User login
Marijuana May Lower Death Risk After Acute MI
CHICAGO – Patients who reported using marijuana prior to experiencing an acute MI had significantly lower in-hospital mortality and were less likely to have cardiogenic shock or require an intra-aortic balloon pump than marijuana nonusers with an MI in an eight-state hospital records study, Dr. Cecelia P. Johnson-Sasso reported at the annual meeting of the American College of Cardiology.
“If this observation is confirmed in independent studies, further investigation into the possible therapeutic benefit of cannabinoid receptor agonists in acute MI may be warranted,” declared Dr. Johnson-Sasso of the University of Colorado Denver.
She and her coinvestigators obtained hospital records with identity information removed for more than 3 million patients admitted for acute MI during 1994-2013 in eight states: California, Colorado, New Hampshire, New Jersey, New York, Texas, Vermont, and West Virginia.
After excluding concomitant users of cocaine, methamphetamine, or alcohol due to the potential for confounding cardiotoxic effects; MI patients under age 19 because of the likelihood of congenital heart disease; and patients over age 70 because only 0.01% of them admitted to marijuana use, the investigators were left with a study population of 3,854 marijuana users and 1.27 million MI patients who hadn’t used marijuana.
In a multivariate regression analysis adjusted for potential confounders including baseline comorbid conditions, patient demographics, and payer status, the marijuana users prior to MI had a 17% reduction in in-hospital mortality, were 20% less likely to undergo intra-aortic balloon pump placement, and had a 26% reduction in shock. On the other hand, they were also 19% more likely than marijuana nonusers to be placed on mechanical ventilation. And even though they were equally likely to undergo diagnostic coronary angiography, they were 28% less likely than marijuana nonusers to undergo percutaneous coronary intervention. All of these differences were statistically significant and clinically meaningful.
She was quick to note the limitations of her study: No data were available on readmissions or late mortality, and it’s highly likely that marijuana use by patients with acute MI was significantly underreported during the study period, which was largely before the legalization movement took off.
With state marijuana laws rapidly changing and the legal pot industry becoming a big business, the lack of research into the health consequences of marijuana by disinterested parties has become glaringly obvious, according to Dr. Johnson-Sasso. Cannabinoid receptors are found not only in the brain, but in cardiac muscle, the kidney, liver, vascular and visceral muscle, aorta, bladder, and immune cells.
She reported having no financial conflicts of interest regarding this study.
CHICAGO – Patients who reported using marijuana prior to experiencing an acute MI had significantly lower in-hospital mortality and were less likely to have cardiogenic shock or require an intra-aortic balloon pump than marijuana nonusers with an MI in an eight-state hospital records study, Dr. Cecelia P. Johnson-Sasso reported at the annual meeting of the American College of Cardiology.
“If this observation is confirmed in independent studies, further investigation into the possible therapeutic benefit of cannabinoid receptor agonists in acute MI may be warranted,” declared Dr. Johnson-Sasso of the University of Colorado Denver.
She and her coinvestigators obtained hospital records with identity information removed for more than 3 million patients admitted for acute MI during 1994-2013 in eight states: California, Colorado, New Hampshire, New Jersey, New York, Texas, Vermont, and West Virginia.
After excluding concomitant users of cocaine, methamphetamine, or alcohol due to the potential for confounding cardiotoxic effects; MI patients under age 19 because of the likelihood of congenital heart disease; and patients over age 70 because only 0.01% of them admitted to marijuana use, the investigators were left with a study population of 3,854 marijuana users and 1.27 million MI patients who hadn’t used marijuana.
In a multivariate regression analysis adjusted for potential confounders including baseline comorbid conditions, patient demographics, and payer status, the marijuana users prior to MI had a 17% reduction in in-hospital mortality, were 20% less likely to undergo intra-aortic balloon pump placement, and had a 26% reduction in shock. On the other hand, they were also 19% more likely than marijuana nonusers to be placed on mechanical ventilation. And even though they were equally likely to undergo diagnostic coronary angiography, they were 28% less likely than marijuana nonusers to undergo percutaneous coronary intervention. All of these differences were statistically significant and clinically meaningful.
She was quick to note the limitations of her study: No data were available on readmissions or late mortality, and it’s highly likely that marijuana use by patients with acute MI was significantly underreported during the study period, which was largely before the legalization movement took off.
With state marijuana laws rapidly changing and the legal pot industry becoming a big business, the lack of research into the health consequences of marijuana by disinterested parties has become glaringly obvious, according to Dr. Johnson-Sasso. Cannabinoid receptors are found not only in the brain, but in cardiac muscle, the kidney, liver, vascular and visceral muscle, aorta, bladder, and immune cells.
She reported having no financial conflicts of interest regarding this study.
CHICAGO – Patients who reported using marijuana prior to experiencing an acute MI had significantly lower in-hospital mortality and were less likely to have cardiogenic shock or require an intra-aortic balloon pump than marijuana nonusers with an MI in an eight-state hospital records study, Dr. Cecelia P. Johnson-Sasso reported at the annual meeting of the American College of Cardiology.
“If this observation is confirmed in independent studies, further investigation into the possible therapeutic benefit of cannabinoid receptor agonists in acute MI may be warranted,” declared Dr. Johnson-Sasso of the University of Colorado Denver.
She and her coinvestigators obtained hospital records with identity information removed for more than 3 million patients admitted for acute MI during 1994-2013 in eight states: California, Colorado, New Hampshire, New Jersey, New York, Texas, Vermont, and West Virginia.
After excluding concomitant users of cocaine, methamphetamine, or alcohol due to the potential for confounding cardiotoxic effects; MI patients under age 19 because of the likelihood of congenital heart disease; and patients over age 70 because only 0.01% of them admitted to marijuana use, the investigators were left with a study population of 3,854 marijuana users and 1.27 million MI patients who hadn’t used marijuana.
In a multivariate regression analysis adjusted for potential confounders including baseline comorbid conditions, patient demographics, and payer status, the marijuana users prior to MI had a 17% reduction in in-hospital mortality, were 20% less likely to undergo intra-aortic balloon pump placement, and had a 26% reduction in shock. On the other hand, they were also 19% more likely than marijuana nonusers to be placed on mechanical ventilation. And even though they were equally likely to undergo diagnostic coronary angiography, they were 28% less likely than marijuana nonusers to undergo percutaneous coronary intervention. All of these differences were statistically significant and clinically meaningful.
She was quick to note the limitations of her study: No data were available on readmissions or late mortality, and it’s highly likely that marijuana use by patients with acute MI was significantly underreported during the study period, which was largely before the legalization movement took off.
With state marijuana laws rapidly changing and the legal pot industry becoming a big business, the lack of research into the health consequences of marijuana by disinterested parties has become glaringly obvious, according to Dr. Johnson-Sasso. Cannabinoid receptors are found not only in the brain, but in cardiac muscle, the kidney, liver, vascular and visceral muscle, aorta, bladder, and immune cells.
She reported having no financial conflicts of interest regarding this study.
AT ACC 16
Marijuana may lower death risk after acute MI
CHICAGO – Patients who reported using marijuana prior to experiencing an acute MI had significantly lower in-hospital mortality and were less likely to have cardiogenic shock or require an intra-aortic balloon pump than marijuana nonusers with an MI in an eight-state hospital records study, Dr. Cecelia P. Johnson-Sasso reported at the annual meeting of the American College of Cardiology.
“If this observation is confirmed in independent studies, further investigation into the possible therapeutic benefit of cannabinoid receptor agonists in acute MI may be warranted,” declared Dr. Johnson-Sasso of the University of Colorado Denver.
She and her coinvestigators obtained hospital records with identity information removed for more than 3 million patients admitted for acute MI during 1994-2013 in eight states: California, Colorado, New Hampshire, New Jersey, New York, Texas, Vermont, and West Virginia.
After excluding concomitant users of cocaine, methamphetamine, or alcohol due to the potential for confounding cardiotoxic effects; MI patients under age 19 because of the likelihood of congenital heart disease; and patients over age 70 because only 0.01% of them admitted to marijuana use, the investigators were left with a study population of 3,854 marijuana users and 1.27 million MI patients who hadn’t used marijuana.
In a multivariate regression analysis adjusted for potential confounders including baseline comorbid conditions, patient demographics, and payer status, the marijuana users prior to MI had a 17% reduction in in-hospital mortality, were 20% less likely to undergo intra-aortic balloon pump placement, and had a 26% reduction in shock. On the other hand, they were also 19% more likely than marijuana nonusers to be placed on mechanical ventilation. And even though they were equally likely to undergo diagnostic coronary angiography, they were 28% less likely than marijuana nonusers to undergo percutaneous coronary intervention. All of these differences were statistically significant and clinically meaningful.
She was quick to note the limitations of her study: No data were available on readmissions or late mortality, and it’s highly likely that marijuana use by patients with acute MI was significantly underreported during the study period, which was largely before the legalization movement took off.
With state marijuana laws rapidly changing and the legal pot industry becoming a big business, the lack of research into the health consequences of marijuana by disinterested parties has become glaringly obvious, according to Dr. Johnson-Sasso. Cannabinoid receptors are found not only in the brain, but in cardiac muscle, the kidney, liver, vascular and visceral muscle, aorta, bladder, and immune cells.
She reported having no financial conflicts of interest regarding this study.
CHICAGO – Patients who reported using marijuana prior to experiencing an acute MI had significantly lower in-hospital mortality and were less likely to have cardiogenic shock or require an intra-aortic balloon pump than marijuana nonusers with an MI in an eight-state hospital records study, Dr. Cecelia P. Johnson-Sasso reported at the annual meeting of the American College of Cardiology.
“If this observation is confirmed in independent studies, further investigation into the possible therapeutic benefit of cannabinoid receptor agonists in acute MI may be warranted,” declared Dr. Johnson-Sasso of the University of Colorado Denver.
She and her coinvestigators obtained hospital records with identity information removed for more than 3 million patients admitted for acute MI during 1994-2013 in eight states: California, Colorado, New Hampshire, New Jersey, New York, Texas, Vermont, and West Virginia.
After excluding concomitant users of cocaine, methamphetamine, or alcohol due to the potential for confounding cardiotoxic effects; MI patients under age 19 because of the likelihood of congenital heart disease; and patients over age 70 because only 0.01% of them admitted to marijuana use, the investigators were left with a study population of 3,854 marijuana users and 1.27 million MI patients who hadn’t used marijuana.
In a multivariate regression analysis adjusted for potential confounders including baseline comorbid conditions, patient demographics, and payer status, the marijuana users prior to MI had a 17% reduction in in-hospital mortality, were 20% less likely to undergo intra-aortic balloon pump placement, and had a 26% reduction in shock. On the other hand, they were also 19% more likely than marijuana nonusers to be placed on mechanical ventilation. And even though they were equally likely to undergo diagnostic coronary angiography, they were 28% less likely than marijuana nonusers to undergo percutaneous coronary intervention. All of these differences were statistically significant and clinically meaningful.
She was quick to note the limitations of her study: No data were available on readmissions or late mortality, and it’s highly likely that marijuana use by patients with acute MI was significantly underreported during the study period, which was largely before the legalization movement took off.
With state marijuana laws rapidly changing and the legal pot industry becoming a big business, the lack of research into the health consequences of marijuana by disinterested parties has become glaringly obvious, according to Dr. Johnson-Sasso. Cannabinoid receptors are found not only in the brain, but in cardiac muscle, the kidney, liver, vascular and visceral muscle, aorta, bladder, and immune cells.
She reported having no financial conflicts of interest regarding this study.
CHICAGO – Patients who reported using marijuana prior to experiencing an acute MI had significantly lower in-hospital mortality and were less likely to have cardiogenic shock or require an intra-aortic balloon pump than marijuana nonusers with an MI in an eight-state hospital records study, Dr. Cecelia P. Johnson-Sasso reported at the annual meeting of the American College of Cardiology.
“If this observation is confirmed in independent studies, further investigation into the possible therapeutic benefit of cannabinoid receptor agonists in acute MI may be warranted,” declared Dr. Johnson-Sasso of the University of Colorado Denver.
She and her coinvestigators obtained hospital records with identity information removed for more than 3 million patients admitted for acute MI during 1994-2013 in eight states: California, Colorado, New Hampshire, New Jersey, New York, Texas, Vermont, and West Virginia.
After excluding concomitant users of cocaine, methamphetamine, or alcohol due to the potential for confounding cardiotoxic effects; MI patients under age 19 because of the likelihood of congenital heart disease; and patients over age 70 because only 0.01% of them admitted to marijuana use, the investigators were left with a study population of 3,854 marijuana users and 1.27 million MI patients who hadn’t used marijuana.
In a multivariate regression analysis adjusted for potential confounders including baseline comorbid conditions, patient demographics, and payer status, the marijuana users prior to MI had a 17% reduction in in-hospital mortality, were 20% less likely to undergo intra-aortic balloon pump placement, and had a 26% reduction in shock. On the other hand, they were also 19% more likely than marijuana nonusers to be placed on mechanical ventilation. And even though they were equally likely to undergo diagnostic coronary angiography, they were 28% less likely than marijuana nonusers to undergo percutaneous coronary intervention. All of these differences were statistically significant and clinically meaningful.
She was quick to note the limitations of her study: No data were available on readmissions or late mortality, and it’s highly likely that marijuana use by patients with acute MI was significantly underreported during the study period, which was largely before the legalization movement took off.
With state marijuana laws rapidly changing and the legal pot industry becoming a big business, the lack of research into the health consequences of marijuana by disinterested parties has become glaringly obvious, according to Dr. Johnson-Sasso. Cannabinoid receptors are found not only in the brain, but in cardiac muscle, the kidney, liver, vascular and visceral muscle, aorta, bladder, and immune cells.
She reported having no financial conflicts of interest regarding this study.
AT ACC 16
Key clinical point: Patients who used marijuana prior to their acute MI had better outcomes.
Major finding: Marijuana use prior to acute MI was associated with a 17% reduction in in-hospital mortality.
Data source: This was a retrospective analysis of hospital records for nearly 1.3 million MI patients in eight states.
Disclosures: The study presenter reported having no financial conflicts of interest.
Stroke Risk Rises Quickly in Recent-onset Atrial Fib
CHICAGO – The stroke risk in patients with recent-onset atrial fibrillation is similar to that of patients with longer-standing atrial fibrillation, according to a new secondary analysis of the landmark ARISTOTLE trial.
“Our key message is that patients with recent-onset atrial fibrillation had a similar risk of stroke but higher mortality than patients with remotely diagnosed atrial fibrillation, suggesting that patients with recently diagnosed atrial fibrillation are not at low risk and therefore warrant stroke prevention strategies,” Dr. Patricia O. Guimaraes said in presenting the findings at the annual meeting of the American College of Cardiology.
“Sometimes we as physicians hesitate in beginning oral anticoagulation therapy for patients that we just diagnosed. And of course patients are often afraid of anticoagulation therapy. But once they present with atrial fibrillation they are already at risk, and that’s why we need to anticoagulate them promptly,” added Dr. Guimaraes of the Duke Clinical Research Institute in Durham, N.C.
The benefits of apixaban (Eliquis) over warfarin seen in the overall randomized ARISTOTLE trial (N Engl J Med. 2011; 365:981-92) were preserved in the recent-onset subset of the atrial fibrillation (AF) study population, she noted.
The rationale for this new post hoc analysis of ARISTOTLE is that virtually all of the evidence supporting anticoagulation for stroke prevention in AF is based on studies conducted in patients with permanent, persistent, or long-standing paroxysmal AF. Much less is known about stroke risk and the benefits of anticoagulation in patients with recent-onset AF, Dr. Guimaraes explained.
The 1,899 ARISTOTLE participants with AF onset within 30 days prior to enrollment comprised 10.5% of the total study population, all of whom had AF and at least one other stroke risk factor. The recent-onset subgroup was the same age as the 16,241 subjects in this analysis who had longer-standing AF, but the recent-onset group included a higher proportion of women, had a lower prevalence of CAD, and their cardiovascular risk factor profile differed from that of the remote-onset AF group.
The composite endpoint of stroke, systemic embolism, major bleeding, or all-cause mortality occurred at a rate of 8.69%/year in the recent-onset AF group, compared with 6.43%/year in the remote-onset group. However, in a multivariate regression analysis adjusted for potential confounders, the only significant differences in outcome between the two groups were in all-cause mortality – 5.15%/year in the recent-onset group, 3.15% in the remote-onset AF patients – and in the composite of stroke, systemic embolism, or all-cause mortality, which had an incidence of 6.46%/year in the recent-onset group, compared with 4.57%/year in remote-onset patients.
Turning to the impact of apixaban, Dr. Guimaraes noted that, as previously reported in the overall study, the primary endpoint of stroke or systemic embolism occurred in the apixaban group at a rate of 1.27%/year, compared with 1.6%/year with warfarin, for a 21% relative risk reduction in favor of the newer agent. She and her coinvestigators determined that in the remote-onset AF subgroup the relative risk reduction was 20%, while in the recent-onset subgroup the size of the effect was similar at 22%.
The composite safety endpoint of major or clinically relevant bleeding occurred in the remote-onset patients at a rate of 3.97%/year with apixaban versus 5.97%/year with warfarin, for a 33% relative risk reduction favoring the novel agent. In the recent-onset group, the rates were 5.04%/year with apixaban, compared with 6.4%/year with warfarin, for a 22% relative risk reduction.
Dr. Guimaraes observed an important limitation of this post hoc analysis is that the remote-onset AF group may have been selected for improved survival, since they didn’t die in the first 30 days after diagnosis.
Session co-chair Dr. Brian Olshansky commented that this analysis, which highlights the risks of recent-onset AF, argues for a strategy whereby a patient who presents to the ED with new-onset AF should get sent home on apixaban rather than being hospitalized for several days in order to be stabilized on warfarin.
“With recent-onset atrial fibrillation it’s going to take you several days to get anticoagulated with warfarin, whereas you’re immediately anticoagulated with apixaban,” said Dr. Olshansky, emeritus professor of internal medicine at the University of Iowa, Iowa City.
The ARISTOTLE trial was supported by Bristol-Myers Squibb and Pfizer. Dr. Guimaraes reported having no financial conflicts of interest.
CHICAGO – The stroke risk in patients with recent-onset atrial fibrillation is similar to that of patients with longer-standing atrial fibrillation, according to a new secondary analysis of the landmark ARISTOTLE trial.
“Our key message is that patients with recent-onset atrial fibrillation had a similar risk of stroke but higher mortality than patients with remotely diagnosed atrial fibrillation, suggesting that patients with recently diagnosed atrial fibrillation are not at low risk and therefore warrant stroke prevention strategies,” Dr. Patricia O. Guimaraes said in presenting the findings at the annual meeting of the American College of Cardiology.
“Sometimes we as physicians hesitate in beginning oral anticoagulation therapy for patients that we just diagnosed. And of course patients are often afraid of anticoagulation therapy. But once they present with atrial fibrillation they are already at risk, and that’s why we need to anticoagulate them promptly,” added Dr. Guimaraes of the Duke Clinical Research Institute in Durham, N.C.
The benefits of apixaban (Eliquis) over warfarin seen in the overall randomized ARISTOTLE trial (N Engl J Med. 2011; 365:981-92) were preserved in the recent-onset subset of the atrial fibrillation (AF) study population, she noted.
The rationale for this new post hoc analysis of ARISTOTLE is that virtually all of the evidence supporting anticoagulation for stroke prevention in AF is based on studies conducted in patients with permanent, persistent, or long-standing paroxysmal AF. Much less is known about stroke risk and the benefits of anticoagulation in patients with recent-onset AF, Dr. Guimaraes explained.
The 1,899 ARISTOTLE participants with AF onset within 30 days prior to enrollment comprised 10.5% of the total study population, all of whom had AF and at least one other stroke risk factor. The recent-onset subgroup was the same age as the 16,241 subjects in this analysis who had longer-standing AF, but the recent-onset group included a higher proportion of women, had a lower prevalence of CAD, and their cardiovascular risk factor profile differed from that of the remote-onset AF group.
The composite endpoint of stroke, systemic embolism, major bleeding, or all-cause mortality occurred at a rate of 8.69%/year in the recent-onset AF group, compared with 6.43%/year in the remote-onset group. However, in a multivariate regression analysis adjusted for potential confounders, the only significant differences in outcome between the two groups were in all-cause mortality – 5.15%/year in the recent-onset group, 3.15% in the remote-onset AF patients – and in the composite of stroke, systemic embolism, or all-cause mortality, which had an incidence of 6.46%/year in the recent-onset group, compared with 4.57%/year in remote-onset patients.
Turning to the impact of apixaban, Dr. Guimaraes noted that, as previously reported in the overall study, the primary endpoint of stroke or systemic embolism occurred in the apixaban group at a rate of 1.27%/year, compared with 1.6%/year with warfarin, for a 21% relative risk reduction in favor of the newer agent. She and her coinvestigators determined that in the remote-onset AF subgroup the relative risk reduction was 20%, while in the recent-onset subgroup the size of the effect was similar at 22%.
The composite safety endpoint of major or clinically relevant bleeding occurred in the remote-onset patients at a rate of 3.97%/year with apixaban versus 5.97%/year with warfarin, for a 33% relative risk reduction favoring the novel agent. In the recent-onset group, the rates were 5.04%/year with apixaban, compared with 6.4%/year with warfarin, for a 22% relative risk reduction.
Dr. Guimaraes observed an important limitation of this post hoc analysis is that the remote-onset AF group may have been selected for improved survival, since they didn’t die in the first 30 days after diagnosis.
Session co-chair Dr. Brian Olshansky commented that this analysis, which highlights the risks of recent-onset AF, argues for a strategy whereby a patient who presents to the ED with new-onset AF should get sent home on apixaban rather than being hospitalized for several days in order to be stabilized on warfarin.
“With recent-onset atrial fibrillation it’s going to take you several days to get anticoagulated with warfarin, whereas you’re immediately anticoagulated with apixaban,” said Dr. Olshansky, emeritus professor of internal medicine at the University of Iowa, Iowa City.
The ARISTOTLE trial was supported by Bristol-Myers Squibb and Pfizer. Dr. Guimaraes reported having no financial conflicts of interest.
CHICAGO – The stroke risk in patients with recent-onset atrial fibrillation is similar to that of patients with longer-standing atrial fibrillation, according to a new secondary analysis of the landmark ARISTOTLE trial.
“Our key message is that patients with recent-onset atrial fibrillation had a similar risk of stroke but higher mortality than patients with remotely diagnosed atrial fibrillation, suggesting that patients with recently diagnosed atrial fibrillation are not at low risk and therefore warrant stroke prevention strategies,” Dr. Patricia O. Guimaraes said in presenting the findings at the annual meeting of the American College of Cardiology.
“Sometimes we as physicians hesitate in beginning oral anticoagulation therapy for patients that we just diagnosed. And of course patients are often afraid of anticoagulation therapy. But once they present with atrial fibrillation they are already at risk, and that’s why we need to anticoagulate them promptly,” added Dr. Guimaraes of the Duke Clinical Research Institute in Durham, N.C.
The benefits of apixaban (Eliquis) over warfarin seen in the overall randomized ARISTOTLE trial (N Engl J Med. 2011; 365:981-92) were preserved in the recent-onset subset of the atrial fibrillation (AF) study population, she noted.
The rationale for this new post hoc analysis of ARISTOTLE is that virtually all of the evidence supporting anticoagulation for stroke prevention in AF is based on studies conducted in patients with permanent, persistent, or long-standing paroxysmal AF. Much less is known about stroke risk and the benefits of anticoagulation in patients with recent-onset AF, Dr. Guimaraes explained.
The 1,899 ARISTOTLE participants with AF onset within 30 days prior to enrollment comprised 10.5% of the total study population, all of whom had AF and at least one other stroke risk factor. The recent-onset subgroup was the same age as the 16,241 subjects in this analysis who had longer-standing AF, but the recent-onset group included a higher proportion of women, had a lower prevalence of CAD, and their cardiovascular risk factor profile differed from that of the remote-onset AF group.
The composite endpoint of stroke, systemic embolism, major bleeding, or all-cause mortality occurred at a rate of 8.69%/year in the recent-onset AF group, compared with 6.43%/year in the remote-onset group. However, in a multivariate regression analysis adjusted for potential confounders, the only significant differences in outcome between the two groups were in all-cause mortality – 5.15%/year in the recent-onset group, 3.15% in the remote-onset AF patients – and in the composite of stroke, systemic embolism, or all-cause mortality, which had an incidence of 6.46%/year in the recent-onset group, compared with 4.57%/year in remote-onset patients.
Turning to the impact of apixaban, Dr. Guimaraes noted that, as previously reported in the overall study, the primary endpoint of stroke or systemic embolism occurred in the apixaban group at a rate of 1.27%/year, compared with 1.6%/year with warfarin, for a 21% relative risk reduction in favor of the newer agent. She and her coinvestigators determined that in the remote-onset AF subgroup the relative risk reduction was 20%, while in the recent-onset subgroup the size of the effect was similar at 22%.
The composite safety endpoint of major or clinically relevant bleeding occurred in the remote-onset patients at a rate of 3.97%/year with apixaban versus 5.97%/year with warfarin, for a 33% relative risk reduction favoring the novel agent. In the recent-onset group, the rates were 5.04%/year with apixaban, compared with 6.4%/year with warfarin, for a 22% relative risk reduction.
Dr. Guimaraes observed an important limitation of this post hoc analysis is that the remote-onset AF group may have been selected for improved survival, since they didn’t die in the first 30 days after diagnosis.
Session co-chair Dr. Brian Olshansky commented that this analysis, which highlights the risks of recent-onset AF, argues for a strategy whereby a patient who presents to the ED with new-onset AF should get sent home on apixaban rather than being hospitalized for several days in order to be stabilized on warfarin.
“With recent-onset atrial fibrillation it’s going to take you several days to get anticoagulated with warfarin, whereas you’re immediately anticoagulated with apixaban,” said Dr. Olshansky, emeritus professor of internal medicine at the University of Iowa, Iowa City.
The ARISTOTLE trial was supported by Bristol-Myers Squibb and Pfizer. Dr. Guimaraes reported having no financial conflicts of interest.
AT ACC 16
Stroke risk rises quickly in recent-onset atrial fib
CHICAGO – The stroke risk in patients with recent-onset atrial fibrillation is similar to that of patients with longer-standing atrial fibrillation, according to a new secondary analysis of the landmark ARISTOTLE trial.
“Our key message is that patients with recent-onset atrial fibrillation had a similar risk of stroke but higher mortality than patients with remotely diagnosed atrial fibrillation, suggesting that patients with recently diagnosed atrial fibrillation are not at low risk and therefore warrant stroke prevention strategies,” Dr. Patricia O. Guimaraes said in presenting the findings at the annual meeting of the American College of Cardiology.
“Sometimes we as physicians hesitate in beginning oral anticoagulation therapy for patients that we just diagnosed. And of course patients are often afraid of anticoagulation therapy. But once they present with atrial fibrillation they are already at risk, and that’s why we need to anticoagulate them promptly,” added Dr. Guimaraes of the Duke Clinical Research Institute in Durham, N.C.
The benefits of apixaban (Eliquis) over warfarin seen in the overall randomized ARISTOTLE trial (N Engl J Med. 2011; 365:981-92) were preserved in the recent-onset subset of the atrial fibrillation (AF) study population, she noted.
The rationale for this new post hoc analysis of ARISTOTLE is that virtually all of the evidence supporting anticoagulation for stroke prevention in AF is based on studies conducted in patients with permanent, persistent, or long-standing paroxysmal AF. Much less is known about stroke risk and the benefits of anticoagulation in patients with recent-onset AF, Dr. Guimaraes explained.
The 1,899 ARISTOTLE participants with AF onset within 30 days prior to enrollment comprised 10.5% of the total study population, all of whom had AF and at least one other stroke risk factor. The recent-onset subgroup was the same age as the 16,241 subjects in this analysis who had longer-standing AF, but the recent-onset group included a higher proportion of women, had a lower prevalence of CAD, and their cardiovascular risk factor profile differed from that of the remote-onset AF group.
The composite endpoint of stroke, systemic embolism, major bleeding, or all-cause mortality occurred at a rate of 8.69%/year in the recent-onset AF group, compared with 6.43%/year in the remote-onset group. However, in a multivariate regression analysis adjusted for potential confounders, the only significant differences in outcome between the two groups were in all-cause mortality – 5.15%/year in the recent-onset group, 3.15% in the remote-onset AF patients – and in the composite of stroke, systemic embolism, or all-cause mortality, which had an incidence of 6.46%/year in the recent-onset group, compared with 4.57%/year in remote-onset patients.
Turning to the impact of apixaban, Dr. Guimaraes noted that, as previously reported in the overall study, the primary endpoint of stroke or systemic embolism occurred in the apixaban group at a rate of 1.27%/year, compared with 1.6%/year with warfarin, for a 21% relative risk reduction in favor of the newer agent. She and her coinvestigators determined that in the remote-onset AF subgroup the relative risk reduction was 20%, while in the recent-onset subgroup the size of the effect was similar at 22%.
The composite safety endpoint of major or clinically relevant bleeding occurred in the remote-onset patients at a rate of 3.97%/year with apixaban versus 5.97%/year with warfarin, for a 33% relative risk reduction favoring the novel agent. In the recent-onset group, the rates were 5.04%/year with apixaban, compared with 6.4%/year with warfarin, for a 22% relative risk reduction.
Dr. Guimaraes observed an important limitation of this post hoc analysis is that the remote-onset AF group may have been selected for improved survival, since they didn’t die in the first 30 days after diagnosis.
Session co-chair Dr. Brian Olshansky commented that this analysis, which highlights the risks of recent-onset AF, argues for a strategy whereby a patient who presents to the ED with new-onset AF should get sent home on apixaban rather than being hospitalized for several days in order to be stabilized on warfarin.
“With recent-onset atrial fibrillation it’s going to take you several days to get anticoagulated with warfarin, whereas you’re immediately anticoagulated with apixaban,” said Dr. Olshansky, emeritus professor of internal medicine at the University of Iowa, Iowa City.
The ARISTOTLE trial was supported by Bristol-Myers Squibb and Pfizer. Dr. Guimaraes reported having no financial conflicts of interest.
CHICAGO – The stroke risk in patients with recent-onset atrial fibrillation is similar to that of patients with longer-standing atrial fibrillation, according to a new secondary analysis of the landmark ARISTOTLE trial.
“Our key message is that patients with recent-onset atrial fibrillation had a similar risk of stroke but higher mortality than patients with remotely diagnosed atrial fibrillation, suggesting that patients with recently diagnosed atrial fibrillation are not at low risk and therefore warrant stroke prevention strategies,” Dr. Patricia O. Guimaraes said in presenting the findings at the annual meeting of the American College of Cardiology.
“Sometimes we as physicians hesitate in beginning oral anticoagulation therapy for patients that we just diagnosed. And of course patients are often afraid of anticoagulation therapy. But once they present with atrial fibrillation they are already at risk, and that’s why we need to anticoagulate them promptly,” added Dr. Guimaraes of the Duke Clinical Research Institute in Durham, N.C.
The benefits of apixaban (Eliquis) over warfarin seen in the overall randomized ARISTOTLE trial (N Engl J Med. 2011; 365:981-92) were preserved in the recent-onset subset of the atrial fibrillation (AF) study population, she noted.
The rationale for this new post hoc analysis of ARISTOTLE is that virtually all of the evidence supporting anticoagulation for stroke prevention in AF is based on studies conducted in patients with permanent, persistent, or long-standing paroxysmal AF. Much less is known about stroke risk and the benefits of anticoagulation in patients with recent-onset AF, Dr. Guimaraes explained.
The 1,899 ARISTOTLE participants with AF onset within 30 days prior to enrollment comprised 10.5% of the total study population, all of whom had AF and at least one other stroke risk factor. The recent-onset subgroup was the same age as the 16,241 subjects in this analysis who had longer-standing AF, but the recent-onset group included a higher proportion of women, had a lower prevalence of CAD, and their cardiovascular risk factor profile differed from that of the remote-onset AF group.
The composite endpoint of stroke, systemic embolism, major bleeding, or all-cause mortality occurred at a rate of 8.69%/year in the recent-onset AF group, compared with 6.43%/year in the remote-onset group. However, in a multivariate regression analysis adjusted for potential confounders, the only significant differences in outcome between the two groups were in all-cause mortality – 5.15%/year in the recent-onset group, 3.15% in the remote-onset AF patients – and in the composite of stroke, systemic embolism, or all-cause mortality, which had an incidence of 6.46%/year in the recent-onset group, compared with 4.57%/year in remote-onset patients.
Turning to the impact of apixaban, Dr. Guimaraes noted that, as previously reported in the overall study, the primary endpoint of stroke or systemic embolism occurred in the apixaban group at a rate of 1.27%/year, compared with 1.6%/year with warfarin, for a 21% relative risk reduction in favor of the newer agent. She and her coinvestigators determined that in the remote-onset AF subgroup the relative risk reduction was 20%, while in the recent-onset subgroup the size of the effect was similar at 22%.
The composite safety endpoint of major or clinically relevant bleeding occurred in the remote-onset patients at a rate of 3.97%/year with apixaban versus 5.97%/year with warfarin, for a 33% relative risk reduction favoring the novel agent. In the recent-onset group, the rates were 5.04%/year with apixaban, compared with 6.4%/year with warfarin, for a 22% relative risk reduction.
Dr. Guimaraes observed an important limitation of this post hoc analysis is that the remote-onset AF group may have been selected for improved survival, since they didn’t die in the first 30 days after diagnosis.
Session co-chair Dr. Brian Olshansky commented that this analysis, which highlights the risks of recent-onset AF, argues for a strategy whereby a patient who presents to the ED with new-onset AF should get sent home on apixaban rather than being hospitalized for several days in order to be stabilized on warfarin.
“With recent-onset atrial fibrillation it’s going to take you several days to get anticoagulated with warfarin, whereas you’re immediately anticoagulated with apixaban,” said Dr. Olshansky, emeritus professor of internal medicine at the University of Iowa, Iowa City.
The ARISTOTLE trial was supported by Bristol-Myers Squibb and Pfizer. Dr. Guimaraes reported having no financial conflicts of interest.
CHICAGO – The stroke risk in patients with recent-onset atrial fibrillation is similar to that of patients with longer-standing atrial fibrillation, according to a new secondary analysis of the landmark ARISTOTLE trial.
“Our key message is that patients with recent-onset atrial fibrillation had a similar risk of stroke but higher mortality than patients with remotely diagnosed atrial fibrillation, suggesting that patients with recently diagnosed atrial fibrillation are not at low risk and therefore warrant stroke prevention strategies,” Dr. Patricia O. Guimaraes said in presenting the findings at the annual meeting of the American College of Cardiology.
“Sometimes we as physicians hesitate in beginning oral anticoagulation therapy for patients that we just diagnosed. And of course patients are often afraid of anticoagulation therapy. But once they present with atrial fibrillation they are already at risk, and that’s why we need to anticoagulate them promptly,” added Dr. Guimaraes of the Duke Clinical Research Institute in Durham, N.C.
The benefits of apixaban (Eliquis) over warfarin seen in the overall randomized ARISTOTLE trial (N Engl J Med. 2011; 365:981-92) were preserved in the recent-onset subset of the atrial fibrillation (AF) study population, she noted.
The rationale for this new post hoc analysis of ARISTOTLE is that virtually all of the evidence supporting anticoagulation for stroke prevention in AF is based on studies conducted in patients with permanent, persistent, or long-standing paroxysmal AF. Much less is known about stroke risk and the benefits of anticoagulation in patients with recent-onset AF, Dr. Guimaraes explained.
The 1,899 ARISTOTLE participants with AF onset within 30 days prior to enrollment comprised 10.5% of the total study population, all of whom had AF and at least one other stroke risk factor. The recent-onset subgroup was the same age as the 16,241 subjects in this analysis who had longer-standing AF, but the recent-onset group included a higher proportion of women, had a lower prevalence of CAD, and their cardiovascular risk factor profile differed from that of the remote-onset AF group.
The composite endpoint of stroke, systemic embolism, major bleeding, or all-cause mortality occurred at a rate of 8.69%/year in the recent-onset AF group, compared with 6.43%/year in the remote-onset group. However, in a multivariate regression analysis adjusted for potential confounders, the only significant differences in outcome between the two groups were in all-cause mortality – 5.15%/year in the recent-onset group, 3.15% in the remote-onset AF patients – and in the composite of stroke, systemic embolism, or all-cause mortality, which had an incidence of 6.46%/year in the recent-onset group, compared with 4.57%/year in remote-onset patients.
Turning to the impact of apixaban, Dr. Guimaraes noted that, as previously reported in the overall study, the primary endpoint of stroke or systemic embolism occurred in the apixaban group at a rate of 1.27%/year, compared with 1.6%/year with warfarin, for a 21% relative risk reduction in favor of the newer agent. She and her coinvestigators determined that in the remote-onset AF subgroup the relative risk reduction was 20%, while in the recent-onset subgroup the size of the effect was similar at 22%.
The composite safety endpoint of major or clinically relevant bleeding occurred in the remote-onset patients at a rate of 3.97%/year with apixaban versus 5.97%/year with warfarin, for a 33% relative risk reduction favoring the novel agent. In the recent-onset group, the rates were 5.04%/year with apixaban, compared with 6.4%/year with warfarin, for a 22% relative risk reduction.
Dr. Guimaraes observed an important limitation of this post hoc analysis is that the remote-onset AF group may have been selected for improved survival, since they didn’t die in the first 30 days after diagnosis.
Session co-chair Dr. Brian Olshansky commented that this analysis, which highlights the risks of recent-onset AF, argues for a strategy whereby a patient who presents to the ED with new-onset AF should get sent home on apixaban rather than being hospitalized for several days in order to be stabilized on warfarin.
“With recent-onset atrial fibrillation it’s going to take you several days to get anticoagulated with warfarin, whereas you’re immediately anticoagulated with apixaban,” said Dr. Olshansky, emeritus professor of internal medicine at the University of Iowa, Iowa City.
The ARISTOTLE trial was supported by Bristol-Myers Squibb and Pfizer. Dr. Guimaraes reported having no financial conflicts of interest.
Key clinical point: Don’t delay starting oral anticoagulation in patients with recent-onset atrial fibrillation.
Major finding: All-cause mortality occurred at a rate of 5.15%/year in patients started on apixaban or warfarin within 30 days following diagnosis of atrial fibrillation, compared with 3.15%/year in those with longer-duration atrial fibrillation.
Data source: This was a secondary post hoc analysis of 18,140 participants in the randomized, double-blind, prospective ARISTOTLE trial of apixaban versus warfarin for stroke prevention.
Disclosures: The study presenter reported having no financial conflicts of interest.
Rhythm control may be best for atrial fib in HFpEF
CHICAGO – Atrial fibrillation with good heart rate control in patients who have heart failure with preserved ejection fraction is independently associated with exercise intolerance, impaired contractile reserve, and a sharply higher mortality rate than in matched HFpEF patients without the arrhythmia, a retrospective analysis showed.
“Our study, the largest of its kind, provides mechanistic evidence from cardiopulmonary testing that a rhythm control strategy may potentially improve peak exercise capacity and survival in this patient population, a finding that of course requires future prospective appraisal in randomized trials comparing rate and rhythm control of atrial fibrillation in HFpEF,” Dr. Mohamed Badreldin Elshazly reported at the annual meeting of the American College of Cardiology.
In the meantime, his study also shows the useful role cardiopulmonary stress testing can play in the setting of atrial fibrillation (AF) in HFpEF, he added.
“Cardiopulmonary stress tests are cheap and easy to do. They’re a big asset for personalized medicine. Using an objective measure like cardiopulmonary stress testing to define the physiologic and hemodynamic consequences of atrial fibrillation in individual patients may help identify those in whom rhythm control may improve exercise tolerance and quality of life, and those who may be okay with rate control,” according to Dr. Elshazly of the Cleveland Clinic.
He noted that while it’s well established that atrial fibrillation is associated with exercise intolerance in patients with heart failure with reduced ejection fraction (HFrEF) and that restoration of sinus rhythm in such patients has a positive impact on exercise hemodynamics, symptom severity, and quality of life, the situation is murkier regarding AF in patients with HFpEF. Prior studies were generally small and unable to establish whether AF was independently associated with exercise intolerance or if HFpEF patients who developed AF were sicker and higher risk.
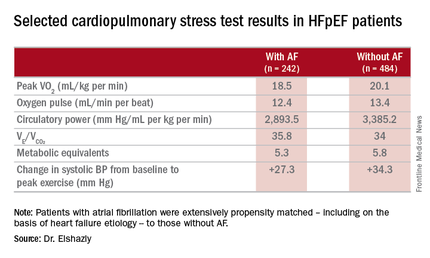
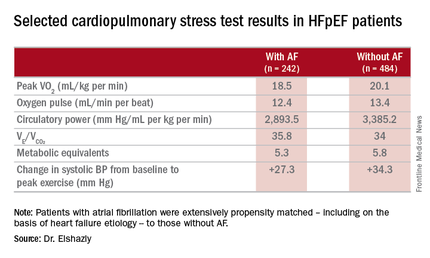
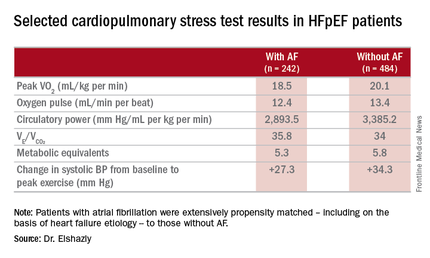
He presented a retrospective, case-control study in a cohort of 1,825 patients with HFpEF referred for maximal, symptom-limited cardiopulmonary stress testing at the Cleveland Clinic. Among these were 242 patients with AF. They were extensively propensity matched – including on the basis of heart failure etiology – to 484 HFpEF patients without AF.
“That’s what makes our study strong. We were the first to be able to do propensity matching and therefore account for other risk factors in our analysis,” Dr. Elshazly explained.
The investigators measured peak oxygen uptake (VO2), the minute ventilation–carbon dioxide production relationship (VE/VCO2) as an indicator of ventilatory efficiency, metabolic equivalents (METS), ventilatory anaerobic threshold, circulatory power as a proxy for cardiac power, peak oxygen pulse as a surrogate for stroke volume, and resting and peak heart rate and systolic blood pressure. The patients with AF were in fibrillation at the time of their cardiopulmonary stress testing.
The HFpEF patients with AF had a mean resting heart rate of 70 beats per minute and a peak rate of 130 bpm. This group showed evidence of impaired peak exercise tolerance as reflected in lower peak VO2, oxygen pulse, and circulatory power at peak exercise. Their VE/VCO2 was higher, indicating impaired ventilatory efficiency. Notably, however, their submaximal exercise capacity was similar to the non-AF controls.
“Atrial fibrillation in these patients is really more of a disease that shows itself in patients when you take them to their peak exercise capacity,” he observed.
All-cause mortality was significantly higher in the AF as compared with no-AF patients with HFpEF. The mortality curves separated early and the divergence grew larger over the course of 8 years of follow-up.
One audience member pointed out that the large mortality difference between the two groups seems disproportionate to the rather modest differences in exercise capacity.
“It brings up an interesting point,” Dr. Elshazly replied. “Maybe the increase in total mortality that we see is being driven by other things besides cardiovascular mortality. Our data doesn’t capture the specific cause of death, be it cancer, for example, but it does raise the idea that this mortality difference is not all driven by cardiovascular mortality, but by atrial fibrillation.”
Dr. Elshazly reported having no financial conflicts of interest regarding his institutionally supported study.
CHICAGO – Atrial fibrillation with good heart rate control in patients who have heart failure with preserved ejection fraction is independently associated with exercise intolerance, impaired contractile reserve, and a sharply higher mortality rate than in matched HFpEF patients without the arrhythmia, a retrospective analysis showed.
“Our study, the largest of its kind, provides mechanistic evidence from cardiopulmonary testing that a rhythm control strategy may potentially improve peak exercise capacity and survival in this patient population, a finding that of course requires future prospective appraisal in randomized trials comparing rate and rhythm control of atrial fibrillation in HFpEF,” Dr. Mohamed Badreldin Elshazly reported at the annual meeting of the American College of Cardiology.
In the meantime, his study also shows the useful role cardiopulmonary stress testing can play in the setting of atrial fibrillation (AF) in HFpEF, he added.
“Cardiopulmonary stress tests are cheap and easy to do. They’re a big asset for personalized medicine. Using an objective measure like cardiopulmonary stress testing to define the physiologic and hemodynamic consequences of atrial fibrillation in individual patients may help identify those in whom rhythm control may improve exercise tolerance and quality of life, and those who may be okay with rate control,” according to Dr. Elshazly of the Cleveland Clinic.
He noted that while it’s well established that atrial fibrillation is associated with exercise intolerance in patients with heart failure with reduced ejection fraction (HFrEF) and that restoration of sinus rhythm in such patients has a positive impact on exercise hemodynamics, symptom severity, and quality of life, the situation is murkier regarding AF in patients with HFpEF. Prior studies were generally small and unable to establish whether AF was independently associated with exercise intolerance or if HFpEF patients who developed AF were sicker and higher risk.
He presented a retrospective, case-control study in a cohort of 1,825 patients with HFpEF referred for maximal, symptom-limited cardiopulmonary stress testing at the Cleveland Clinic. Among these were 242 patients with AF. They were extensively propensity matched – including on the basis of heart failure etiology – to 484 HFpEF patients without AF.
“That’s what makes our study strong. We were the first to be able to do propensity matching and therefore account for other risk factors in our analysis,” Dr. Elshazly explained.
The investigators measured peak oxygen uptake (VO2), the minute ventilation–carbon dioxide production relationship (VE/VCO2) as an indicator of ventilatory efficiency, metabolic equivalents (METS), ventilatory anaerobic threshold, circulatory power as a proxy for cardiac power, peak oxygen pulse as a surrogate for stroke volume, and resting and peak heart rate and systolic blood pressure. The patients with AF were in fibrillation at the time of their cardiopulmonary stress testing.
The HFpEF patients with AF had a mean resting heart rate of 70 beats per minute and a peak rate of 130 bpm. This group showed evidence of impaired peak exercise tolerance as reflected in lower peak VO2, oxygen pulse, and circulatory power at peak exercise. Their VE/VCO2 was higher, indicating impaired ventilatory efficiency. Notably, however, their submaximal exercise capacity was similar to the non-AF controls.
“Atrial fibrillation in these patients is really more of a disease that shows itself in patients when you take them to their peak exercise capacity,” he observed.
All-cause mortality was significantly higher in the AF as compared with no-AF patients with HFpEF. The mortality curves separated early and the divergence grew larger over the course of 8 years of follow-up.
One audience member pointed out that the large mortality difference between the two groups seems disproportionate to the rather modest differences in exercise capacity.
“It brings up an interesting point,” Dr. Elshazly replied. “Maybe the increase in total mortality that we see is being driven by other things besides cardiovascular mortality. Our data doesn’t capture the specific cause of death, be it cancer, for example, but it does raise the idea that this mortality difference is not all driven by cardiovascular mortality, but by atrial fibrillation.”
Dr. Elshazly reported having no financial conflicts of interest regarding his institutionally supported study.
CHICAGO – Atrial fibrillation with good heart rate control in patients who have heart failure with preserved ejection fraction is independently associated with exercise intolerance, impaired contractile reserve, and a sharply higher mortality rate than in matched HFpEF patients without the arrhythmia, a retrospective analysis showed.
“Our study, the largest of its kind, provides mechanistic evidence from cardiopulmonary testing that a rhythm control strategy may potentially improve peak exercise capacity and survival in this patient population, a finding that of course requires future prospective appraisal in randomized trials comparing rate and rhythm control of atrial fibrillation in HFpEF,” Dr. Mohamed Badreldin Elshazly reported at the annual meeting of the American College of Cardiology.
In the meantime, his study also shows the useful role cardiopulmonary stress testing can play in the setting of atrial fibrillation (AF) in HFpEF, he added.
“Cardiopulmonary stress tests are cheap and easy to do. They’re a big asset for personalized medicine. Using an objective measure like cardiopulmonary stress testing to define the physiologic and hemodynamic consequences of atrial fibrillation in individual patients may help identify those in whom rhythm control may improve exercise tolerance and quality of life, and those who may be okay with rate control,” according to Dr. Elshazly of the Cleveland Clinic.
He noted that while it’s well established that atrial fibrillation is associated with exercise intolerance in patients with heart failure with reduced ejection fraction (HFrEF) and that restoration of sinus rhythm in such patients has a positive impact on exercise hemodynamics, symptom severity, and quality of life, the situation is murkier regarding AF in patients with HFpEF. Prior studies were generally small and unable to establish whether AF was independently associated with exercise intolerance or if HFpEF patients who developed AF were sicker and higher risk.
He presented a retrospective, case-control study in a cohort of 1,825 patients with HFpEF referred for maximal, symptom-limited cardiopulmonary stress testing at the Cleveland Clinic. Among these were 242 patients with AF. They were extensively propensity matched – including on the basis of heart failure etiology – to 484 HFpEF patients without AF.
“That’s what makes our study strong. We were the first to be able to do propensity matching and therefore account for other risk factors in our analysis,” Dr. Elshazly explained.
The investigators measured peak oxygen uptake (VO2), the minute ventilation–carbon dioxide production relationship (VE/VCO2) as an indicator of ventilatory efficiency, metabolic equivalents (METS), ventilatory anaerobic threshold, circulatory power as a proxy for cardiac power, peak oxygen pulse as a surrogate for stroke volume, and resting and peak heart rate and systolic blood pressure. The patients with AF were in fibrillation at the time of their cardiopulmonary stress testing.
The HFpEF patients with AF had a mean resting heart rate of 70 beats per minute and a peak rate of 130 bpm. This group showed evidence of impaired peak exercise tolerance as reflected in lower peak VO2, oxygen pulse, and circulatory power at peak exercise. Their VE/VCO2 was higher, indicating impaired ventilatory efficiency. Notably, however, their submaximal exercise capacity was similar to the non-AF controls.
“Atrial fibrillation in these patients is really more of a disease that shows itself in patients when you take them to their peak exercise capacity,” he observed.
All-cause mortality was significantly higher in the AF as compared with no-AF patients with HFpEF. The mortality curves separated early and the divergence grew larger over the course of 8 years of follow-up.
One audience member pointed out that the large mortality difference between the two groups seems disproportionate to the rather modest differences in exercise capacity.
“It brings up an interesting point,” Dr. Elshazly replied. “Maybe the increase in total mortality that we see is being driven by other things besides cardiovascular mortality. Our data doesn’t capture the specific cause of death, be it cancer, for example, but it does raise the idea that this mortality difference is not all driven by cardiovascular mortality, but by atrial fibrillation.”
Dr. Elshazly reported having no financial conflicts of interest regarding his institutionally supported study.
AT ACC 16
Key clinical point: Atrial fibrillation in patients with heart failure with preserved ejection fraction is associated with exercise intolerance and increased mortality.
Major finding: Mean peak VO2 was 18.5 mL/kg per minute in patients with HFpEF and atrial fibrillation, significantly less than the 20.1 mL/kg per minute in controls.
Data source: A retrospective, single-institution study of cardiopulmonary stress test findings and 8-year mortality in 242 patients with HFpEF and atrial fibrillation and 484 propensity-matched controls with HFpEF and no arrhythmia.
Disclosures: The presenter reported having no financial conflicts of interest regarding his institutionally supported study.
Prompt antidepressant treatment swiftly chops cardiovascular risk
CHICAGO – Prompt, effective treatment for depression in the primary care setting appears to swiftly reduce the elevated cardiovascular risk known to be tied to the mood disorder, Heidi Thomas May, Ph.D., reported at the annual meeting of the American College of Cardiology.
“We know that depression is a risk factor for long-term adverse cardiovascular outcomes. Our study shows that it can also have immediate effects on someone’s cardiovascular health. I think our study highlights the importance of screening for depression in the primary care setting – and if someone’s depressed, they need to be treated,” said Dr. May, a cardiovascular and genetic epidemiologist at Intermountain Medical Center in Murray, Utah.
She presented an observational study of the electronic medical records of 7,559 Intermountain Healthcare patients over age 40 years who completed the Patient Health Questionnaire-9 (PHQ-9) depression screening tool during a visit to an Intermountain primary care clinic for any reason. They completed another PHQ-9 a median of 2.7 years later. Under the Intermountain system, a PHQ-9 score of 10 or more triggers implementation of a depression treatment pathway, the specifics of which vary depending upon the severity of symptoms.
On the basis of their two PHQ-9 scores, all patients were classified into one of four groups: The “nondepressed” group of 3,286 patients had a score of 9 or less on both occasions; the “remained depressed” cohort of 1,987 patients scored 10 or more on both PHQ-9s; the “no longer depressed” group of 1,542 patients scored at least 10 but subsequently improved by at least 5 points to a score of 9 or less; and the 735 patients in the “became depressed” group first scored 9 or less on the PHQ-9 but subsequently had at least a 5-point increase to a score of 10 or more.
The subjects were then followed for major adverse cardiovascular events, or MACE – defined as a composite of death, diagnosis of coronary artery disease, acute MI, stroke, and heart failure hospitalization – for a median of 208 days after completing their second PHQ-9.
The MACE rate was 4.8% in the nondepressed group and similar at 4.6% in the “no longer depressed” group, Dr. May reported. Both groups fared significantly better than the “remained depressed” and “became depressed” groups, which had MACE rates of 6% and 6.4%, respectively.
In a multivariate regression analysis adjusted for demographics, cardiovascular risk factors, prior disease diagnoses, medications, and other potential confounders, the “remained depressed” group was 33% more likely to experience a cardiovascular event than was the nondepressed group, she said. The “became depressed” group had a 44% increase in risk, compared with the nondepressed individuals. In contrast, the MACE risk in patients in the “no longer depressed” group was not significantly different from that of patients who weren’t depressed at either time point. And the MACE risk of patients who became depressed during the course of the study was no different from that of patients who remained depressed at both time points.
This is the first study of its kind, Dr. May said. Hence, the results require confirmation, ideally in a randomized clinical trial.
She reported having no financial conflicts regarding the study, which was supported by Intermountain Healthcare.
CHICAGO – Prompt, effective treatment for depression in the primary care setting appears to swiftly reduce the elevated cardiovascular risk known to be tied to the mood disorder, Heidi Thomas May, Ph.D., reported at the annual meeting of the American College of Cardiology.
“We know that depression is a risk factor for long-term adverse cardiovascular outcomes. Our study shows that it can also have immediate effects on someone’s cardiovascular health. I think our study highlights the importance of screening for depression in the primary care setting – and if someone’s depressed, they need to be treated,” said Dr. May, a cardiovascular and genetic epidemiologist at Intermountain Medical Center in Murray, Utah.
She presented an observational study of the electronic medical records of 7,559 Intermountain Healthcare patients over age 40 years who completed the Patient Health Questionnaire-9 (PHQ-9) depression screening tool during a visit to an Intermountain primary care clinic for any reason. They completed another PHQ-9 a median of 2.7 years later. Under the Intermountain system, a PHQ-9 score of 10 or more triggers implementation of a depression treatment pathway, the specifics of which vary depending upon the severity of symptoms.
On the basis of their two PHQ-9 scores, all patients were classified into one of four groups: The “nondepressed” group of 3,286 patients had a score of 9 or less on both occasions; the “remained depressed” cohort of 1,987 patients scored 10 or more on both PHQ-9s; the “no longer depressed” group of 1,542 patients scored at least 10 but subsequently improved by at least 5 points to a score of 9 or less; and the 735 patients in the “became depressed” group first scored 9 or less on the PHQ-9 but subsequently had at least a 5-point increase to a score of 10 or more.
The subjects were then followed for major adverse cardiovascular events, or MACE – defined as a composite of death, diagnosis of coronary artery disease, acute MI, stroke, and heart failure hospitalization – for a median of 208 days after completing their second PHQ-9.
The MACE rate was 4.8% in the nondepressed group and similar at 4.6% in the “no longer depressed” group, Dr. May reported. Both groups fared significantly better than the “remained depressed” and “became depressed” groups, which had MACE rates of 6% and 6.4%, respectively.
In a multivariate regression analysis adjusted for demographics, cardiovascular risk factors, prior disease diagnoses, medications, and other potential confounders, the “remained depressed” group was 33% more likely to experience a cardiovascular event than was the nondepressed group, she said. The “became depressed” group had a 44% increase in risk, compared with the nondepressed individuals. In contrast, the MACE risk in patients in the “no longer depressed” group was not significantly different from that of patients who weren’t depressed at either time point. And the MACE risk of patients who became depressed during the course of the study was no different from that of patients who remained depressed at both time points.
This is the first study of its kind, Dr. May said. Hence, the results require confirmation, ideally in a randomized clinical trial.
She reported having no financial conflicts regarding the study, which was supported by Intermountain Healthcare.
CHICAGO – Prompt, effective treatment for depression in the primary care setting appears to swiftly reduce the elevated cardiovascular risk known to be tied to the mood disorder, Heidi Thomas May, Ph.D., reported at the annual meeting of the American College of Cardiology.
“We know that depression is a risk factor for long-term adverse cardiovascular outcomes. Our study shows that it can also have immediate effects on someone’s cardiovascular health. I think our study highlights the importance of screening for depression in the primary care setting – and if someone’s depressed, they need to be treated,” said Dr. May, a cardiovascular and genetic epidemiologist at Intermountain Medical Center in Murray, Utah.
She presented an observational study of the electronic medical records of 7,559 Intermountain Healthcare patients over age 40 years who completed the Patient Health Questionnaire-9 (PHQ-9) depression screening tool during a visit to an Intermountain primary care clinic for any reason. They completed another PHQ-9 a median of 2.7 years later. Under the Intermountain system, a PHQ-9 score of 10 or more triggers implementation of a depression treatment pathway, the specifics of which vary depending upon the severity of symptoms.
On the basis of their two PHQ-9 scores, all patients were classified into one of four groups: The “nondepressed” group of 3,286 patients had a score of 9 or less on both occasions; the “remained depressed” cohort of 1,987 patients scored 10 or more on both PHQ-9s; the “no longer depressed” group of 1,542 patients scored at least 10 but subsequently improved by at least 5 points to a score of 9 or less; and the 735 patients in the “became depressed” group first scored 9 or less on the PHQ-9 but subsequently had at least a 5-point increase to a score of 10 or more.
The subjects were then followed for major adverse cardiovascular events, or MACE – defined as a composite of death, diagnosis of coronary artery disease, acute MI, stroke, and heart failure hospitalization – for a median of 208 days after completing their second PHQ-9.
The MACE rate was 4.8% in the nondepressed group and similar at 4.6% in the “no longer depressed” group, Dr. May reported. Both groups fared significantly better than the “remained depressed” and “became depressed” groups, which had MACE rates of 6% and 6.4%, respectively.
In a multivariate regression analysis adjusted for demographics, cardiovascular risk factors, prior disease diagnoses, medications, and other potential confounders, the “remained depressed” group was 33% more likely to experience a cardiovascular event than was the nondepressed group, she said. The “became depressed” group had a 44% increase in risk, compared with the nondepressed individuals. In contrast, the MACE risk in patients in the “no longer depressed” group was not significantly different from that of patients who weren’t depressed at either time point. And the MACE risk of patients who became depressed during the course of the study was no different from that of patients who remained depressed at both time points.
This is the first study of its kind, Dr. May said. Hence, the results require confirmation, ideally in a randomized clinical trial.
She reported having no financial conflicts regarding the study, which was supported by Intermountain Healthcare.
AT ACC 16
Key clinical point: Event rate was no different in “no longer depressed” group than in “never depressed.”
Major finding: Major adverse cardiovascular events were 44% more likely in primary care patients who became depressed during a median 2.7-year period, compared with those who weren’t depressed at either time point.
Data source: An observational study of 7,550 patients screened for depression in primary care clinics.
Disclosures: The study was supported by Intermountain Healthcare. Dr. May reported having no financial conflicts of interest.
Exercise Is Protective but Underutilized in Atrial Fib Patients
CHICAGO – Efforts to encourage even modest amounts of physical activity in sedentary patients with atrial fibrillation are likely to pay off in reduced risks of cardiovascular and all-cause mortality, according to a report from the EurObservational Research Program Pilot Survey on Atrial Fibrillation General Registry.
“Clearly we would recommend regular physical activity for patients with atrial fibrillation on the basis of the mortality benefit we see in the registry. If we give patients with atrial fibrillation oral anticoagulation, they are protected against stroke risk, but clearly they are still dying a lot,” Dr. Marco Proietti said at the annual meeting of the American College of Cardiology.
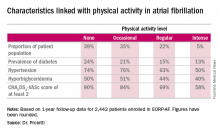
He presented 1-year follow-up data on 2,442 “real world” patients enrolled in the nine-country, observational, prospective registry, known as EORP-AF, shortly after being diagnosed with AF. One of the goals of EORP-AF is to learn whether physical exercise protects against cardiovascular events and all-cause mortality in AF patients, as has been well established in the general population and in patients at high cardiovascular risk.
One striking finding was that nearly 40% of patients in EORP-AF reported engaging in no physical activity, defined for study purposes as zero to less than 3 hours of physical activity per week for less than 2 years.
The other three categories employed by investigators were “occasional,” meaning less than 3 hours per week but for 2 years or more; “regular,” defined as at least 3 hours weekly for at least 2 years; and “intense,” which required more than 7 hours of physical activity per week for at least 2 years. Levels of cardiovascular and stroke risk factors decreased progressively with increasing levels of physical activity. Only 5% of the AF patients met the ‘intense’ standard, noted Dr. Proietti of the University of Birmingham (England).
The 1-year cardiovascular mortality rate approached 6% in the no physical activity group and hovered around 1% in the other three groups. The 1-year all-cause mortality rate exceeded 12% in the no-exercise group, was 4%% in the occasional exercisers, and 1%-2% in the groups reporting regular or intense physical activity.
The 1-year composite endpoint of cardiovascular death, any thromboembolism, or a bleeding event occurred in 12% of the sedentary patients, a rate two-to-three times higher than in the others.
Updated outcomes are to be reported from the EORP-AF pilot registry after 2 and 3 years of follow-up. Meanwhile, on the basis of the success of the pilot registry, more than 10,000 patients with AF have been enrolled in the EORP-AF main registry, according to Dr. Proietti.
A study limitation, he conceded, is that the registry includes no objective measure of physical capacity, such as METS.
Session co-chair Dr. Brian Olshansky, emeritus professor of internal medicine at the University of Iowa, Iowa City, observed that the registry data raise a classic chicken-versus-egg issue: Do the sedentary patients do worse because they’re inactive, or are they inactive because they are sicker and hence have worse outcomes?
Dr. Proietti said the registry data provide some support for the latter idea, since the no-physical-activity group had higher prevalences of coronary artery disease and heart failure.
Dr. Olshansky raised another point: “It’s interesting to me that there’s a whole bunch of literature showing that elite endurance athletes – bike racers, cross country skiers – have a very high incidence of atrial fibrillation. It seems to be either an inflammatory or an autonomic issue.”
Dr. Proietti replied that he’s familiar with that extensive literature, but the EORP-AF data through 1 year don’t provide validation. While the intense physical activity group tended to have more symptomatic AF than the other groups, they were no more likely to show progression from paroxysmal to permanent AF. The much larger main registry now underway may be able to better clarify the relationship between physical activity and incidence and progression of AF, including the possibility of a U-shaped dose-response curve.
The EORP-AF registry is supported by the European Society of Cardiology. Dr. Proietti reported having no financial conflicts of interest.
CHICAGO – Efforts to encourage even modest amounts of physical activity in sedentary patients with atrial fibrillation are likely to pay off in reduced risks of cardiovascular and all-cause mortality, according to a report from the EurObservational Research Program Pilot Survey on Atrial Fibrillation General Registry.
“Clearly we would recommend regular physical activity for patients with atrial fibrillation on the basis of the mortality benefit we see in the registry. If we give patients with atrial fibrillation oral anticoagulation, they are protected against stroke risk, but clearly they are still dying a lot,” Dr. Marco Proietti said at the annual meeting of the American College of Cardiology.
He presented 1-year follow-up data on 2,442 “real world” patients enrolled in the nine-country, observational, prospective registry, known as EORP-AF, shortly after being diagnosed with AF. One of the goals of EORP-AF is to learn whether physical exercise protects against cardiovascular events and all-cause mortality in AF patients, as has been well established in the general population and in patients at high cardiovascular risk.
One striking finding was that nearly 40% of patients in EORP-AF reported engaging in no physical activity, defined for study purposes as zero to less than 3 hours of physical activity per week for less than 2 years.
The other three categories employed by investigators were “occasional,” meaning less than 3 hours per week but for 2 years or more; “regular,” defined as at least 3 hours weekly for at least 2 years; and “intense,” which required more than 7 hours of physical activity per week for at least 2 years. Levels of cardiovascular and stroke risk factors decreased progressively with increasing levels of physical activity. Only 5% of the AF patients met the ‘intense’ standard, noted Dr. Proietti of the University of Birmingham (England).
The 1-year cardiovascular mortality rate approached 6% in the no physical activity group and hovered around 1% in the other three groups. The 1-year all-cause mortality rate exceeded 12% in the no-exercise group, was 4%% in the occasional exercisers, and 1%-2% in the groups reporting regular or intense physical activity.
The 1-year composite endpoint of cardiovascular death, any thromboembolism, or a bleeding event occurred in 12% of the sedentary patients, a rate two-to-three times higher than in the others.
Updated outcomes are to be reported from the EORP-AF pilot registry after 2 and 3 years of follow-up. Meanwhile, on the basis of the success of the pilot registry, more than 10,000 patients with AF have been enrolled in the EORP-AF main registry, according to Dr. Proietti.
A study limitation, he conceded, is that the registry includes no objective measure of physical capacity, such as METS.
Session co-chair Dr. Brian Olshansky, emeritus professor of internal medicine at the University of Iowa, Iowa City, observed that the registry data raise a classic chicken-versus-egg issue: Do the sedentary patients do worse because they’re inactive, or are they inactive because they are sicker and hence have worse outcomes?
Dr. Proietti said the registry data provide some support for the latter idea, since the no-physical-activity group had higher prevalences of coronary artery disease and heart failure.
Dr. Olshansky raised another point: “It’s interesting to me that there’s a whole bunch of literature showing that elite endurance athletes – bike racers, cross country skiers – have a very high incidence of atrial fibrillation. It seems to be either an inflammatory or an autonomic issue.”
Dr. Proietti replied that he’s familiar with that extensive literature, but the EORP-AF data through 1 year don’t provide validation. While the intense physical activity group tended to have more symptomatic AF than the other groups, they were no more likely to show progression from paroxysmal to permanent AF. The much larger main registry now underway may be able to better clarify the relationship between physical activity and incidence and progression of AF, including the possibility of a U-shaped dose-response curve.
The EORP-AF registry is supported by the European Society of Cardiology. Dr. Proietti reported having no financial conflicts of interest.
CHICAGO – Efforts to encourage even modest amounts of physical activity in sedentary patients with atrial fibrillation are likely to pay off in reduced risks of cardiovascular and all-cause mortality, according to a report from the EurObservational Research Program Pilot Survey on Atrial Fibrillation General Registry.
“Clearly we would recommend regular physical activity for patients with atrial fibrillation on the basis of the mortality benefit we see in the registry. If we give patients with atrial fibrillation oral anticoagulation, they are protected against stroke risk, but clearly they are still dying a lot,” Dr. Marco Proietti said at the annual meeting of the American College of Cardiology.
He presented 1-year follow-up data on 2,442 “real world” patients enrolled in the nine-country, observational, prospective registry, known as EORP-AF, shortly after being diagnosed with AF. One of the goals of EORP-AF is to learn whether physical exercise protects against cardiovascular events and all-cause mortality in AF patients, as has been well established in the general population and in patients at high cardiovascular risk.
One striking finding was that nearly 40% of patients in EORP-AF reported engaging in no physical activity, defined for study purposes as zero to less than 3 hours of physical activity per week for less than 2 years.
The other three categories employed by investigators were “occasional,” meaning less than 3 hours per week but for 2 years or more; “regular,” defined as at least 3 hours weekly for at least 2 years; and “intense,” which required more than 7 hours of physical activity per week for at least 2 years. Levels of cardiovascular and stroke risk factors decreased progressively with increasing levels of physical activity. Only 5% of the AF patients met the ‘intense’ standard, noted Dr. Proietti of the University of Birmingham (England).
The 1-year cardiovascular mortality rate approached 6% in the no physical activity group and hovered around 1% in the other three groups. The 1-year all-cause mortality rate exceeded 12% in the no-exercise group, was 4%% in the occasional exercisers, and 1%-2% in the groups reporting regular or intense physical activity.
The 1-year composite endpoint of cardiovascular death, any thromboembolism, or a bleeding event occurred in 12% of the sedentary patients, a rate two-to-three times higher than in the others.
Updated outcomes are to be reported from the EORP-AF pilot registry after 2 and 3 years of follow-up. Meanwhile, on the basis of the success of the pilot registry, more than 10,000 patients with AF have been enrolled in the EORP-AF main registry, according to Dr. Proietti.
A study limitation, he conceded, is that the registry includes no objective measure of physical capacity, such as METS.
Session co-chair Dr. Brian Olshansky, emeritus professor of internal medicine at the University of Iowa, Iowa City, observed that the registry data raise a classic chicken-versus-egg issue: Do the sedentary patients do worse because they’re inactive, or are they inactive because they are sicker and hence have worse outcomes?
Dr. Proietti said the registry data provide some support for the latter idea, since the no-physical-activity group had higher prevalences of coronary artery disease and heart failure.
Dr. Olshansky raised another point: “It’s interesting to me that there’s a whole bunch of literature showing that elite endurance athletes – bike racers, cross country skiers – have a very high incidence of atrial fibrillation. It seems to be either an inflammatory or an autonomic issue.”
Dr. Proietti replied that he’s familiar with that extensive literature, but the EORP-AF data through 1 year don’t provide validation. While the intense physical activity group tended to have more symptomatic AF than the other groups, they were no more likely to show progression from paroxysmal to permanent AF. The much larger main registry now underway may be able to better clarify the relationship between physical activity and incidence and progression of AF, including the possibility of a U-shaped dose-response curve.
The EORP-AF registry is supported by the European Society of Cardiology. Dr. Proietti reported having no financial conflicts of interest.
AT ACC 16
Exercise is protective but underutilized in atrial fib patients
CHICAGO – Efforts to encourage even modest amounts of physical activity in sedentary patients with atrial fibrillation are likely to pay off in reduced risks of cardiovascular and all-cause mortality, according to a report from the EurObservational Research Program Pilot Survey on Atrial Fibrillation General Registry.
“Clearly we would recommend regular physical activity for patients with atrial fibrillation on the basis of the mortality benefit we see in the registry. If we give patients with atrial fibrillation oral anticoagulation, they are protected against stroke risk, but clearly they are still dying a lot,” Dr. Marco Proietti said at the annual meeting of the American College of Cardiology.
He presented 1-year follow-up data on 2,442 “real world” patients enrolled in the nine-country, observational, prospective registry, known as EORP-AF, shortly after being diagnosed with AF. One of the goals of EORP-AF is to learn whether physical exercise protects against cardiovascular events and all-cause mortality in AF patients, as has been well established in the general population and in patients at high cardiovascular risk.
One striking finding was that nearly 40% of patients in EORP-AF reported engaging in no physical activity, defined for study purposes as zero to less than 3 hours of physical activity per week for less than 2 years.
The other three categories employed by investigators were “occasional,” meaning less than 3 hours per week but for 2 years or more; “regular,” defined as at least 3 hours weekly for at least 2 years; and “intense,” which required more than 7 hours of physical activity per week for at least 2 years. Levels of cardiovascular and stroke risk factors decreased progressively with increasing levels of physical activity. Only 5% of the AF patients met the ‘intense’ standard, noted Dr. Proietti of the University of Birmingham (England).
The 1-year cardiovascular mortality rate approached 6% in the no physical activity group and hovered around 1% in the other three groups. The 1-year all-cause mortality rate exceeded 12% in the no-exercise group, was 4%% in the occasional exercisers, and 1%-2% in the groups reporting regular or intense physical activity.
The 1-year composite endpoint of cardiovascular death, any thromboembolism, or a bleeding event occurred in 12% of the sedentary patients, a rate two-to-three times higher than in the others.
Updated outcomes are to be reported from the EORP-AF pilot registry after 2 and 3 years of follow-up. Meanwhile, on the basis of the success of the pilot registry, more than 10,000 patients with AF have been enrolled in the EORP-AF main registry, according to Dr. Proietti.
A study limitation, he conceded, is that the registry includes no objective measure of physical capacity, such as METS.
Session co-chair Dr. Brian Olshansky, emeritus professor of internal medicine at the University of Iowa, Iowa City, observed that the registry data raise a classic chicken-versus-egg issue: Do the sedentary patients do worse because they’re inactive, or are they inactive because they are sicker and hence have worse outcomes?
Dr. Proietti said the registry data provide some support for the latter idea, since the no-physical-activity group had higher prevalences of coronary artery disease and heart failure.
Dr. Olshansky raised another point: “It’s interesting to me that there’s a whole bunch of literature showing that elite endurance athletes – bike racers, cross country skiers – have a very high incidence of atrial fibrillation. It seems to be either an inflammatory or an autonomic issue.”
Dr. Proietti replied that he’s familiar with that extensive literature, but the EORP-AF data through 1 year don’t provide validation. While the intense physical activity group tended to have more symptomatic AF than the other groups, they were no more likely to show progression from paroxysmal to permanent AF. The much larger main registry now underway may be able to better clarify the relationship between physical activity and incidence and progression of AF, including the possibility of a U-shaped dose-response curve.
The EORP-AF registry is supported by the European Society of Cardiology. Dr. Proietti reported having no financial conflicts of interest.
CHICAGO – Efforts to encourage even modest amounts of physical activity in sedentary patients with atrial fibrillation are likely to pay off in reduced risks of cardiovascular and all-cause mortality, according to a report from the EurObservational Research Program Pilot Survey on Atrial Fibrillation General Registry.
“Clearly we would recommend regular physical activity for patients with atrial fibrillation on the basis of the mortality benefit we see in the registry. If we give patients with atrial fibrillation oral anticoagulation, they are protected against stroke risk, but clearly they are still dying a lot,” Dr. Marco Proietti said at the annual meeting of the American College of Cardiology.
He presented 1-year follow-up data on 2,442 “real world” patients enrolled in the nine-country, observational, prospective registry, known as EORP-AF, shortly after being diagnosed with AF. One of the goals of EORP-AF is to learn whether physical exercise protects against cardiovascular events and all-cause mortality in AF patients, as has been well established in the general population and in patients at high cardiovascular risk.
One striking finding was that nearly 40% of patients in EORP-AF reported engaging in no physical activity, defined for study purposes as zero to less than 3 hours of physical activity per week for less than 2 years.
The other three categories employed by investigators were “occasional,” meaning less than 3 hours per week but for 2 years or more; “regular,” defined as at least 3 hours weekly for at least 2 years; and “intense,” which required more than 7 hours of physical activity per week for at least 2 years. Levels of cardiovascular and stroke risk factors decreased progressively with increasing levels of physical activity. Only 5% of the AF patients met the ‘intense’ standard, noted Dr. Proietti of the University of Birmingham (England).
The 1-year cardiovascular mortality rate approached 6% in the no physical activity group and hovered around 1% in the other three groups. The 1-year all-cause mortality rate exceeded 12% in the no-exercise group, was 4%% in the occasional exercisers, and 1%-2% in the groups reporting regular or intense physical activity.
The 1-year composite endpoint of cardiovascular death, any thromboembolism, or a bleeding event occurred in 12% of the sedentary patients, a rate two-to-three times higher than in the others.
Updated outcomes are to be reported from the EORP-AF pilot registry after 2 and 3 years of follow-up. Meanwhile, on the basis of the success of the pilot registry, more than 10,000 patients with AF have been enrolled in the EORP-AF main registry, according to Dr. Proietti.
A study limitation, he conceded, is that the registry includes no objective measure of physical capacity, such as METS.
Session co-chair Dr. Brian Olshansky, emeritus professor of internal medicine at the University of Iowa, Iowa City, observed that the registry data raise a classic chicken-versus-egg issue: Do the sedentary patients do worse because they’re inactive, or are they inactive because they are sicker and hence have worse outcomes?
Dr. Proietti said the registry data provide some support for the latter idea, since the no-physical-activity group had higher prevalences of coronary artery disease and heart failure.
Dr. Olshansky raised another point: “It’s interesting to me that there’s a whole bunch of literature showing that elite endurance athletes – bike racers, cross country skiers – have a very high incidence of atrial fibrillation. It seems to be either an inflammatory or an autonomic issue.”
Dr. Proietti replied that he’s familiar with that extensive literature, but the EORP-AF data through 1 year don’t provide validation. While the intense physical activity group tended to have more symptomatic AF than the other groups, they were no more likely to show progression from paroxysmal to permanent AF. The much larger main registry now underway may be able to better clarify the relationship between physical activity and incidence and progression of AF, including the possibility of a U-shaped dose-response curve.
The EORP-AF registry is supported by the European Society of Cardiology. Dr. Proietti reported having no financial conflicts of interest.
CHICAGO – Efforts to encourage even modest amounts of physical activity in sedentary patients with atrial fibrillation are likely to pay off in reduced risks of cardiovascular and all-cause mortality, according to a report from the EurObservational Research Program Pilot Survey on Atrial Fibrillation General Registry.
“Clearly we would recommend regular physical activity for patients with atrial fibrillation on the basis of the mortality benefit we see in the registry. If we give patients with atrial fibrillation oral anticoagulation, they are protected against stroke risk, but clearly they are still dying a lot,” Dr. Marco Proietti said at the annual meeting of the American College of Cardiology.
He presented 1-year follow-up data on 2,442 “real world” patients enrolled in the nine-country, observational, prospective registry, known as EORP-AF, shortly after being diagnosed with AF. One of the goals of EORP-AF is to learn whether physical exercise protects against cardiovascular events and all-cause mortality in AF patients, as has been well established in the general population and in patients at high cardiovascular risk.
One striking finding was that nearly 40% of patients in EORP-AF reported engaging in no physical activity, defined for study purposes as zero to less than 3 hours of physical activity per week for less than 2 years.
The other three categories employed by investigators were “occasional,” meaning less than 3 hours per week but for 2 years or more; “regular,” defined as at least 3 hours weekly for at least 2 years; and “intense,” which required more than 7 hours of physical activity per week for at least 2 years. Levels of cardiovascular and stroke risk factors decreased progressively with increasing levels of physical activity. Only 5% of the AF patients met the ‘intense’ standard, noted Dr. Proietti of the University of Birmingham (England).
The 1-year cardiovascular mortality rate approached 6% in the no physical activity group and hovered around 1% in the other three groups. The 1-year all-cause mortality rate exceeded 12% in the no-exercise group, was 4%% in the occasional exercisers, and 1%-2% in the groups reporting regular or intense physical activity.
The 1-year composite endpoint of cardiovascular death, any thromboembolism, or a bleeding event occurred in 12% of the sedentary patients, a rate two-to-three times higher than in the others.
Updated outcomes are to be reported from the EORP-AF pilot registry after 2 and 3 years of follow-up. Meanwhile, on the basis of the success of the pilot registry, more than 10,000 patients with AF have been enrolled in the EORP-AF main registry, according to Dr. Proietti.
A study limitation, he conceded, is that the registry includes no objective measure of physical capacity, such as METS.
Session co-chair Dr. Brian Olshansky, emeritus professor of internal medicine at the University of Iowa, Iowa City, observed that the registry data raise a classic chicken-versus-egg issue: Do the sedentary patients do worse because they’re inactive, or are they inactive because they are sicker and hence have worse outcomes?
Dr. Proietti said the registry data provide some support for the latter idea, since the no-physical-activity group had higher prevalences of coronary artery disease and heart failure.
Dr. Olshansky raised another point: “It’s interesting to me that there’s a whole bunch of literature showing that elite endurance athletes – bike racers, cross country skiers – have a very high incidence of atrial fibrillation. It seems to be either an inflammatory or an autonomic issue.”
Dr. Proietti replied that he’s familiar with that extensive literature, but the EORP-AF data through 1 year don’t provide validation. While the intense physical activity group tended to have more symptomatic AF than the other groups, they were no more likely to show progression from paroxysmal to permanent AF. The much larger main registry now underway may be able to better clarify the relationship between physical activity and incidence and progression of AF, including the possibility of a U-shaped dose-response curve.
The EORP-AF registry is supported by the European Society of Cardiology. Dr. Proietti reported having no financial conflicts of interest.
AT ACC 16
Key clinical point: Atrial fibrillation patients who report engaging in even occasional physical activity have a markedly lower risk of all-cause mortality than those who are sedentary.
Major finding: The 1-year composite outcome of cardiovascular death, any thromboembolism, or a bleeding event occurred in 12% in patients with atrial fibrillation who were sedentary, a rate two to three times greater than in those who engaged in various amounts of physical activity.
Data source: An analysis of 1-year outcomes in 2,442 patients with AF enrolled in the prospective, observational EORP-AF pilot registry.
Disclosures: The EORP-AF registry is supported by the European Society of Cardiology. The presenter reported having no financial conflicts of interest.
Which ECG criteria are best for screening adolescent athletes?
CHICAGO – Results of the first-ever large study of ECG-based criteria for use in sports preparticipation screening in adolescent athletes demonstrate that the so-called Refined criteria decisively outperform the European Society of Cardiology and Seattle criteria, Dr. Aneil Malhotra reported at the annual meeting of the American College of Cardiology.
All three sets of 12-lead ECG criteria maintained an overall 92% sensitivity for the detection of serious cardiac pathology. However, the Refined criteria provided a major boost in specificity – and a markedly lower false positive rate, according to Dr. Malhotra of St. George’s, University of London.
The Refined criteria performed particularly well in the black adolescent athletes. That’s important because of black athletes’ historically high false positive rates with other ECG criteria, which lead to the time and expense of further testing, needless anxiety for the athletes and their families, and susceptibility to erroneous disqualification, he added.
The ESC recommendations for ECG interpretation in athletes were published in 2010 (Eur Heart J. 2010 Jan;31[2]:243-59). Because of their high false positive rates and the fact that the ESC criteria were derived exclusively from white athletes, an international consensus panel subsequently issued the Seattle criteria, which were developed based upon data from both black and white athletes (Br J Sports Med. 2013 Feb;47[3]:122-4).
While the Seattle criteria performed better than the ESC criteria, many sports cardiologists felt there was further room for improvement in setting criteria that differentiate between physiologic ECG patterns and those indicative of serious cardiac disease. Thus, another international expert consensus panel came up with the Refined criteria. And while the Refined criteria clearly outperformed the ESC and Seattle criteria when applied to a large group of young adult athletes (Circulation. 2014 Apr 22;129[16]:1637-49), the fact is that all three sets of criteria were developed with data from adult athletes. None had been tested in adolescent athletes, even though they are vastly more numerous than were adult athletes in every country. It was the need to validate the applicability of the adult-based criteria in adolescent athletes that was the impetus for Dr. Malhotra’s retrospective study.
He and his coinvestigators applied all three sets of criteria to a unique data set: 10,156 elite adolescent soccer players in the English Football Association’s program for the development of soccer professionals. The cohort consisted of 9,262 white and 894 black players, making this the largest-ever study conducted in adolescent black athletes. The subjects averaged just over 16 years in age and trained on average for more than 12 hours per week.
The English Football Association’s preparticipation screening program included a full history and physical examination, a 12-lead ECG, and – most importantly – an echocardiogram for every athlete, which enabled investigators to validate the ECG findings. The cost of echocardiography in young English footballers is covered by Cardiac Risk in the Young, a charitable organization.
Application of the ESC criteria resulted in an abnormal ECG requiring further investigation in 12.9% of the white athletes. With the Seattle criteria, this rate dropped to 4.2%. With the Refined criteria, it fell further to 2.8%.
In black adolescent athletes, the abnormal ECG rate was 16.2% with the ESC criteria, 5.8% with the Seattle criteria, and 3.8% using the Refined criteria.
A total of 36 cases of cardiac conditions predisposing to sudden cardiac death were identified in the overall cohort. Thirty-three of the 36 affected athletes were correctly identified by all three sets of ECG criteria, including all 28 cases of Wolf-Parkinson-White syndrome and the three cases of hypertrophic cardiomyopathy.
Armed with the true positive rates, the investigators were able to determine that the false positive ECG rates were 12.6% in whites and 15.5% in blacks with the ESC criteria, 3.9% in whites and 5.3% in blacks with the Seattle criteria, and 2.5% in whites and 3.1% in blacks by the Refined criteria.
The positive predictive value of the 12-lead ECG was more than fourfold higher with the Refined as compared with the ESC criteria: 11% versus 2.5% with the ESC and 7.5% with the Seattle criteria, Dr. Malhotra continued.
He explained that the Refined criteria differ from the other two sets of criteria as follows: There are a series of normal ECG findings in the adolescent athletes that are unrelated to training, and that experts agree don’t warrant further evaluation, such as incomplete right bundle branch block or sinus bradycardia. And there are well established ECG abnormalities that necessitate further testing. The Refined criteria establish an evidence-based set of borderline ECG findings that are deemed normal in isolation: atrial enlargement, axis deviation, and complete bundle branch block. Only if two or more of these findings are present is the ECG deemed abnormal.
The Refined criteria have been adopted by the sports cardiologists who perform preparticipation screening for the English Football Association and other UK athletic organizations. But Dr. Malhotra and his coinvestigators also tested a further refinement of the Refined criteria in the adolescent soccer players and found it further improved the results. The refinement involved incorporation of one element of the Seattle criteria, which deems T wave inversion in the V1 and V2 leads as normal in all athletes.
When Dr. Malhotra and colleagues applied this additional refinement to the study cohort of more than 10,000 elite adolescent soccer players, they found the updated Refined criteria reduced the overall abnormal ECG rate from 2.9% to 2.1% while maintaining a specificity in excess of 96% for the detection of serious cardiac pathology. These updated Refined criteria will soon be routinely used in preparticipation screening for the Football Association’s youth development program, he added.
Session co-chair Dr. John A. Spertus was favorably impressed.
“This is really terrific work. Congratulations. I love studies that declare and define waste in effort and resources, and worry for patients, and can eliminate that,” said Dr. Spertus, professor of medicine and director of cardiovascular education and outcomes research at the Mid America Heart Institute and University of Missouri, Kansas City.
The American Academy of Pediatrics and other U.S. medical societies do not routinely recommend a preparticipation ECG at this time, but rather a preparticipation physical evaluation involving a targeted history and physical exam available at www.aap.org by searching “ppe-4 forms.”
This study was funded by Cardiac Risk in the Young and the English Football Association. Dr. Malhotra reported having no financial conflicts of interest.
CHICAGO – Results of the first-ever large study of ECG-based criteria for use in sports preparticipation screening in adolescent athletes demonstrate that the so-called Refined criteria decisively outperform the European Society of Cardiology and Seattle criteria, Dr. Aneil Malhotra reported at the annual meeting of the American College of Cardiology.
All three sets of 12-lead ECG criteria maintained an overall 92% sensitivity for the detection of serious cardiac pathology. However, the Refined criteria provided a major boost in specificity – and a markedly lower false positive rate, according to Dr. Malhotra of St. George’s, University of London.
The Refined criteria performed particularly well in the black adolescent athletes. That’s important because of black athletes’ historically high false positive rates with other ECG criteria, which lead to the time and expense of further testing, needless anxiety for the athletes and their families, and susceptibility to erroneous disqualification, he added.
The ESC recommendations for ECG interpretation in athletes were published in 2010 (Eur Heart J. 2010 Jan;31[2]:243-59). Because of their high false positive rates and the fact that the ESC criteria were derived exclusively from white athletes, an international consensus panel subsequently issued the Seattle criteria, which were developed based upon data from both black and white athletes (Br J Sports Med. 2013 Feb;47[3]:122-4).
While the Seattle criteria performed better than the ESC criteria, many sports cardiologists felt there was further room for improvement in setting criteria that differentiate between physiologic ECG patterns and those indicative of serious cardiac disease. Thus, another international expert consensus panel came up with the Refined criteria. And while the Refined criteria clearly outperformed the ESC and Seattle criteria when applied to a large group of young adult athletes (Circulation. 2014 Apr 22;129[16]:1637-49), the fact is that all three sets of criteria were developed with data from adult athletes. None had been tested in adolescent athletes, even though they are vastly more numerous than were adult athletes in every country. It was the need to validate the applicability of the adult-based criteria in adolescent athletes that was the impetus for Dr. Malhotra’s retrospective study.
He and his coinvestigators applied all three sets of criteria to a unique data set: 10,156 elite adolescent soccer players in the English Football Association’s program for the development of soccer professionals. The cohort consisted of 9,262 white and 894 black players, making this the largest-ever study conducted in adolescent black athletes. The subjects averaged just over 16 years in age and trained on average for more than 12 hours per week.
The English Football Association’s preparticipation screening program included a full history and physical examination, a 12-lead ECG, and – most importantly – an echocardiogram for every athlete, which enabled investigators to validate the ECG findings. The cost of echocardiography in young English footballers is covered by Cardiac Risk in the Young, a charitable organization.
Application of the ESC criteria resulted in an abnormal ECG requiring further investigation in 12.9% of the white athletes. With the Seattle criteria, this rate dropped to 4.2%. With the Refined criteria, it fell further to 2.8%.
In black adolescent athletes, the abnormal ECG rate was 16.2% with the ESC criteria, 5.8% with the Seattle criteria, and 3.8% using the Refined criteria.
A total of 36 cases of cardiac conditions predisposing to sudden cardiac death were identified in the overall cohort. Thirty-three of the 36 affected athletes were correctly identified by all three sets of ECG criteria, including all 28 cases of Wolf-Parkinson-White syndrome and the three cases of hypertrophic cardiomyopathy.
Armed with the true positive rates, the investigators were able to determine that the false positive ECG rates were 12.6% in whites and 15.5% in blacks with the ESC criteria, 3.9% in whites and 5.3% in blacks with the Seattle criteria, and 2.5% in whites and 3.1% in blacks by the Refined criteria.
The positive predictive value of the 12-lead ECG was more than fourfold higher with the Refined as compared with the ESC criteria: 11% versus 2.5% with the ESC and 7.5% with the Seattle criteria, Dr. Malhotra continued.
He explained that the Refined criteria differ from the other two sets of criteria as follows: There are a series of normal ECG findings in the adolescent athletes that are unrelated to training, and that experts agree don’t warrant further evaluation, such as incomplete right bundle branch block or sinus bradycardia. And there are well established ECG abnormalities that necessitate further testing. The Refined criteria establish an evidence-based set of borderline ECG findings that are deemed normal in isolation: atrial enlargement, axis deviation, and complete bundle branch block. Only if two or more of these findings are present is the ECG deemed abnormal.
The Refined criteria have been adopted by the sports cardiologists who perform preparticipation screening for the English Football Association and other UK athletic organizations. But Dr. Malhotra and his coinvestigators also tested a further refinement of the Refined criteria in the adolescent soccer players and found it further improved the results. The refinement involved incorporation of one element of the Seattle criteria, which deems T wave inversion in the V1 and V2 leads as normal in all athletes.
When Dr. Malhotra and colleagues applied this additional refinement to the study cohort of more than 10,000 elite adolescent soccer players, they found the updated Refined criteria reduced the overall abnormal ECG rate from 2.9% to 2.1% while maintaining a specificity in excess of 96% for the detection of serious cardiac pathology. These updated Refined criteria will soon be routinely used in preparticipation screening for the Football Association’s youth development program, he added.
Session co-chair Dr. John A. Spertus was favorably impressed.
“This is really terrific work. Congratulations. I love studies that declare and define waste in effort and resources, and worry for patients, and can eliminate that,” said Dr. Spertus, professor of medicine and director of cardiovascular education and outcomes research at the Mid America Heart Institute and University of Missouri, Kansas City.
The American Academy of Pediatrics and other U.S. medical societies do not routinely recommend a preparticipation ECG at this time, but rather a preparticipation physical evaluation involving a targeted history and physical exam available at www.aap.org by searching “ppe-4 forms.”
This study was funded by Cardiac Risk in the Young and the English Football Association. Dr. Malhotra reported having no financial conflicts of interest.
CHICAGO – Results of the first-ever large study of ECG-based criteria for use in sports preparticipation screening in adolescent athletes demonstrate that the so-called Refined criteria decisively outperform the European Society of Cardiology and Seattle criteria, Dr. Aneil Malhotra reported at the annual meeting of the American College of Cardiology.
All three sets of 12-lead ECG criteria maintained an overall 92% sensitivity for the detection of serious cardiac pathology. However, the Refined criteria provided a major boost in specificity – and a markedly lower false positive rate, according to Dr. Malhotra of St. George’s, University of London.
The Refined criteria performed particularly well in the black adolescent athletes. That’s important because of black athletes’ historically high false positive rates with other ECG criteria, which lead to the time and expense of further testing, needless anxiety for the athletes and their families, and susceptibility to erroneous disqualification, he added.
The ESC recommendations for ECG interpretation in athletes were published in 2010 (Eur Heart J. 2010 Jan;31[2]:243-59). Because of their high false positive rates and the fact that the ESC criteria were derived exclusively from white athletes, an international consensus panel subsequently issued the Seattle criteria, which were developed based upon data from both black and white athletes (Br J Sports Med. 2013 Feb;47[3]:122-4).
While the Seattle criteria performed better than the ESC criteria, many sports cardiologists felt there was further room for improvement in setting criteria that differentiate between physiologic ECG patterns and those indicative of serious cardiac disease. Thus, another international expert consensus panel came up with the Refined criteria. And while the Refined criteria clearly outperformed the ESC and Seattle criteria when applied to a large group of young adult athletes (Circulation. 2014 Apr 22;129[16]:1637-49), the fact is that all three sets of criteria were developed with data from adult athletes. None had been tested in adolescent athletes, even though they are vastly more numerous than were adult athletes in every country. It was the need to validate the applicability of the adult-based criteria in adolescent athletes that was the impetus for Dr. Malhotra’s retrospective study.
He and his coinvestigators applied all three sets of criteria to a unique data set: 10,156 elite adolescent soccer players in the English Football Association’s program for the development of soccer professionals. The cohort consisted of 9,262 white and 894 black players, making this the largest-ever study conducted in adolescent black athletes. The subjects averaged just over 16 years in age and trained on average for more than 12 hours per week.
The English Football Association’s preparticipation screening program included a full history and physical examination, a 12-lead ECG, and – most importantly – an echocardiogram for every athlete, which enabled investigators to validate the ECG findings. The cost of echocardiography in young English footballers is covered by Cardiac Risk in the Young, a charitable organization.
Application of the ESC criteria resulted in an abnormal ECG requiring further investigation in 12.9% of the white athletes. With the Seattle criteria, this rate dropped to 4.2%. With the Refined criteria, it fell further to 2.8%.
In black adolescent athletes, the abnormal ECG rate was 16.2% with the ESC criteria, 5.8% with the Seattle criteria, and 3.8% using the Refined criteria.
A total of 36 cases of cardiac conditions predisposing to sudden cardiac death were identified in the overall cohort. Thirty-three of the 36 affected athletes were correctly identified by all three sets of ECG criteria, including all 28 cases of Wolf-Parkinson-White syndrome and the three cases of hypertrophic cardiomyopathy.
Armed with the true positive rates, the investigators were able to determine that the false positive ECG rates were 12.6% in whites and 15.5% in blacks with the ESC criteria, 3.9% in whites and 5.3% in blacks with the Seattle criteria, and 2.5% in whites and 3.1% in blacks by the Refined criteria.
The positive predictive value of the 12-lead ECG was more than fourfold higher with the Refined as compared with the ESC criteria: 11% versus 2.5% with the ESC and 7.5% with the Seattle criteria, Dr. Malhotra continued.
He explained that the Refined criteria differ from the other two sets of criteria as follows: There are a series of normal ECG findings in the adolescent athletes that are unrelated to training, and that experts agree don’t warrant further evaluation, such as incomplete right bundle branch block or sinus bradycardia. And there are well established ECG abnormalities that necessitate further testing. The Refined criteria establish an evidence-based set of borderline ECG findings that are deemed normal in isolation: atrial enlargement, axis deviation, and complete bundle branch block. Only if two or more of these findings are present is the ECG deemed abnormal.
The Refined criteria have been adopted by the sports cardiologists who perform preparticipation screening for the English Football Association and other UK athletic organizations. But Dr. Malhotra and his coinvestigators also tested a further refinement of the Refined criteria in the adolescent soccer players and found it further improved the results. The refinement involved incorporation of one element of the Seattle criteria, which deems T wave inversion in the V1 and V2 leads as normal in all athletes.
When Dr. Malhotra and colleagues applied this additional refinement to the study cohort of more than 10,000 elite adolescent soccer players, they found the updated Refined criteria reduced the overall abnormal ECG rate from 2.9% to 2.1% while maintaining a specificity in excess of 96% for the detection of serious cardiac pathology. These updated Refined criteria will soon be routinely used in preparticipation screening for the Football Association’s youth development program, he added.
Session co-chair Dr. John A. Spertus was favorably impressed.
“This is really terrific work. Congratulations. I love studies that declare and define waste in effort and resources, and worry for patients, and can eliminate that,” said Dr. Spertus, professor of medicine and director of cardiovascular education and outcomes research at the Mid America Heart Institute and University of Missouri, Kansas City.
The American Academy of Pediatrics and other U.S. medical societies do not routinely recommend a preparticipation ECG at this time, but rather a preparticipation physical evaluation involving a targeted history and physical exam available at www.aap.org by searching “ppe-4 forms.”
This study was funded by Cardiac Risk in the Young and the English Football Association. Dr. Malhotra reported having no financial conflicts of interest.
AT ACC 16
Key clinical point: So-called Refined criteria outperform Seattle and ESC criteria for detection of cardiac abnormalities in teen elite athletes.
Major finding: The overall abnormal screening ECG rate was 13.2% with the ESC criteria, 4.3% with the Seattle criteria, and 2.9% with the Refined criteria.
Data source: A retrospective study that applied three different sets of 12-lead ECG interpretation criteria to preparticipation screening of more than 10,000 elite adolescent United Kingdom soccer players.
Disclosures: This study was funded by Cardiac Risk in the Young and the English Football Association. The presenter reported having no financial conflicts of interest.
Strong gender difference for stroke in diabetes patients with restless legs syndrome
CHICAGO – Stroke risk in diabetic women with restless legs syndrome (RLS) is triple that of diabetic men with the sensorimotor disease, Zoe Heis reported at the annual meeting of the American College of Cardiology.
The mechanism underlying this marked gender discrepancy in risk requires further investigation, as does the highly practical question of whether improved diabetic control can reduce the stroke risk, said Ms. Heis of the Center for Integrative Research on Cardiovascular Aging at Aurora Health Care in Milwaukee.
She presented a retrospective cohort study of 385 patients diagnosed with RLS during 2011-2013 at a community sleep center using the International RLS Study Group criteria. Along with 770 propensity-matched controls, they were followed until mid-2015. At baseline, 40% of the RLS patients had diabetes and 70% had hypertension, as did 32% and 63% of controls, respectively.
Stroke occurred in 7.5% of the RLS group and 4.2% of matched controls. The presence of diabetes more than doubled the stroke risk in both groups.
The risk of stroke was 18.2% in diabetic women with RLS and 7% in diabetic men with RLS. In a multivariate analysis that controlled for potential confounding factors, this translated to a threefold increased stroke risk.
Diabetes was associated with a doubling of stroke risk in subjects without RLS, but the risk was similar in men and women, according to Ms. Heis.
In addition to diabetes and female gender, the other major predictor of increased stroke risk in patients with RLS was, not surprisingly, hypertension. It was associated with a 13-fold increased likelihood of stroke, she noted.
RLS was initially linked to increased risk of coronary heart disease in a report from the Nurses’ Health Study (Circulation. 2012 Oct 2;126[14]:1689-94). In 2015, another research group linked more severe RLS to an increased risk of stroke. Ms. Heis and her coinvestigators carried out the current study to test their hypothesis that, since diabetes is a condition that accelerates cardiovascular disease, the endocrine disorder would boost stroke risk more in subjects with RLS than in those without it.
Ms. Heis reported having no financial conflicts regarding her study, which was conducted free of commercial support.
CHICAGO – Stroke risk in diabetic women with restless legs syndrome (RLS) is triple that of diabetic men with the sensorimotor disease, Zoe Heis reported at the annual meeting of the American College of Cardiology.
The mechanism underlying this marked gender discrepancy in risk requires further investigation, as does the highly practical question of whether improved diabetic control can reduce the stroke risk, said Ms. Heis of the Center for Integrative Research on Cardiovascular Aging at Aurora Health Care in Milwaukee.
She presented a retrospective cohort study of 385 patients diagnosed with RLS during 2011-2013 at a community sleep center using the International RLS Study Group criteria. Along with 770 propensity-matched controls, they were followed until mid-2015. At baseline, 40% of the RLS patients had diabetes and 70% had hypertension, as did 32% and 63% of controls, respectively.
Stroke occurred in 7.5% of the RLS group and 4.2% of matched controls. The presence of diabetes more than doubled the stroke risk in both groups.
The risk of stroke was 18.2% in diabetic women with RLS and 7% in diabetic men with RLS. In a multivariate analysis that controlled for potential confounding factors, this translated to a threefold increased stroke risk.
Diabetes was associated with a doubling of stroke risk in subjects without RLS, but the risk was similar in men and women, according to Ms. Heis.
In addition to diabetes and female gender, the other major predictor of increased stroke risk in patients with RLS was, not surprisingly, hypertension. It was associated with a 13-fold increased likelihood of stroke, she noted.
RLS was initially linked to increased risk of coronary heart disease in a report from the Nurses’ Health Study (Circulation. 2012 Oct 2;126[14]:1689-94). In 2015, another research group linked more severe RLS to an increased risk of stroke. Ms. Heis and her coinvestigators carried out the current study to test their hypothesis that, since diabetes is a condition that accelerates cardiovascular disease, the endocrine disorder would boost stroke risk more in subjects with RLS than in those without it.
Ms. Heis reported having no financial conflicts regarding her study, which was conducted free of commercial support.
CHICAGO – Stroke risk in diabetic women with restless legs syndrome (RLS) is triple that of diabetic men with the sensorimotor disease, Zoe Heis reported at the annual meeting of the American College of Cardiology.
The mechanism underlying this marked gender discrepancy in risk requires further investigation, as does the highly practical question of whether improved diabetic control can reduce the stroke risk, said Ms. Heis of the Center for Integrative Research on Cardiovascular Aging at Aurora Health Care in Milwaukee.
She presented a retrospective cohort study of 385 patients diagnosed with RLS during 2011-2013 at a community sleep center using the International RLS Study Group criteria. Along with 770 propensity-matched controls, they were followed until mid-2015. At baseline, 40% of the RLS patients had diabetes and 70% had hypertension, as did 32% and 63% of controls, respectively.
Stroke occurred in 7.5% of the RLS group and 4.2% of matched controls. The presence of diabetes more than doubled the stroke risk in both groups.
The risk of stroke was 18.2% in diabetic women with RLS and 7% in diabetic men with RLS. In a multivariate analysis that controlled for potential confounding factors, this translated to a threefold increased stroke risk.
Diabetes was associated with a doubling of stroke risk in subjects without RLS, but the risk was similar in men and women, according to Ms. Heis.
In addition to diabetes and female gender, the other major predictor of increased stroke risk in patients with RLS was, not surprisingly, hypertension. It was associated with a 13-fold increased likelihood of stroke, she noted.
RLS was initially linked to increased risk of coronary heart disease in a report from the Nurses’ Health Study (Circulation. 2012 Oct 2;126[14]:1689-94). In 2015, another research group linked more severe RLS to an increased risk of stroke. Ms. Heis and her coinvestigators carried out the current study to test their hypothesis that, since diabetes is a condition that accelerates cardiovascular disease, the endocrine disorder would boost stroke risk more in subjects with RLS than in those without it.
Ms. Heis reported having no financial conflicts regarding her study, which was conducted free of commercial support.
AT ACC 16
Key clinical point: Diabetic women who have restless legs syndrome face a sharply elevated risk of stroke.
Major finding: Stroke occurred in 18.2% of diabetic women with restless legs syndrome, compared with 7% of men.
Data source: This retrospective cohort study included 385 patients with restless legs syndrome and 770 propensity-matched controls.
Disclosures: This study was conducted free of commercial support. The presenter reported having no financial conflicts.