered by sepsis," Dr. Donze noted.
He reported having no financial conflicts regarding this study.
AT ACC 14
Major finding: Preoperative sepsis is a strong independent risk factor for postoperative arterial and venous thrombosis; the more severe the sepsis, the greater the thrombosis risk.
Data source: This was an analysis of nearly 1.75 million surgical procedures at 314 U.S. hospitals detailed in the American College of Surgeons National Quality Improvement Program registry.
Disclosures: The presenter reported having no financial conflicts.
ECG screening of young athletes doesn’t trigger anxiety
WASHINGTON – Preparticipation 12-lead ECG screening of school age athletes didn’t cause an increase in anxiety levels, regardless of race, sex, or age, in a large study.
Skeptics of ECG screening of young athletes to identify those with occult hypertrophic cardiomyopathy and other conditions of interest have raised the specter that false-positive results in mass screening programs would cause waves of needless anxiety. But this assertion has not been formally evaluated until now, Dr. Mallory Irwin said at the annual meeting of the American College of Cardiology.
Dr. Irwin of the department of family medicine at the University of Tennessee, Knoxville, presented a prospective multisite study involving 1,504 athletes in 18 sports at 22 high schools, all of whom underwent precompetition cardiovascular screening by history, physical exam, and 12-lead ECG. Those with a positive screen got an on-site echocardiographic examination. As part of the study, all athletes also received pre- and postscreen validated psychological assessments focusing on anxiety, health attitudes, and the impact of screening on sports participation.
Of the athletes, 76% had a normal screen, 23% had what proved to be a false-positive screen, and just under 1% were diagnosed with a major or minor cardiac disorder.
Overall, athletes didn’t report feeling anxiety during the screening. There was no difference in anxiety level between those with a normal screen, compared with athletes with a false-positive screen. Anxiety levels in athletes with a false-positive screen were similar, regardless of whether the false-positive finding was based upon the ECG, physical exam, or history. Those with a false-positive screen said afterward that they would still recommend routine preparticipation ECG screening, and that the more intensive work-up they got based upon the screening result would have a positive impact on their training because of the extra measure of reassurance it provided.
"Undue anxiety due to false-positive screens does not appear to be a justified reason to oppose ECG screening," Dr. Irwin said.
The 0.9% of athletes who were diagnosed with a cardiac condition did have higher anxiety levels after receiving their diagnosis, but they also expressed a conviction that all athletes should have an ECG prior to sports competition, she added.
Before undergoing screening, the female athletes expressed a significantly greater preference for knowing about any underlying cardiac condition, compared with their male counterparts. The black athletes were as a group less concerned about and less interested in cardiovascular screening than were the white athletes.
The standardized history and physical exam used in the study were based on American Heart Association guidelines. The 12-lead ECG interpretation relied upon the 2013 Seattle criteria.
This study was funded in part by an American Medical Society for Sports Medicine Young Investigator Research Grant to Dr. Irwin, who reported having no financial conflicts.
WASHINGTON – Preparticipation 12-lead ECG screening of school age athletes didn’t cause an increase in anxiety levels, regardless of race, sex, or age, in a large study.
Skeptics of ECG screening of young athletes to identify those with occult hypertrophic cardiomyopathy and other conditions of interest have raised the specter that false-positive results in mass screening programs would cause waves of needless anxiety. But this assertion has not been formally evaluated until now, Dr. Mallory Irwin said at the annual meeting of the American College of Cardiology.
Dr. Irwin of the department of family medicine at the University of Tennessee, Knoxville, presented a prospective multisite study involving 1,504 athletes in 18 sports at 22 high schools, all of whom underwent precompetition cardiovascular screening by history, physical exam, and 12-lead ECG. Those with a positive screen got an on-site echocardiographic examination. As part of the study, all athletes also received pre- and postscreen validated psychological assessments focusing on anxiety, health attitudes, and the impact of screening on sports participation.
Of the athletes, 76% had a normal screen, 23% had what proved to be a false-positive screen, and just under 1% were diagnosed with a major or minor cardiac disorder.
Overall, athletes didn’t report feeling anxiety during the screening. There was no difference in anxiety level between those with a normal screen, compared with athletes with a false-positive screen. Anxiety levels in athletes with a false-positive screen were similar, regardless of whether the false-positive finding was based upon the ECG, physical exam, or history. Those with a false-positive screen said afterward that they would still recommend routine preparticipation ECG screening, and that the more intensive work-up they got based upon the screening result would have a positive impact on their training because of the extra measure of reassurance it provided.
"Undue anxiety due to false-positive screens does not appear to be a justified reason to oppose ECG screening," Dr. Irwin said.
The 0.9% of athletes who were diagnosed with a cardiac condition did have higher anxiety levels after receiving their diagnosis, but they also expressed a conviction that all athletes should have an ECG prior to sports competition, she added.
Before undergoing screening, the female athletes expressed a significantly greater preference for knowing about any underlying cardiac condition, compared with their male counterparts. The black athletes were as a group less concerned about and less interested in cardiovascular screening than were the white athletes.
The standardized history and physical exam used in the study were based on American Heart Association guidelines. The 12-lead ECG interpretation relied upon the 2013 Seattle criteria.
This study was funded in part by an American Medical Society for Sports Medicine Young Investigator Research Grant to Dr. Irwin, who reported having no financial conflicts.
WASHINGTON – Preparticipation 12-lead ECG screening of school age athletes didn’t cause an increase in anxiety levels, regardless of race, sex, or age, in a large study.
Skeptics of ECG screening of young athletes to identify those with occult hypertrophic cardiomyopathy and other conditions of interest have raised the specter that false-positive results in mass screening programs would cause waves of needless anxiety. But this assertion has not been formally evaluated until now, Dr. Mallory Irwin said at the annual meeting of the American College of Cardiology.
Dr. Irwin of the department of family medicine at the University of Tennessee, Knoxville, presented a prospective multisite study involving 1,504 athletes in 18 sports at 22 high schools, all of whom underwent precompetition cardiovascular screening by history, physical exam, and 12-lead ECG. Those with a positive screen got an on-site echocardiographic examination. As part of the study, all athletes also received pre- and postscreen validated psychological assessments focusing on anxiety, health attitudes, and the impact of screening on sports participation.
Of the athletes, 76% had a normal screen, 23% had what proved to be a false-positive screen, and just under 1% were diagnosed with a major or minor cardiac disorder.
Overall, athletes didn’t report feeling anxiety during the screening. There was no difference in anxiety level between those with a normal screen, compared with athletes with a false-positive screen. Anxiety levels in athletes with a false-positive screen were similar, regardless of whether the false-positive finding was based upon the ECG, physical exam, or history. Those with a false-positive screen said afterward that they would still recommend routine preparticipation ECG screening, and that the more intensive work-up they got based upon the screening result would have a positive impact on their training because of the extra measure of reassurance it provided.
"Undue anxiety due to false-positive screens does not appear to be a justified reason to oppose ECG screening," Dr. Irwin said.
The 0.9% of athletes who were diagnosed with a cardiac condition did have higher anxiety levels after receiving their diagnosis, but they also expressed a conviction that all athletes should have an ECG prior to sports competition, she added.
Before undergoing screening, the female athletes expressed a significantly greater preference for knowing about any underlying cardiac condition, compared with their male counterparts. The black athletes were as a group less concerned about and less interested in cardiovascular screening than were the white athletes.
The standardized history and physical exam used in the study were based on American Heart Association guidelines. The 12-lead ECG interpretation relied upon the 2013 Seattle criteria.
This study was funded in part by an American Medical Society for Sports Medicine Young Investigator Research Grant to Dr. Irwin, who reported having no financial conflicts.
AT ACC 14
Major finding: Precompetition cardiac screening of high school athletes via 12-lead ECG, history, and physical exam did not result in excessive anxiety, even in the 23% with what proved to be a false-positive result.
Data source: A prospective study of 1,504 athletes participating in 18 sports at 22 high schools who underwent standardized preparticipation cardiovascular screening as well as validated pre- and postscreen psychological assessments.
Disclosures: The study was partially funded by an American Medical Society for Sports Medicine Young Investigator Research Grant to the presenter, who reported no financial conflicts.
Apixiban for VTE reduces subsequent hospitalizations
WASHINGTON – Treating acute venous thromboembolism with the fixed-dose oral factor Xa inhibitor apixaban significantly reduces subsequent all-cause hospitalizations, compared with conventional therapy with enoxaparin followed by warfarin, according to a secondary analysis of the landmark AMPLIFY trial.
The 21% reduction in the risk of hospitalization in the apixaban group during the 6 months following the initial VTE was driven mainly by fewer hospitalizations for recurrent VTE or major bleeding. There were also significantly fewer physician office visits by patients on apixaban than for those on enoxaparin/warfarin, Dr. Margot Johnson reported at the annual meeting of the American College of Cardiology.
An analysis of the cost savings associated with this reduction in hospitalizations seen in AMPLIFY is underway and will be reported later this year, added Dr. Johnson of King’s College Hospital in London.
AMPLIFY (Apixaban for the Initial Management of Pulmonary Embolism and Deep Vein Thrombosis) was a randomized double-blind study of 5,365 patients with acute symptomatic VTE who were assigned to 6 months of treatment with apixaban (Eliquis) at 10 mg b.i.d. for 7 days followed by 5 mg b.i.d. or to enoxaparin followed by warfarin. In the previously reported primary outcomes (N. Engl. J. Med. 2013;369:799-808), apixaban showed noninferiority to the conventional regimen in terms of the rate of recurrent VTE or VTE-related death, and a highly significant superiority in terms of major bleeding, with a 69% risk reduction.
Dr. Johnson reported that during the 6-month study period, 5.72% of the apixaban group had one or more hospitalizations after the initial event, compared with 7.07% of the control group. This translated to a significant 21% relative risk reduction. For every 74 patients treated with apixaban instead of enoxaparin/warfarin, one hospitalization was avoided. Moreover, when a hospitalization occurred in apixaban-treated patients, the mean length of stay was shorter: 10.2 vs. 11.7 days in the enoxaparin-warfarin group.
The median time to a first hospitalization was 63 days in the apixaban group, compared with 34.5 days in controls.
The apixaban group’s advantage in terms of hospitalization risk was consistent across subgroups on the basis of age, body weight, sex, and renal function.
The number of emergency department visits during the 6-month follow-up period was similar in the two study arms. However, only 5.8% of the apixaban group visited a physician’s office, compared with 7.3% of controls. The reasons for these office visits were basically the same as for the hospitalizations: mostly recurrent VTEs and bleeding episodes. In the apixaban group, 35 patients had an office visit for recurrent VTE, compared with 61 controls. And 71 apixaban-treated patients made an office visit for bleeding episodes, compared with 130 controls.
Session cochair Dr. Emile R. Mohler commented on the finding that 37 patients in the apixaban group and 48 on enoxaparin/warfarin required hospitalization for recurrent VTE.
"It seems like we’re not doing a good enough job there. Either both of these anticoagulants don’t work well, or the patients aren’t taking the medication, or we’re not following up with them enough. I can’t remember the last time in my own clinical practice that somebody who took their medication came back within 6 months of having a VTE. It seems strange. I think there’s a lot of room for improvement," commented Dr. Mohler, professor of medicine and director of vascular medicine at the University of Pennsylvania, Philadelphia.
Dr. Johnson agreed about the room for improvement. But she added that, although the data she presented were based upon an intention-to-treat analysis, the results were the same – significantly fewer hospitalizations in the apixaban group – in a per-protocol analysis that excluded patients with less than 80% adherence to their study medication.
"One of the big things we saw in AMPLIFY is that whenever you stop an anticoagulant, you see the recurrence rate go up by about 10% per year. So it’s very important that these people continue their anticoagulation – and the more we can reduce their bleeding events, the more likely they are to comply with that therapy and be protected from having another VTE," she added.
Session cochair Dr. John P. Cooke commented that one underutilized aspect of treatment for acute VTE is compressive support, which he said has been given short shrift in the major practice guidelines.
"Often as physicians, we give patients a pill and we think that we’ve treated them. Compressive support is important in VTE," stressed Dr. Cooke, chair of the department of cardiovascular sciences at the Houston Methodist Research Institute and director of the Center for Cardiovascular Regeneration at the Houston Methodist DeBakey Heart and Vascular Center.
The AMPLIFY trial was sponsored by Bristol-Myers Squibb and Pfizer. Dr. Johnson reported having no financial conflicts.
WASHINGTON – Treating acute venous thromboembolism with the fixed-dose oral factor Xa inhibitor apixaban significantly reduces subsequent all-cause hospitalizations, compared with conventional therapy with enoxaparin followed by warfarin, according to a secondary analysis of the landmark AMPLIFY trial.
The 21% reduction in the risk of hospitalization in the apixaban group during the 6 months following the initial VTE was driven mainly by fewer hospitalizations for recurrent VTE or major bleeding. There were also significantly fewer physician office visits by patients on apixaban than for those on enoxaparin/warfarin, Dr. Margot Johnson reported at the annual meeting of the American College of Cardiology.
An analysis of the cost savings associated with this reduction in hospitalizations seen in AMPLIFY is underway and will be reported later this year, added Dr. Johnson of King’s College Hospital in London.
AMPLIFY (Apixaban for the Initial Management of Pulmonary Embolism and Deep Vein Thrombosis) was a randomized double-blind study of 5,365 patients with acute symptomatic VTE who were assigned to 6 months of treatment with apixaban (Eliquis) at 10 mg b.i.d. for 7 days followed by 5 mg b.i.d. or to enoxaparin followed by warfarin. In the previously reported primary outcomes (N. Engl. J. Med. 2013;369:799-808), apixaban showed noninferiority to the conventional regimen in terms of the rate of recurrent VTE or VTE-related death, and a highly significant superiority in terms of major bleeding, with a 69% risk reduction.
Dr. Johnson reported that during the 6-month study period, 5.72% of the apixaban group had one or more hospitalizations after the initial event, compared with 7.07% of the control group. This translated to a significant 21% relative risk reduction. For every 74 patients treated with apixaban instead of enoxaparin/warfarin, one hospitalization was avoided. Moreover, when a hospitalization occurred in apixaban-treated patients, the mean length of stay was shorter: 10.2 vs. 11.7 days in the enoxaparin-warfarin group.
The median time to a first hospitalization was 63 days in the apixaban group, compared with 34.5 days in controls.
The apixaban group’s advantage in terms of hospitalization risk was consistent across subgroups on the basis of age, body weight, sex, and renal function.
The number of emergency department visits during the 6-month follow-up period was similar in the two study arms. However, only 5.8% of the apixaban group visited a physician’s office, compared with 7.3% of controls. The reasons for these office visits were basically the same as for the hospitalizations: mostly recurrent VTEs and bleeding episodes. In the apixaban group, 35 patients had an office visit for recurrent VTE, compared with 61 controls. And 71 apixaban-treated patients made an office visit for bleeding episodes, compared with 130 controls.
Session cochair Dr. Emile R. Mohler commented on the finding that 37 patients in the apixaban group and 48 on enoxaparin/warfarin required hospitalization for recurrent VTE.
"It seems like we’re not doing a good enough job there. Either both of these anticoagulants don’t work well, or the patients aren’t taking the medication, or we’re not following up with them enough. I can’t remember the last time in my own clinical practice that somebody who took their medication came back within 6 months of having a VTE. It seems strange. I think there’s a lot of room for improvement," commented Dr. Mohler, professor of medicine and director of vascular medicine at the University of Pennsylvania, Philadelphia.
Dr. Johnson agreed about the room for improvement. But she added that, although the data she presented were based upon an intention-to-treat analysis, the results were the same – significantly fewer hospitalizations in the apixaban group – in a per-protocol analysis that excluded patients with less than 80% adherence to their study medication.
"One of the big things we saw in AMPLIFY is that whenever you stop an anticoagulant, you see the recurrence rate go up by about 10% per year. So it’s very important that these people continue their anticoagulation – and the more we can reduce their bleeding events, the more likely they are to comply with that therapy and be protected from having another VTE," she added.
Session cochair Dr. John P. Cooke commented that one underutilized aspect of treatment for acute VTE is compressive support, which he said has been given short shrift in the major practice guidelines.
"Often as physicians, we give patients a pill and we think that we’ve treated them. Compressive support is important in VTE," stressed Dr. Cooke, chair of the department of cardiovascular sciences at the Houston Methodist Research Institute and director of the Center for Cardiovascular Regeneration at the Houston Methodist DeBakey Heart and Vascular Center.
The AMPLIFY trial was sponsored by Bristol-Myers Squibb and Pfizer. Dr. Johnson reported having no financial conflicts.
WASHINGTON – Treating acute venous thromboembolism with the fixed-dose oral factor Xa inhibitor apixaban significantly reduces subsequent all-cause hospitalizations, compared with conventional therapy with enoxaparin followed by warfarin, according to a secondary analysis of the landmark AMPLIFY trial.
The 21% reduction in the risk of hospitalization in the apixaban group during the 6 months following the initial VTE was driven mainly by fewer hospitalizations for recurrent VTE or major bleeding. There were also significantly fewer physician office visits by patients on apixaban than for those on enoxaparin/warfarin, Dr. Margot Johnson reported at the annual meeting of the American College of Cardiology.
An analysis of the cost savings associated with this reduction in hospitalizations seen in AMPLIFY is underway and will be reported later this year, added Dr. Johnson of King’s College Hospital in London.
AMPLIFY (Apixaban for the Initial Management of Pulmonary Embolism and Deep Vein Thrombosis) was a randomized double-blind study of 5,365 patients with acute symptomatic VTE who were assigned to 6 months of treatment with apixaban (Eliquis) at 10 mg b.i.d. for 7 days followed by 5 mg b.i.d. or to enoxaparin followed by warfarin. In the previously reported primary outcomes (N. Engl. J. Med. 2013;369:799-808), apixaban showed noninferiority to the conventional regimen in terms of the rate of recurrent VTE or VTE-related death, and a highly significant superiority in terms of major bleeding, with a 69% risk reduction.
Dr. Johnson reported that during the 6-month study period, 5.72% of the apixaban group had one or more hospitalizations after the initial event, compared with 7.07% of the control group. This translated to a significant 21% relative risk reduction. For every 74 patients treated with apixaban instead of enoxaparin/warfarin, one hospitalization was avoided. Moreover, when a hospitalization occurred in apixaban-treated patients, the mean length of stay was shorter: 10.2 vs. 11.7 days in the enoxaparin-warfarin group.
The median time to a first hospitalization was 63 days in the apixaban group, compared with 34.5 days in controls.
The apixaban group’s advantage in terms of hospitalization risk was consistent across subgroups on the basis of age, body weight, sex, and renal function.
The number of emergency department visits during the 6-month follow-up period was similar in the two study arms. However, only 5.8% of the apixaban group visited a physician’s office, compared with 7.3% of controls. The reasons for these office visits were basically the same as for the hospitalizations: mostly recurrent VTEs and bleeding episodes. In the apixaban group, 35 patients had an office visit for recurrent VTE, compared with 61 controls. And 71 apixaban-treated patients made an office visit for bleeding episodes, compared with 130 controls.
Session cochair Dr. Emile R. Mohler commented on the finding that 37 patients in the apixaban group and 48 on enoxaparin/warfarin required hospitalization for recurrent VTE.
"It seems like we’re not doing a good enough job there. Either both of these anticoagulants don’t work well, or the patients aren’t taking the medication, or we’re not following up with them enough. I can’t remember the last time in my own clinical practice that somebody who took their medication came back within 6 months of having a VTE. It seems strange. I think there’s a lot of room for improvement," commented Dr. Mohler, professor of medicine and director of vascular medicine at the University of Pennsylvania, Philadelphia.
Dr. Johnson agreed about the room for improvement. But she added that, although the data she presented were based upon an intention-to-treat analysis, the results were the same – significantly fewer hospitalizations in the apixaban group – in a per-protocol analysis that excluded patients with less than 80% adherence to their study medication.
"One of the big things we saw in AMPLIFY is that whenever you stop an anticoagulant, you see the recurrence rate go up by about 10% per year. So it’s very important that these people continue their anticoagulation – and the more we can reduce their bleeding events, the more likely they are to comply with that therapy and be protected from having another VTE," she added.
Session cochair Dr. John P. Cooke commented that one underutilized aspect of treatment for acute VTE is compressive support, which he said has been given short shrift in the major practice guidelines.
"Often as physicians, we give patients a pill and we think that we’ve treated them. Compressive support is important in VTE," stressed Dr. Cooke, chair of the department of cardiovascular sciences at the Houston Methodist Research Institute and director of the Center for Cardiovascular Regeneration at the Houston Methodist DeBakey Heart and Vascular Center.
The AMPLIFY trial was sponsored by Bristol-Myers Squibb and Pfizer. Dr. Johnson reported having no financial conflicts.
AT ACC 14
Major finding: Patients whose acute venous thromboembolism was treated with 6 months of apixaban were 21% less likely to have another hospitalization than were those who received enoxaparin followed by warfarin.
Data source: The double-blind AMPLIFY trial, which randomized 5,365 patients with acute VTE to 6 months of fixed-dose apixaban or conventional therapy with enoxaparin followed by warfarin.
Disclosures: The study was sponsored by Bristol-Myers Squibb and Pfizer. The presenter reported having no financial conflicts.
Marriage protects against vascular disease
WASHINGTON – Being married is independently associated with a significantly reduced rate of vascular disease across all arterial beds, according to a population-based study of more than 3.5 million subjects.
This apparent protective effect was strongest in younger individuals. In a multivariate regression analysis adjusted for demographics and cardiovascular risk factors, married subjects under age 50 years were 12% less likely to have prevalent vascular disease than were those who were single. The risk advantage shrank with advancing age such that married participants above age 70 years had a 4% lower risk of vascular disease than did those who were single, a difference that was statistically significant because of the huge size of the study population. And those who were single were at lower risk than were widowed or divorced subjects, Dr. Carlos L. Alviar reported at the annual meeting of the American College of Cardiology.
He presented an analysis of slightly more than 3.5 million participants in the Life Line Screening Diabetes Mellitus and Vascular Disease survey conducted during 2003-2008. Unlike most other studies of the relationship between marital status and health, which have focused on the risk of coronary disease, this study also included screening for peripheral artery disease, abdominal aortic aneurysm, and cerebrovascular disease.
Among participants of all ages, the risk of prevalent vascular disease was 5% less in those who were married than in those who were single. The risk was 3.2% greater in subjects who were divorced than in those who were single, and 5.1% greater in subjects who were widowed, according to Dr. Alviar of New York University.
The mean age of the study population was 63.7 years. Among women, 63.4% were married, 8.1% were single, 10.5% divorced, and 18% widowed. The male demographics were somewhat different: 80.4% of the men were married, 8.8% single, 6.1% divorced, and 4.7% were widowed.
Being widowed was associated with a higher prevalence of diabetes, hypertension, physical inactivity, and dyslipidemia, although investigators adjusted for that in their multivariate analysis. Divorced subjects were more likely to be smokers and have a family history of premature cardiovascular disease.
Dr. Alviar proposed as potential explanations for the reduced prevalence of vascular disease among married individuals their possibly lower levels of psychologic and physical stress, better access to medical care, and improved adherence to medication.
He reported having no financial disclosures regarding this study.
WASHINGTON – Being married is independently associated with a significantly reduced rate of vascular disease across all arterial beds, according to a population-based study of more than 3.5 million subjects.
This apparent protective effect was strongest in younger individuals. In a multivariate regression analysis adjusted for demographics and cardiovascular risk factors, married subjects under age 50 years were 12% less likely to have prevalent vascular disease than were those who were single. The risk advantage shrank with advancing age such that married participants above age 70 years had a 4% lower risk of vascular disease than did those who were single, a difference that was statistically significant because of the huge size of the study population. And those who were single were at lower risk than were widowed or divorced subjects, Dr. Carlos L. Alviar reported at the annual meeting of the American College of Cardiology.
He presented an analysis of slightly more than 3.5 million participants in the Life Line Screening Diabetes Mellitus and Vascular Disease survey conducted during 2003-2008. Unlike most other studies of the relationship between marital status and health, which have focused on the risk of coronary disease, this study also included screening for peripheral artery disease, abdominal aortic aneurysm, and cerebrovascular disease.
Among participants of all ages, the risk of prevalent vascular disease was 5% less in those who were married than in those who were single. The risk was 3.2% greater in subjects who were divorced than in those who were single, and 5.1% greater in subjects who were widowed, according to Dr. Alviar of New York University.
The mean age of the study population was 63.7 years. Among women, 63.4% were married, 8.1% were single, 10.5% divorced, and 18% widowed. The male demographics were somewhat different: 80.4% of the men were married, 8.8% single, 6.1% divorced, and 4.7% were widowed.
Being widowed was associated with a higher prevalence of diabetes, hypertension, physical inactivity, and dyslipidemia, although investigators adjusted for that in their multivariate analysis. Divorced subjects were more likely to be smokers and have a family history of premature cardiovascular disease.
Dr. Alviar proposed as potential explanations for the reduced prevalence of vascular disease among married individuals their possibly lower levels of psychologic and physical stress, better access to medical care, and improved adherence to medication.
He reported having no financial disclosures regarding this study.
WASHINGTON – Being married is independently associated with a significantly reduced rate of vascular disease across all arterial beds, according to a population-based study of more than 3.5 million subjects.
This apparent protective effect was strongest in younger individuals. In a multivariate regression analysis adjusted for demographics and cardiovascular risk factors, married subjects under age 50 years were 12% less likely to have prevalent vascular disease than were those who were single. The risk advantage shrank with advancing age such that married participants above age 70 years had a 4% lower risk of vascular disease than did those who were single, a difference that was statistically significant because of the huge size of the study population. And those who were single were at lower risk than were widowed or divorced subjects, Dr. Carlos L. Alviar reported at the annual meeting of the American College of Cardiology.
He presented an analysis of slightly more than 3.5 million participants in the Life Line Screening Diabetes Mellitus and Vascular Disease survey conducted during 2003-2008. Unlike most other studies of the relationship between marital status and health, which have focused on the risk of coronary disease, this study also included screening for peripheral artery disease, abdominal aortic aneurysm, and cerebrovascular disease.
Among participants of all ages, the risk of prevalent vascular disease was 5% less in those who were married than in those who were single. The risk was 3.2% greater in subjects who were divorced than in those who were single, and 5.1% greater in subjects who were widowed, according to Dr. Alviar of New York University.
The mean age of the study population was 63.7 years. Among women, 63.4% were married, 8.1% were single, 10.5% divorced, and 18% widowed. The male demographics were somewhat different: 80.4% of the men were married, 8.8% single, 6.1% divorced, and 4.7% were widowed.
Being widowed was associated with a higher prevalence of diabetes, hypertension, physical inactivity, and dyslipidemia, although investigators adjusted for that in their multivariate analysis. Divorced subjects were more likely to be smokers and have a family history of premature cardiovascular disease.
Dr. Alviar proposed as potential explanations for the reduced prevalence of vascular disease among married individuals their possibly lower levels of psychologic and physical stress, better access to medical care, and improved adherence to medication.
He reported having no financial disclosures regarding this study.
AT ACC 14
Major finding: Married men under age 50 years were 14.4% less likely than their single counterparts were to have vascular disease, and married women were 10.7% less likely. This advantage remained significant, albeit attenuated, in older married individuals.
Data source: This was an analysis of 3,532,189 adult participants in the Life Line Screening Diabetes Mellitus and Vascular Disease survey.
Disclosures: The study presenter reported having no financial conflicts of interest.
When Low HDL Means ‘No Sweat’
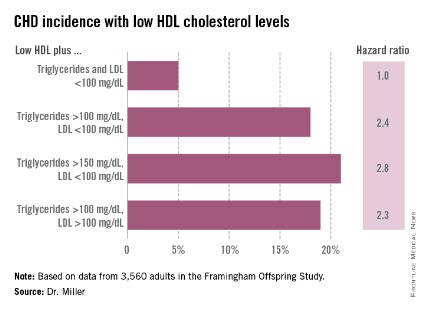
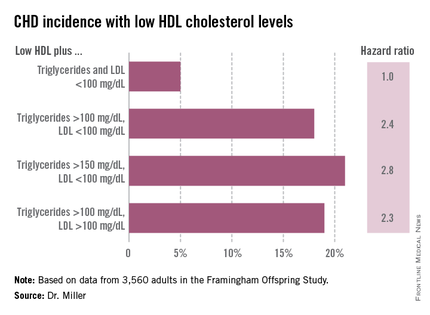
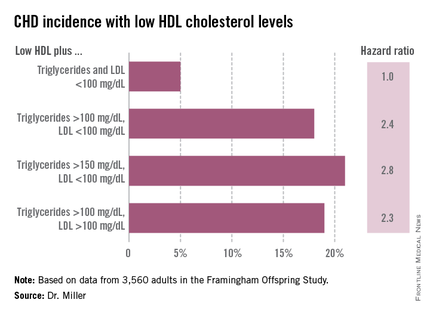
WASHINGTON– Low HDL cholesterol does not increase the risk of coronary heart disease when LDL cholesterol and triglyceride levels are normal, according to an analysis from the Framingham Offspring Study.
"In the Framingham Offspring Study, isolated HDL levels lower than the median are associated with a low risk of CHD. These data suggest that isolated low HDL may not be an atherogenic phenotype, Dr. Michael Miller said at the annual meeting of the American College of Cardiology.
While it’s well established that low HDL is associated with increased CHD risk, the risk in patients with isolated low HDL hasn’t been well studied. Yet low HDL together with an LDL below 100 mg/dL and a triglyceride level below 100 mg/dL is not a rare combination. It represented 7.4% of all study participants with low HDL, as defined by a level below the median, meaning less than 42 mg/dL in men and 54 mg/dL in women, noted Dr. Miller, professor of medicine, epidemiology, and preventive medicine and director of the center for preventive cardiology at the University of Maryland, Baltimore.
He reported on 3,560 adults in the Framingham Offspring Study with baseline lipid measurements recorded in 1987-1991. During a mean follow-up of 18 years, the incidence of newly diagnosed CHD was low in participants with isolated low HDL: just 5%. That was similar to the 4% incidence in subjects with above average HDL and low LDL and triglycerides. In contrast, when low HDL was present in subjects with higher LDL and/or triglycerides, the incidence of CHD was higher. So was the relative risk of CHD in a multivariate analysis after adjustment for age, sex, smoking status, diabetes, and hypertension.
When low HDL was present in combination with an LDL greater than 130 mg/dL along with triglycerides elevated above cut points of 150 and 200 mg/dL, the incident CHD rates climbed to 20%-25%, with adjusted hazard ratios of 1.7-2, compared with the risk in subjects with isolated low HDL.
The Framingham Offspring Study is funded by the National Heart, Lung, and Blood Institute. Dr. Miller reported receiving a research grant from Amgen.
WASHINGTON– Low HDL cholesterol does not increase the risk of coronary heart disease when LDL cholesterol and triglyceride levels are normal, according to an analysis from the Framingham Offspring Study.
"In the Framingham Offspring Study, isolated HDL levels lower than the median are associated with a low risk of CHD. These data suggest that isolated low HDL may not be an atherogenic phenotype, Dr. Michael Miller said at the annual meeting of the American College of Cardiology.
While it’s well established that low HDL is associated with increased CHD risk, the risk in patients with isolated low HDL hasn’t been well studied. Yet low HDL together with an LDL below 100 mg/dL and a triglyceride level below 100 mg/dL is not a rare combination. It represented 7.4% of all study participants with low HDL, as defined by a level below the median, meaning less than 42 mg/dL in men and 54 mg/dL in women, noted Dr. Miller, professor of medicine, epidemiology, and preventive medicine and director of the center for preventive cardiology at the University of Maryland, Baltimore.
He reported on 3,560 adults in the Framingham Offspring Study with baseline lipid measurements recorded in 1987-1991. During a mean follow-up of 18 years, the incidence of newly diagnosed CHD was low in participants with isolated low HDL: just 5%. That was similar to the 4% incidence in subjects with above average HDL and low LDL and triglycerides. In contrast, when low HDL was present in subjects with higher LDL and/or triglycerides, the incidence of CHD was higher. So was the relative risk of CHD in a multivariate analysis after adjustment for age, sex, smoking status, diabetes, and hypertension.
When low HDL was present in combination with an LDL greater than 130 mg/dL along with triglycerides elevated above cut points of 150 and 200 mg/dL, the incident CHD rates climbed to 20%-25%, with adjusted hazard ratios of 1.7-2, compared with the risk in subjects with isolated low HDL.
The Framingham Offspring Study is funded by the National Heart, Lung, and Blood Institute. Dr. Miller reported receiving a research grant from Amgen.
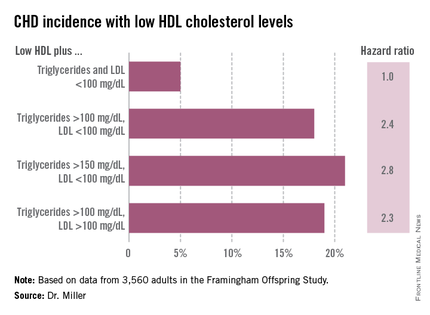
WASHINGTON– Low HDL cholesterol does not increase the risk of coronary heart disease when LDL cholesterol and triglyceride levels are normal, according to an analysis from the Framingham Offspring Study.
"In the Framingham Offspring Study, isolated HDL levels lower than the median are associated with a low risk of CHD. These data suggest that isolated low HDL may not be an atherogenic phenotype, Dr. Michael Miller said at the annual meeting of the American College of Cardiology.
While it’s well established that low HDL is associated with increased CHD risk, the risk in patients with isolated low HDL hasn’t been well studied. Yet low HDL together with an LDL below 100 mg/dL and a triglyceride level below 100 mg/dL is not a rare combination. It represented 7.4% of all study participants with low HDL, as defined by a level below the median, meaning less than 42 mg/dL in men and 54 mg/dL in women, noted Dr. Miller, professor of medicine, epidemiology, and preventive medicine and director of the center for preventive cardiology at the University of Maryland, Baltimore.
He reported on 3,560 adults in the Framingham Offspring Study with baseline lipid measurements recorded in 1987-1991. During a mean follow-up of 18 years, the incidence of newly diagnosed CHD was low in participants with isolated low HDL: just 5%. That was similar to the 4% incidence in subjects with above average HDL and low LDL and triglycerides. In contrast, when low HDL was present in subjects with higher LDL and/or triglycerides, the incidence of CHD was higher. So was the relative risk of CHD in a multivariate analysis after adjustment for age, sex, smoking status, diabetes, and hypertension.
When low HDL was present in combination with an LDL greater than 130 mg/dL along with triglycerides elevated above cut points of 150 and 200 mg/dL, the incident CHD rates climbed to 20%-25%, with adjusted hazard ratios of 1.7-2, compared with the risk in subjects with isolated low HDL.
The Framingham Offspring Study is funded by the National Heart, Lung, and Blood Institute. Dr. Miller reported receiving a research grant from Amgen.
AT ACC 14
When low HDL means ‘no sweat’
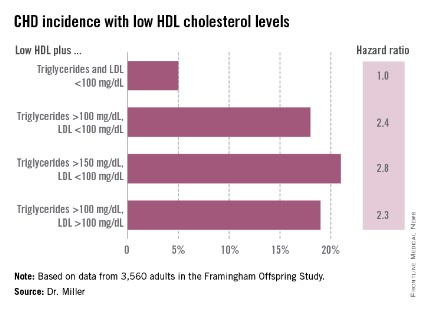
WASHINGTON– Low HDL cholesterol does not increase the risk of coronary heart disease when LDL cholesterol and triglyceride levels are normal, according to an analysis from the Framingham Offspring Study.
"In the Framingham Offspring Study, isolated HDL levels lower than the median are associated with a low risk of CHD. These data suggest that isolated low HDL may not be an atherogenic phenotype, Dr. Michael Miller said at the annual meeting of the American College of Cardiology.
While it’s well established that low HDL is associated with increased CHD risk, the risk in patients with isolated low HDL hasn’t been well studied. Yet low HDL together with an LDL below 100 mg/dL and a triglyceride level below 100 mg/dL is not a rare combination. It represented 7.4% of all study participants with low HDL, as defined by a level below the median, meaning less than 42 mg/dL in men and 54 mg/dL in women, noted Dr. Miller, professor of medicine, epidemiology, and preventive medicine and director of the center for preventive cardiology at the University of Maryland, Baltimore.
He reported on 3,560 adults in the Framingham Offspring Study with baseline lipid measurements recorded in 1987-1991. During a mean follow-up of 18 years, the incidence of newly diagnosed CHD was low in participants with isolated low HDL: just 5%. That was similar to the 4% incidence in subjects with above average HDL and low LDL and triglycerides. In contrast, when low HDL was present in subjects with higher LDL and/or triglycerides, the incidence of CHD was higher. So was the relative risk of CHD in a multivariate analysis after adjustment for age, sex, smoking status, diabetes, and hypertension.
When low HDL was present in combination with an LDL greater than 130 mg/dL along with triglycerides elevated above cut points of 150 and 200 mg/dL, the incident CHD rates climbed to 20%-25%, with adjusted hazard ratios of 1.7-2, compared with the risk in subjects with isolated low HDL.
The Framingham Offspring Study is funded by the National Heart, Lung, and Blood Institute. Dr. Miller reported receiving a research grant from Amgen.
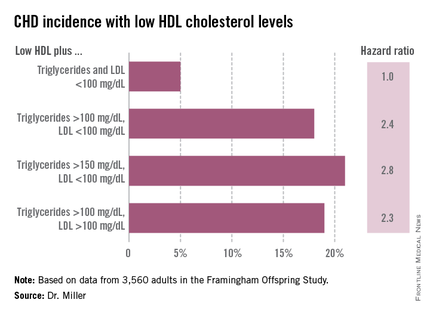
WASHINGTON– Low HDL cholesterol does not increase the risk of coronary heart disease when LDL cholesterol and triglyceride levels are normal, according to an analysis from the Framingham Offspring Study.
"In the Framingham Offspring Study, isolated HDL levels lower than the median are associated with a low risk of CHD. These data suggest that isolated low HDL may not be an atherogenic phenotype, Dr. Michael Miller said at the annual meeting of the American College of Cardiology.
While it’s well established that low HDL is associated with increased CHD risk, the risk in patients with isolated low HDL hasn’t been well studied. Yet low HDL together with an LDL below 100 mg/dL and a triglyceride level below 100 mg/dL is not a rare combination. It represented 7.4% of all study participants with low HDL, as defined by a level below the median, meaning less than 42 mg/dL in men and 54 mg/dL in women, noted Dr. Miller, professor of medicine, epidemiology, and preventive medicine and director of the center for preventive cardiology at the University of Maryland, Baltimore.
He reported on 3,560 adults in the Framingham Offspring Study with baseline lipid measurements recorded in 1987-1991. During a mean follow-up of 18 years, the incidence of newly diagnosed CHD was low in participants with isolated low HDL: just 5%. That was similar to the 4% incidence in subjects with above average HDL and low LDL and triglycerides. In contrast, when low HDL was present in subjects with higher LDL and/or triglycerides, the incidence of CHD was higher. So was the relative risk of CHD in a multivariate analysis after adjustment for age, sex, smoking status, diabetes, and hypertension.
When low HDL was present in combination with an LDL greater than 130 mg/dL along with triglycerides elevated above cut points of 150 and 200 mg/dL, the incident CHD rates climbed to 20%-25%, with adjusted hazard ratios of 1.7-2, compared with the risk in subjects with isolated low HDL.
The Framingham Offspring Study is funded by the National Heart, Lung, and Blood Institute. Dr. Miller reported receiving a research grant from Amgen.
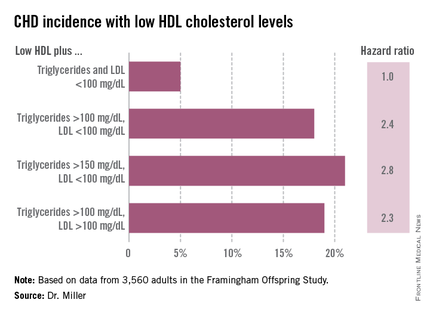
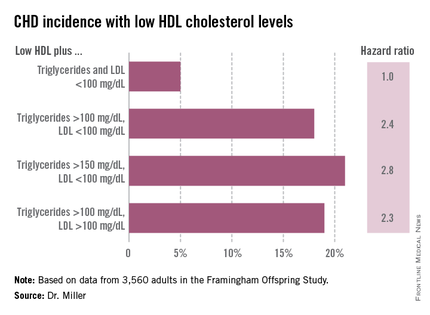
WASHINGTON– Low HDL cholesterol does not increase the risk of coronary heart disease when LDL cholesterol and triglyceride levels are normal, according to an analysis from the Framingham Offspring Study.
"In the Framingham Offspring Study, isolated HDL levels lower than the median are associated with a low risk of CHD. These data suggest that isolated low HDL may not be an atherogenic phenotype, Dr. Michael Miller said at the annual meeting of the American College of Cardiology.
While it’s well established that low HDL is associated with increased CHD risk, the risk in patients with isolated low HDL hasn’t been well studied. Yet low HDL together with an LDL below 100 mg/dL and a triglyceride level below 100 mg/dL is not a rare combination. It represented 7.4% of all study participants with low HDL, as defined by a level below the median, meaning less than 42 mg/dL in men and 54 mg/dL in women, noted Dr. Miller, professor of medicine, epidemiology, and preventive medicine and director of the center for preventive cardiology at the University of Maryland, Baltimore.
He reported on 3,560 adults in the Framingham Offspring Study with baseline lipid measurements recorded in 1987-1991. During a mean follow-up of 18 years, the incidence of newly diagnosed CHD was low in participants with isolated low HDL: just 5%. That was similar to the 4% incidence in subjects with above average HDL and low LDL and triglycerides. In contrast, when low HDL was present in subjects with higher LDL and/or triglycerides, the incidence of CHD was higher. So was the relative risk of CHD in a multivariate analysis after adjustment for age, sex, smoking status, diabetes, and hypertension.
When low HDL was present in combination with an LDL greater than 130 mg/dL along with triglycerides elevated above cut points of 150 and 200 mg/dL, the incident CHD rates climbed to 20%-25%, with adjusted hazard ratios of 1.7-2, compared with the risk in subjects with isolated low HDL.
The Framingham Offspring Study is funded by the National Heart, Lung, and Blood Institute. Dr. Miller reported receiving a research grant from Amgen.
AT ACC 14
Major finding: Adults with low HDL cholesterol coupled with an LDL cholesterol below 100 mg/dL and a triglyceride level below 100 mg/dL had a very low rate of incident coronary heart disease during long-term follow-up.
Data source: The Framingham Offspring Study is an ongoing long-term prospective epidemiologic study. This analysis focused on 3,560 subjects with a mean 18 years of follow-up after their baseline lipid levels were obtained.
Disclosures: The Framingham Offspring Study is funded by the National Heart, Lung, and Blood Institute. Dr. Miller reported receiving a research grant from Amgen.
Life partner provides better heart failure outcomes
WASHINGTON – Marital status plays an underappreciated role in heart failure prognosis.
Indeed, having a life partner was independently associated with a 12% reduction in the risk of all-cause mortality or hospitalization during a median follow-up of 2.5 years in the randomized HF-ACTION trial, Dr. Robert J. Mentz reported at the annual meeting of the American College of Cardiology.
HF-ACTION (Heart Failure: A Controlled Trial Investigating Outcomes in Exercise Training) was an 82-center, randomized trial examining the effects of exercise training in 2,331 heart failure patients with a left ventricular ejection fraction of 35% or less. The primary outcome has been reported previously (JAMA 2009;301:1439-50). In this new secondary analysis, Dr. Mentz and coinvestigators scrutinized the independent impacts of marital status, education level, and economic status on outcomes.
Of HF-ACTION participants, 61% had a current life partner at baseline, 60% had more than a high school education, and 59% had an annual income of at least $25,000. In a multivariate analysis controlling for demographics, comorbid conditions, heart failure etiology, and other potential confounders, life partner status was independently associated with a 12% lower composite event rate for all-cause mortality/hospitalization; education level and income didn’t have significant prognostic value, according to Dr. Mentz, a cardiologist at Duke University, Durham, N.C.
As this was a secondary analysis, the findings should be considered hypothesis generating. "Future prospective studies of social support interventions may be warranted to improve outcomes in this patient population," he observed.
Modern management of heart failure is complex, and fatigue is a prominent symptom. Possible mechanisms that might explain the observed benefit of life partnership in terms of patient outcomes include having someone at home to make sure the patient is taking medications appropriately. The spouse or life partner can also function as a second set of ears during clinic visits.
"When you’re in the physician’s office and information and instructions are coming at you like water out of a fire hose, your partner is there to write things down and help you remember points," Dr. Mentz noted.
The HF-ACTION trial was sponsored by the National Heart, Lung, and Blood Institute. Dr. Mentz reported having no relevant financial interests.
WASHINGTON – Marital status plays an underappreciated role in heart failure prognosis.
Indeed, having a life partner was independently associated with a 12% reduction in the risk of all-cause mortality or hospitalization during a median follow-up of 2.5 years in the randomized HF-ACTION trial, Dr. Robert J. Mentz reported at the annual meeting of the American College of Cardiology.
HF-ACTION (Heart Failure: A Controlled Trial Investigating Outcomes in Exercise Training) was an 82-center, randomized trial examining the effects of exercise training in 2,331 heart failure patients with a left ventricular ejection fraction of 35% or less. The primary outcome has been reported previously (JAMA 2009;301:1439-50). In this new secondary analysis, Dr. Mentz and coinvestigators scrutinized the independent impacts of marital status, education level, and economic status on outcomes.
Of HF-ACTION participants, 61% had a current life partner at baseline, 60% had more than a high school education, and 59% had an annual income of at least $25,000. In a multivariate analysis controlling for demographics, comorbid conditions, heart failure etiology, and other potential confounders, life partner status was independently associated with a 12% lower composite event rate for all-cause mortality/hospitalization; education level and income didn’t have significant prognostic value, according to Dr. Mentz, a cardiologist at Duke University, Durham, N.C.
As this was a secondary analysis, the findings should be considered hypothesis generating. "Future prospective studies of social support interventions may be warranted to improve outcomes in this patient population," he observed.
Modern management of heart failure is complex, and fatigue is a prominent symptom. Possible mechanisms that might explain the observed benefit of life partnership in terms of patient outcomes include having someone at home to make sure the patient is taking medications appropriately. The spouse or life partner can also function as a second set of ears during clinic visits.
"When you’re in the physician’s office and information and instructions are coming at you like water out of a fire hose, your partner is there to write things down and help you remember points," Dr. Mentz noted.
The HF-ACTION trial was sponsored by the National Heart, Lung, and Blood Institute. Dr. Mentz reported having no relevant financial interests.
WASHINGTON – Marital status plays an underappreciated role in heart failure prognosis.
Indeed, having a life partner was independently associated with a 12% reduction in the risk of all-cause mortality or hospitalization during a median follow-up of 2.5 years in the randomized HF-ACTION trial, Dr. Robert J. Mentz reported at the annual meeting of the American College of Cardiology.
HF-ACTION (Heart Failure: A Controlled Trial Investigating Outcomes in Exercise Training) was an 82-center, randomized trial examining the effects of exercise training in 2,331 heart failure patients with a left ventricular ejection fraction of 35% or less. The primary outcome has been reported previously (JAMA 2009;301:1439-50). In this new secondary analysis, Dr. Mentz and coinvestigators scrutinized the independent impacts of marital status, education level, and economic status on outcomes.
Of HF-ACTION participants, 61% had a current life partner at baseline, 60% had more than a high school education, and 59% had an annual income of at least $25,000. In a multivariate analysis controlling for demographics, comorbid conditions, heart failure etiology, and other potential confounders, life partner status was independently associated with a 12% lower composite event rate for all-cause mortality/hospitalization; education level and income didn’t have significant prognostic value, according to Dr. Mentz, a cardiologist at Duke University, Durham, N.C.
As this was a secondary analysis, the findings should be considered hypothesis generating. "Future prospective studies of social support interventions may be warranted to improve outcomes in this patient population," he observed.
Modern management of heart failure is complex, and fatigue is a prominent symptom. Possible mechanisms that might explain the observed benefit of life partnership in terms of patient outcomes include having someone at home to make sure the patient is taking medications appropriately. The spouse or life partner can also function as a second set of ears during clinic visits.
"When you’re in the physician’s office and information and instructions are coming at you like water out of a fire hose, your partner is there to write things down and help you remember points," Dr. Mentz noted.
The HF-ACTION trial was sponsored by the National Heart, Lung, and Blood Institute. Dr. Mentz reported having no relevant financial interests.
AT ACC 14
Major finding: Having a current life partner was independently associated with a 12% reduction in the risk of all-cause mortality or hospitalization among patients with heart failure.
Data source: This was a secondary analysis of data from a prospective 82-center study involving 2,331 patients with heart failure and a left ventricular ejection fraction of 35% or less who were followed for a median of 2.5 years.
Disclosures: The HF-ACTION trial was sponsored by the NHLBI. The presenter reported having no relevant financial interests.
Insertable monitor reveals AF in 30% of cryptogenic stroke patients
WASHINGTON – Continuous cardiac monitoring via Medtronic’s insertable REVEAL XT device resulted in detection of atrial fibrillation in 30% of cryptogenic stroke patients at 36 months of follow-up in the CRYSTAL AF trial.
In stark contrast, the AF detection rate was a mere 3% in the control group randomized to standard monitoring with serial ECGs and Holter monitoring, Dr. Rod S. Passman reported at the annual meeting of the American College of Cardiology.
Seventy-seven percent of first episodes of AF detected through 36 months were asymptomatic.
"These data support the use of long-term continuous cardiac monitoring in patients with cryptogenic stroke," concluded Dr. Passman, medical director of the program for atrial fibrillation at the Bluhm Cardiovascular Institute at Northwestern University, Chicago.
Thirty percent of all strokes are cryptogenic; that is, of unknown mechanism despite a thorough workup. The rationale underlying the CRYSTAL AF (Cryptogenic Stroke and Underlying Atrial Fibrillation) study was that many of these strokes are actually due to AF, which has gone undetected by conventional methods. The detection of AF in a patient with a history of ischemic stroke warrants initiation of long-term oral anticoagulation therapy, the cardiologist noted.
The CRYSTAL AF study randomized 441 cryptogenic stroke patients to the REVEAL XT insertable cardiac monitor (ICM) or conventional monitoring for possible AF. The 6- and 12-month outcomes were presented earlier this year at the International Stroke Conference. The AF detection rates were significantly higher in the ICM group at both time points. At ACC 14, Dr. Passman presented the updated 36-month outcomes.
The median time from randomization to AF detection was 8.4 months in the ICM recipients. That’s well beyond the time frame during which external monitoring can realistically be used, he noted.
Fully 95% of patients with AF detected via ICM had at least 1 day with an episode duration greater than 6 minutes. Among patients with AF detected by ICM within the first 12 months, about half had one or more episodes of 12 hours duration or longer.
The detection of five cases of AF through 36 months in the control group required considerable use of resources, including 202 ECGs and 52 Holter monitoring sessions.
When AF was discovered in patients in either arm of the study, physicians took action. In 90% of cases, patients were switched from antiplatelet therapy to an oral anticoagulant, even though that measure wasn’t addressed in the study protocol.
Dr. Passman said that in order to avoid using an ICM in all patients with cryptogenic stroke, investigators are now trying to develop a prediction rule that can identify those at highest risk of having AF. So far, age and left atrial size as determined using transesophageal echocardiography are among the better predictors.
Session cochair Dr. Yochai Birnbaum expressed reservations regarding whole-hog adoption of the ICM approach to AF detection.
"We are getting to a situation here like with ultrasensitive troponin assays," the cardiologist observed. "We now have very sensitive tools, and we tend to look at AF as an all or none cause of stroke. But the question for me is: Is 10 minutes of atrial fibrillation that is detected occasionally – not every day – really a risk for stroke? What I’m missing here in CRYSTAL AF is a control group of patients without a history of stroke who had a REVEAL XT monitor for 3 years, asking the question, ‘How often do you detect short runs of AF?’ "
"If we are saying 30% of cryptogenic stroke patients will eventually have evidence of atrial fibrillation, then it might be cheaper to treat all of the people from the beginning with an oral anticoagulant," added Dr. Birnbaum, professor of medicine at Baylor College of Medicine, Houston.
Dr. Passman conceded that the burden of AF needed to have a stroke remains unknown, as does the extent of AF in an age-matched, disease-matched population without cryptogenic stroke.
"But we do know that we have good therapies to prevent stroke in patients who have AF, and that patients with cryptogenic stroke are a high-risk population. Whether their AF is causal or not is something we can debate, but certainly finding AF is important," he countered.
The leadless Reveal XT ICM is implanted in a simple 15- to 30-minute outpatient procedure done under local anesthesia. The MRI-compatible device can be followed remotely and includes an automatic AF detection algorithm.
The CRYSTAL AF study was funded by Medtronic. Dr. Passman reported receiving research funds from and serving as a consultant to as well as on the speakers bureau for the company. In addition, he is on speakers bureaus for Pfizer, Bristol-Myers Squibb, Janssen, and Boehringer Ingelheim.
WASHINGTON – Continuous cardiac monitoring via Medtronic’s insertable REVEAL XT device resulted in detection of atrial fibrillation in 30% of cryptogenic stroke patients at 36 months of follow-up in the CRYSTAL AF trial.
In stark contrast, the AF detection rate was a mere 3% in the control group randomized to standard monitoring with serial ECGs and Holter monitoring, Dr. Rod S. Passman reported at the annual meeting of the American College of Cardiology.
Seventy-seven percent of first episodes of AF detected through 36 months were asymptomatic.
"These data support the use of long-term continuous cardiac monitoring in patients with cryptogenic stroke," concluded Dr. Passman, medical director of the program for atrial fibrillation at the Bluhm Cardiovascular Institute at Northwestern University, Chicago.
Thirty percent of all strokes are cryptogenic; that is, of unknown mechanism despite a thorough workup. The rationale underlying the CRYSTAL AF (Cryptogenic Stroke and Underlying Atrial Fibrillation) study was that many of these strokes are actually due to AF, which has gone undetected by conventional methods. The detection of AF in a patient with a history of ischemic stroke warrants initiation of long-term oral anticoagulation therapy, the cardiologist noted.
The CRYSTAL AF study randomized 441 cryptogenic stroke patients to the REVEAL XT insertable cardiac monitor (ICM) or conventional monitoring for possible AF. The 6- and 12-month outcomes were presented earlier this year at the International Stroke Conference. The AF detection rates were significantly higher in the ICM group at both time points. At ACC 14, Dr. Passman presented the updated 36-month outcomes.
The median time from randomization to AF detection was 8.4 months in the ICM recipients. That’s well beyond the time frame during which external monitoring can realistically be used, he noted.
Fully 95% of patients with AF detected via ICM had at least 1 day with an episode duration greater than 6 minutes. Among patients with AF detected by ICM within the first 12 months, about half had one or more episodes of 12 hours duration or longer.
The detection of five cases of AF through 36 months in the control group required considerable use of resources, including 202 ECGs and 52 Holter monitoring sessions.
When AF was discovered in patients in either arm of the study, physicians took action. In 90% of cases, patients were switched from antiplatelet therapy to an oral anticoagulant, even though that measure wasn’t addressed in the study protocol.
Dr. Passman said that in order to avoid using an ICM in all patients with cryptogenic stroke, investigators are now trying to develop a prediction rule that can identify those at highest risk of having AF. So far, age and left atrial size as determined using transesophageal echocardiography are among the better predictors.
Session cochair Dr. Yochai Birnbaum expressed reservations regarding whole-hog adoption of the ICM approach to AF detection.
"We are getting to a situation here like with ultrasensitive troponin assays," the cardiologist observed. "We now have very sensitive tools, and we tend to look at AF as an all or none cause of stroke. But the question for me is: Is 10 minutes of atrial fibrillation that is detected occasionally – not every day – really a risk for stroke? What I’m missing here in CRYSTAL AF is a control group of patients without a history of stroke who had a REVEAL XT monitor for 3 years, asking the question, ‘How often do you detect short runs of AF?’ "
"If we are saying 30% of cryptogenic stroke patients will eventually have evidence of atrial fibrillation, then it might be cheaper to treat all of the people from the beginning with an oral anticoagulant," added Dr. Birnbaum, professor of medicine at Baylor College of Medicine, Houston.
Dr. Passman conceded that the burden of AF needed to have a stroke remains unknown, as does the extent of AF in an age-matched, disease-matched population without cryptogenic stroke.
"But we do know that we have good therapies to prevent stroke in patients who have AF, and that patients with cryptogenic stroke are a high-risk population. Whether their AF is causal or not is something we can debate, but certainly finding AF is important," he countered.
The leadless Reveal XT ICM is implanted in a simple 15- to 30-minute outpatient procedure done under local anesthesia. The MRI-compatible device can be followed remotely and includes an automatic AF detection algorithm.
The CRYSTAL AF study was funded by Medtronic. Dr. Passman reported receiving research funds from and serving as a consultant to as well as on the speakers bureau for the company. In addition, he is on speakers bureaus for Pfizer, Bristol-Myers Squibb, Janssen, and Boehringer Ingelheim.
WASHINGTON – Continuous cardiac monitoring via Medtronic’s insertable REVEAL XT device resulted in detection of atrial fibrillation in 30% of cryptogenic stroke patients at 36 months of follow-up in the CRYSTAL AF trial.
In stark contrast, the AF detection rate was a mere 3% in the control group randomized to standard monitoring with serial ECGs and Holter monitoring, Dr. Rod S. Passman reported at the annual meeting of the American College of Cardiology.
Seventy-seven percent of first episodes of AF detected through 36 months were asymptomatic.
"These data support the use of long-term continuous cardiac monitoring in patients with cryptogenic stroke," concluded Dr. Passman, medical director of the program for atrial fibrillation at the Bluhm Cardiovascular Institute at Northwestern University, Chicago.
Thirty percent of all strokes are cryptogenic; that is, of unknown mechanism despite a thorough workup. The rationale underlying the CRYSTAL AF (Cryptogenic Stroke and Underlying Atrial Fibrillation) study was that many of these strokes are actually due to AF, which has gone undetected by conventional methods. The detection of AF in a patient with a history of ischemic stroke warrants initiation of long-term oral anticoagulation therapy, the cardiologist noted.
The CRYSTAL AF study randomized 441 cryptogenic stroke patients to the REVEAL XT insertable cardiac monitor (ICM) or conventional monitoring for possible AF. The 6- and 12-month outcomes were presented earlier this year at the International Stroke Conference. The AF detection rates were significantly higher in the ICM group at both time points. At ACC 14, Dr. Passman presented the updated 36-month outcomes.
The median time from randomization to AF detection was 8.4 months in the ICM recipients. That’s well beyond the time frame during which external monitoring can realistically be used, he noted.
Fully 95% of patients with AF detected via ICM had at least 1 day with an episode duration greater than 6 minutes. Among patients with AF detected by ICM within the first 12 months, about half had one or more episodes of 12 hours duration or longer.
The detection of five cases of AF through 36 months in the control group required considerable use of resources, including 202 ECGs and 52 Holter monitoring sessions.
When AF was discovered in patients in either arm of the study, physicians took action. In 90% of cases, patients were switched from antiplatelet therapy to an oral anticoagulant, even though that measure wasn’t addressed in the study protocol.
Dr. Passman said that in order to avoid using an ICM in all patients with cryptogenic stroke, investigators are now trying to develop a prediction rule that can identify those at highest risk of having AF. So far, age and left atrial size as determined using transesophageal echocardiography are among the better predictors.
Session cochair Dr. Yochai Birnbaum expressed reservations regarding whole-hog adoption of the ICM approach to AF detection.
"We are getting to a situation here like with ultrasensitive troponin assays," the cardiologist observed. "We now have very sensitive tools, and we tend to look at AF as an all or none cause of stroke. But the question for me is: Is 10 minutes of atrial fibrillation that is detected occasionally – not every day – really a risk for stroke? What I’m missing here in CRYSTAL AF is a control group of patients without a history of stroke who had a REVEAL XT monitor for 3 years, asking the question, ‘How often do you detect short runs of AF?’ "
"If we are saying 30% of cryptogenic stroke patients will eventually have evidence of atrial fibrillation, then it might be cheaper to treat all of the people from the beginning with an oral anticoagulant," added Dr. Birnbaum, professor of medicine at Baylor College of Medicine, Houston.
Dr. Passman conceded that the burden of AF needed to have a stroke remains unknown, as does the extent of AF in an age-matched, disease-matched population without cryptogenic stroke.
"But we do know that we have good therapies to prevent stroke in patients who have AF, and that patients with cryptogenic stroke are a high-risk population. Whether their AF is causal or not is something we can debate, but certainly finding AF is important," he countered.
The leadless Reveal XT ICM is implanted in a simple 15- to 30-minute outpatient procedure done under local anesthesia. The MRI-compatible device can be followed remotely and includes an automatic AF detection algorithm.
The CRYSTAL AF study was funded by Medtronic. Dr. Passman reported receiving research funds from and serving as a consultant to as well as on the speakers bureau for the company. In addition, he is on speakers bureaus for Pfizer, Bristol-Myers Squibb, Janssen, and Boehringer Ingelheim.
AT ACC 14
Major finding: Newly detected atrial fibrillation was identified in 30% of cryptogenic stroke patients with an insertable cardiac monitor during 36 months of follow-up, compared with a 3% rate with standard monitoring using ECGs and Holter recordings.
Data source: The randomized, multicenter CRYSTAL AF trial included 441 cryptogenic stroke patients who were randomized to an insertable cardiac monitor or conventional monitoring and prospectively followed.
Disclosures: The study was funded by Medtronic. The presenter is a consultant to and on the speakers bureau for the company.
Post-MI beta-blockers: Less is more
WASHINGTON – Physicians seldom prescribe beta-blockers post MI in the full doses shown to improve survival in the classic randomized clinical trials conducted several decades ago, according to a large new study – and that, as it turns out, is a very good thing.
Results of the OBTAIN (Optimal Beta-Blocker Therapy After Myocardial Infarction) registry indicate that 2-year mortality post MI is lowest in patients discharged on a dose that’s roughly just 25% of target doses established in the landmark randomized trials, Dr. Jeffrey Goldberger reported at the annual meeting of the American College of Cardiology.
Two-year mortality post MI discharge followed a J-shaped curve: It was lowest, at 9.4%, in patients on about 25% of the target dose, and worst, at 14.9%, among those on more than 50% of the target dose. Mortality was intermediate in those whose beta-blocker dose hovered around either 12% or 50%. And patients on any of these four commonly prescribed dosing regimens fared significantly better than those who weren’t discharged on a beta-blocker, whose 2-year mortality was 21.7%, reported Dr. Goldberger, professor of medicine at Northwestern University in Chicago.
"Based on these data, we feel that following an MI it is important to treat patients with a beta-blocker. However, achieving the target doses used in prior randomized clinical trials is neither necessary nor desirable," he declared.
Quality improvement initiatives implemented in the past decade have resulted in greater than 90% utilization of beta-blockers after MI. However, practice guidelines don’t recommend specific beta-blockers or target doses. The OBTAIN registry was created in order to pin down the optimal dosing. The study hypothesis was that achieving target doses would be associated with better survival than with lower doses. Not so, investigators discovered.
The OBTAIN registry included 7,057 acute MI patients enrolled at 26 participating centers. In-hospital mortality was 4.7%. Of those patients who survived to discharge, 91.5% left the hospital on a beta-blocker. Metoprolol was prescribed in two-thirds of patients. The second most frequently prescribed beta-blocker post MI was carvedilol, utilized in one-quarter of patients.
The target daily doses normalized to those established in the landmark randomized trials as having a survival benefit are metoprolol 200 mg, carvedilol 50 mg, atenolol 100 mg, bisoprolol 10 mg, propranolol 180 mg, and timolol 20 mg.
Thirty-seven percent of patients discharged on a beta-blocker were on roughly 25% of the target dose. Roughly 25% of patients were on 12% of the target dose, a similar proportion got 50% of the target dose, and a mere 13% got more than 50% of the target dose. Three weeks post discharge, three-quarters of patients were on the same dose as when they left the hospital. Half of the rest had been titrated to a higher dose, the other half to a lower one.
In a multivariate analysis adjusted for demographics, diabetes and other comorbid conditions, ST-elevation MI, in-hospital therapies and length of stay, and other discharge medications, patients discharged on a beta-blocker had a 38%-51% lower mortality than those not on a beta-blocker. The most common reason that patients weren’t on a beta-blocker at discharge was hypotension.
Session cochair Dr. Yochai Birnbaum observed that the landmark randomized trials showing a mortality benefit for post-MI beta-blocker therapy were carried out in an era before statins and other potent secondary prevention therapies.
"It might be that when we add more and more medications, there are some interactions that are unclear. Maybe the previous recommendations are no longer valid," said Dr. Birnbaum, professor of medicine at Baylor College of Medicine, Houston.
The OBTAIN registry was sponsored by the National Heart, Lung, and Blood Institute. Dr. Goldberger reported having no relevant financial relationships.
WASHINGTON – Physicians seldom prescribe beta-blockers post MI in the full doses shown to improve survival in the classic randomized clinical trials conducted several decades ago, according to a large new study – and that, as it turns out, is a very good thing.
Results of the OBTAIN (Optimal Beta-Blocker Therapy After Myocardial Infarction) registry indicate that 2-year mortality post MI is lowest in patients discharged on a dose that’s roughly just 25% of target doses established in the landmark randomized trials, Dr. Jeffrey Goldberger reported at the annual meeting of the American College of Cardiology.
Two-year mortality post MI discharge followed a J-shaped curve: It was lowest, at 9.4%, in patients on about 25% of the target dose, and worst, at 14.9%, among those on more than 50% of the target dose. Mortality was intermediate in those whose beta-blocker dose hovered around either 12% or 50%. And patients on any of these four commonly prescribed dosing regimens fared significantly better than those who weren’t discharged on a beta-blocker, whose 2-year mortality was 21.7%, reported Dr. Goldberger, professor of medicine at Northwestern University in Chicago.
"Based on these data, we feel that following an MI it is important to treat patients with a beta-blocker. However, achieving the target doses used in prior randomized clinical trials is neither necessary nor desirable," he declared.
Quality improvement initiatives implemented in the past decade have resulted in greater than 90% utilization of beta-blockers after MI. However, practice guidelines don’t recommend specific beta-blockers or target doses. The OBTAIN registry was created in order to pin down the optimal dosing. The study hypothesis was that achieving target doses would be associated with better survival than with lower doses. Not so, investigators discovered.
The OBTAIN registry included 7,057 acute MI patients enrolled at 26 participating centers. In-hospital mortality was 4.7%. Of those patients who survived to discharge, 91.5% left the hospital on a beta-blocker. Metoprolol was prescribed in two-thirds of patients. The second most frequently prescribed beta-blocker post MI was carvedilol, utilized in one-quarter of patients.
The target daily doses normalized to those established in the landmark randomized trials as having a survival benefit are metoprolol 200 mg, carvedilol 50 mg, atenolol 100 mg, bisoprolol 10 mg, propranolol 180 mg, and timolol 20 mg.
Thirty-seven percent of patients discharged on a beta-blocker were on roughly 25% of the target dose. Roughly 25% of patients were on 12% of the target dose, a similar proportion got 50% of the target dose, and a mere 13% got more than 50% of the target dose. Three weeks post discharge, three-quarters of patients were on the same dose as when they left the hospital. Half of the rest had been titrated to a higher dose, the other half to a lower one.
In a multivariate analysis adjusted for demographics, diabetes and other comorbid conditions, ST-elevation MI, in-hospital therapies and length of stay, and other discharge medications, patients discharged on a beta-blocker had a 38%-51% lower mortality than those not on a beta-blocker. The most common reason that patients weren’t on a beta-blocker at discharge was hypotension.
Session cochair Dr. Yochai Birnbaum observed that the landmark randomized trials showing a mortality benefit for post-MI beta-blocker therapy were carried out in an era before statins and other potent secondary prevention therapies.
"It might be that when we add more and more medications, there are some interactions that are unclear. Maybe the previous recommendations are no longer valid," said Dr. Birnbaum, professor of medicine at Baylor College of Medicine, Houston.
The OBTAIN registry was sponsored by the National Heart, Lung, and Blood Institute. Dr. Goldberger reported having no relevant financial relationships.
WASHINGTON – Physicians seldom prescribe beta-blockers post MI in the full doses shown to improve survival in the classic randomized clinical trials conducted several decades ago, according to a large new study – and that, as it turns out, is a very good thing.
Results of the OBTAIN (Optimal Beta-Blocker Therapy After Myocardial Infarction) registry indicate that 2-year mortality post MI is lowest in patients discharged on a dose that’s roughly just 25% of target doses established in the landmark randomized trials, Dr. Jeffrey Goldberger reported at the annual meeting of the American College of Cardiology.
Two-year mortality post MI discharge followed a J-shaped curve: It was lowest, at 9.4%, in patients on about 25% of the target dose, and worst, at 14.9%, among those on more than 50% of the target dose. Mortality was intermediate in those whose beta-blocker dose hovered around either 12% or 50%. And patients on any of these four commonly prescribed dosing regimens fared significantly better than those who weren’t discharged on a beta-blocker, whose 2-year mortality was 21.7%, reported Dr. Goldberger, professor of medicine at Northwestern University in Chicago.
"Based on these data, we feel that following an MI it is important to treat patients with a beta-blocker. However, achieving the target doses used in prior randomized clinical trials is neither necessary nor desirable," he declared.
Quality improvement initiatives implemented in the past decade have resulted in greater than 90% utilization of beta-blockers after MI. However, practice guidelines don’t recommend specific beta-blockers or target doses. The OBTAIN registry was created in order to pin down the optimal dosing. The study hypothesis was that achieving target doses would be associated with better survival than with lower doses. Not so, investigators discovered.
The OBTAIN registry included 7,057 acute MI patients enrolled at 26 participating centers. In-hospital mortality was 4.7%. Of those patients who survived to discharge, 91.5% left the hospital on a beta-blocker. Metoprolol was prescribed in two-thirds of patients. The second most frequently prescribed beta-blocker post MI was carvedilol, utilized in one-quarter of patients.
The target daily doses normalized to those established in the landmark randomized trials as having a survival benefit are metoprolol 200 mg, carvedilol 50 mg, atenolol 100 mg, bisoprolol 10 mg, propranolol 180 mg, and timolol 20 mg.
Thirty-seven percent of patients discharged on a beta-blocker were on roughly 25% of the target dose. Roughly 25% of patients were on 12% of the target dose, a similar proportion got 50% of the target dose, and a mere 13% got more than 50% of the target dose. Three weeks post discharge, three-quarters of patients were on the same dose as when they left the hospital. Half of the rest had been titrated to a higher dose, the other half to a lower one.
In a multivariate analysis adjusted for demographics, diabetes and other comorbid conditions, ST-elevation MI, in-hospital therapies and length of stay, and other discharge medications, patients discharged on a beta-blocker had a 38%-51% lower mortality than those not on a beta-blocker. The most common reason that patients weren’t on a beta-blocker at discharge was hypotension.
Session cochair Dr. Yochai Birnbaum observed that the landmark randomized trials showing a mortality benefit for post-MI beta-blocker therapy were carried out in an era before statins and other potent secondary prevention therapies.
"It might be that when we add more and more medications, there are some interactions that are unclear. Maybe the previous recommendations are no longer valid," said Dr. Birnbaum, professor of medicine at Baylor College of Medicine, Houston.
The OBTAIN registry was sponsored by the National Heart, Lung, and Blood Institute. Dr. Goldberger reported having no relevant financial relationships.
AT ACC 14
Major finding: Patients discharged post MI on a beta-blocker at roughly 25% of the target dose – which was established as conferring a survival benefit in the earlier, classic randomized trials – had a significantly lower 2-year mortality than those discharged on higher or lower doses.
Data source: The observational OBTAIN registry included more than 7,000 acute MI patients at 26 sites.
Disclosures: Dr. Goldberger reported having no financial conflicts with regard to the National Heart, Lung, and Blood Institute–sponsored registry.