User login
American College of Surgeons (ACS): Annual Clinical Congress
Nerve monitoring linked to higher risk of vocal cord paralysis
SAN FRANCISCO – Use of intraoperative nerve monitoring during thyroidectomy to avoid injuring the recurrent laryngeal nerve is counterintuitively associated with a higher risk of vocal cord paralysis, in a cohort study of data from the Nationwide Inpatient Sample.
“We do caution against perhaps the broad adoption of nerve monitoring until we can really study this further,” said Dr. Thomas K. Chung, a research fellow in the department of surgery, division of otolaryngology, at the University of Alabama at Birmingham, and the study’s lead investigator.
He and his colleagues compared outcomes between 12,742 patients who had nerve monitoring and 230,433 patients who did not (the conventional practice) while undergoing thyroidectomy between 2008 and 2011.
The proportion of patients who developed vocal cord paralysis was significantly higher with monitoring than without it (1.9% vs. 1.4%), he reported at the annual clinical congress of the American College of Surgeons. The findings were essentially the same in propensity-adjusted analyses that took into account differences between groups in preoperative factors (1.8% vs. 1.3%).
There was no evidence that the difference was related to differences in the use of laryngoscopy to check for paralysis, in hospitals’ coding and billing for monitoring, or in payers’ coverage of this surgical adjunct.
Stratified analyses looking at the extent of surgery showed total thyroidectomy with neck dissection to be the exception, as patients monitored during these more complex operations were significantly less likely to develop vocal cord paralysis than were nonmonitored counterparts (2.8% vs. 4.5%).
The more often hospitals used nerve monitoring as indicated by the volume of thyroidectomy cases, the lower the rate of vocal cord paralysis – with the exception of cases of partial thyroidectomy, in which more frequent use was associated with a counterintuitive increase in the rate of this complication, according to Dr. Chung, who disclosed that he had no relevant conflicts of interest.
“Nerve monitoring demonstrates a significant benefit particularly in complex cases such as total thyroidectomy with neck dissection,” he said. “Low nerve monitoring and utilization with partial thyroidectomy appears to be associated with higher vocal cord paralysis; with respect to the partial thyroidectomies, this may be due to the fact that the burden of complication is already so low, with vocal cord paralysis rates of about 0.8%, that additional use of nerve monitoring may not confer any benefit.”
Dr. Chung offered several possible reasons as to why monitoring may be associated with a higher risk of vocal cord paralysis, including presence of a learning curve, substitution of monitoring for direct visualization of the nerve, and false-negatives whereby a lack of signal from the monitor may lead to more aggressive ablation when the nerve is in fact nearby.
The study had its limitations, he acknowledged. “Nerve monitoring may not be coded all the time,” he said. Information about prior neck radiation and surgery, which increase the risk of vocal cord paralysis, was unavailable. “In the group with thyroidectomy with neck dissection, there is no code for central neck dissection. And even if it is a partial thyroidectomy with neck dissection, the central neck dissection would put both nerves at risk and therefore certainly increase the risk of vocal cord paralysis,” he noted.
Invited discussant Julie Ann Sosa, chief of endocrine surgery at the Duke Cancer Institute in Durham, N.C., said, “I would like to congratulate you and your whole group for tackling what is perhaps one of the most highly contested and contentious issues within endocrine surgery and otolaryngology. It’s also I think a very important area for study because there is a relative paucity of data demonstrating for or against the use of this technology as an adjunct. Current guidelines basically say it’s a wash: We can’t say one way or the other whether folks should be using it. And the anticipated guidelines, those coming out from the American Thyroid Association, similarly will say that more data are needed. So I think you are filling a clear vacuum.”
Dr. Sosa questioned the generalizability of the findings, noting that nearly two-thirds of thyroid procedures are now done in the ambulatory setting. “You used the Nationwide Inpatient Sample, so I think you are looking at a minority of cases and highly complex cases, with a length of stay on the order of 2-3 days, which is really exceptional. Most of us send home patients the same day. So how generalizable do you think your conclusions are, and have you thought about potentially using some of the ambulatory surgery databases to try to ask similar questions?” she queried.
The investigators plan to repeat analyses using the Nationwide Inpatient Sample’s ambulatory data set next, according to Dr. Chung. “Being able to see whether or not this still holds true in an outpatient setting is definitely worthwhile,” he agreed.
Dr. Sosa further wondered about the roles of bilateral versus unilateral monitoring, and continuous versus intermittent monitoring, saying, “I think the approach an individual surgeon takes could definitely result in different outcomes. So I wonder, were you able to address at a more granular level the specific technologies employed?”
The Nationwide Inpatient Sample unfortunately does not capture information on these aspects of monitoring, said Dr. Chung. However, “with respect to continuous versus intermittent, we do think that that’s actually an important variable. It is possible that those who are using nerve monitoring are doing this in a continuous fashion, so when they perhaps injure the first side of the vocal cords, they may stop. So what was originally planned to be a total thyroidectomy from the get-go that had an intraoperative nerve injury may be aborted so as to not create any disastrous airway complications. That may also artificially increase the partial thyroidectomy results, thereby increasing vocal cord paralysis complications in the partial thyroidectomy group.”
Recurrent laryngeal nerve injury resulting in vocal cord paralysis, voice, and swallowing dysfunction is a dreaded complication of thyroid surgery.
Fortunately, this is a relatively rare event, occurring anywhere from 0.5% to 2%, in experienced hands. The utilization of nerve monitoring has been proposed to potentially help decrease nerve injury, however, its real strength may be in helping to identify recurrent nerve injury intraoperatively. Knowing the recurrent laryngeal nerve is injured on one side may lead the surgeon to perform a partial thyroidectomy to avoid major airway issues.
The surgeon may choose to wait for nerve function to return before operating on the contralateral side. Utilization of nerve monitoring allows the surgeon to alter the course of the operation potentially leading to better patient outcomes.
Dr. Chung and colleagues have done an excellent job in adding valuable data to the controversial area of nerve monitoring during thyroid surgery. As they point out, their study is subject to the inherent limitations of large national database reviews. Since most thyroid surgeries are performed in the outpatient setting, it is likely that the Nationwide Inpatient Sample does not capture majority of the cases and reflects the more complicated cases, which required a longer length of stay. Recent data also suggest that the percentage of surgeons using nerve monitoring has increased significantly and that more than 70% of all fellows in training programs use nerve monitoring. This technology is not a substitute for an experienced surgeon but in the proper setting can be useful in making critical operative decisions.
Dr. Kepal N. Patel is an ACS Fellow; chief, Division of Endocrine Surgery; associate professor of surgery, biochemistry and otolaryngology; and director, Thyroid Cancer Interdisciplinary Program, New York University Langone Medical Center.
Recurrent laryngeal nerve injury resulting in vocal cord paralysis, voice, and swallowing dysfunction is a dreaded complication of thyroid surgery.
Fortunately, this is a relatively rare event, occurring anywhere from 0.5% to 2%, in experienced hands. The utilization of nerve monitoring has been proposed to potentially help decrease nerve injury, however, its real strength may be in helping to identify recurrent nerve injury intraoperatively. Knowing the recurrent laryngeal nerve is injured on one side may lead the surgeon to perform a partial thyroidectomy to avoid major airway issues.
The surgeon may choose to wait for nerve function to return before operating on the contralateral side. Utilization of nerve monitoring allows the surgeon to alter the course of the operation potentially leading to better patient outcomes.
Dr. Chung and colleagues have done an excellent job in adding valuable data to the controversial area of nerve monitoring during thyroid surgery. As they point out, their study is subject to the inherent limitations of large national database reviews. Since most thyroid surgeries are performed in the outpatient setting, it is likely that the Nationwide Inpatient Sample does not capture majority of the cases and reflects the more complicated cases, which required a longer length of stay. Recent data also suggest that the percentage of surgeons using nerve monitoring has increased significantly and that more than 70% of all fellows in training programs use nerve monitoring. This technology is not a substitute for an experienced surgeon but in the proper setting can be useful in making critical operative decisions.
Dr. Kepal N. Patel is an ACS Fellow; chief, Division of Endocrine Surgery; associate professor of surgery, biochemistry and otolaryngology; and director, Thyroid Cancer Interdisciplinary Program, New York University Langone Medical Center.
Recurrent laryngeal nerve injury resulting in vocal cord paralysis, voice, and swallowing dysfunction is a dreaded complication of thyroid surgery.
Fortunately, this is a relatively rare event, occurring anywhere from 0.5% to 2%, in experienced hands. The utilization of nerve monitoring has been proposed to potentially help decrease nerve injury, however, its real strength may be in helping to identify recurrent nerve injury intraoperatively. Knowing the recurrent laryngeal nerve is injured on one side may lead the surgeon to perform a partial thyroidectomy to avoid major airway issues.
The surgeon may choose to wait for nerve function to return before operating on the contralateral side. Utilization of nerve monitoring allows the surgeon to alter the course of the operation potentially leading to better patient outcomes.
Dr. Chung and colleagues have done an excellent job in adding valuable data to the controversial area of nerve monitoring during thyroid surgery. As they point out, their study is subject to the inherent limitations of large national database reviews. Since most thyroid surgeries are performed in the outpatient setting, it is likely that the Nationwide Inpatient Sample does not capture majority of the cases and reflects the more complicated cases, which required a longer length of stay. Recent data also suggest that the percentage of surgeons using nerve monitoring has increased significantly and that more than 70% of all fellows in training programs use nerve monitoring. This technology is not a substitute for an experienced surgeon but in the proper setting can be useful in making critical operative decisions.
Dr. Kepal N. Patel is an ACS Fellow; chief, Division of Endocrine Surgery; associate professor of surgery, biochemistry and otolaryngology; and director, Thyroid Cancer Interdisciplinary Program, New York University Langone Medical Center.
SAN FRANCISCO – Use of intraoperative nerve monitoring during thyroidectomy to avoid injuring the recurrent laryngeal nerve is counterintuitively associated with a higher risk of vocal cord paralysis, in a cohort study of data from the Nationwide Inpatient Sample.
“We do caution against perhaps the broad adoption of nerve monitoring until we can really study this further,” said Dr. Thomas K. Chung, a research fellow in the department of surgery, division of otolaryngology, at the University of Alabama at Birmingham, and the study’s lead investigator.
He and his colleagues compared outcomes between 12,742 patients who had nerve monitoring and 230,433 patients who did not (the conventional practice) while undergoing thyroidectomy between 2008 and 2011.
The proportion of patients who developed vocal cord paralysis was significantly higher with monitoring than without it (1.9% vs. 1.4%), he reported at the annual clinical congress of the American College of Surgeons. The findings were essentially the same in propensity-adjusted analyses that took into account differences between groups in preoperative factors (1.8% vs. 1.3%).
There was no evidence that the difference was related to differences in the use of laryngoscopy to check for paralysis, in hospitals’ coding and billing for monitoring, or in payers’ coverage of this surgical adjunct.
Stratified analyses looking at the extent of surgery showed total thyroidectomy with neck dissection to be the exception, as patients monitored during these more complex operations were significantly less likely to develop vocal cord paralysis than were nonmonitored counterparts (2.8% vs. 4.5%).
The more often hospitals used nerve monitoring as indicated by the volume of thyroidectomy cases, the lower the rate of vocal cord paralysis – with the exception of cases of partial thyroidectomy, in which more frequent use was associated with a counterintuitive increase in the rate of this complication, according to Dr. Chung, who disclosed that he had no relevant conflicts of interest.
“Nerve monitoring demonstrates a significant benefit particularly in complex cases such as total thyroidectomy with neck dissection,” he said. “Low nerve monitoring and utilization with partial thyroidectomy appears to be associated with higher vocal cord paralysis; with respect to the partial thyroidectomies, this may be due to the fact that the burden of complication is already so low, with vocal cord paralysis rates of about 0.8%, that additional use of nerve monitoring may not confer any benefit.”
Dr. Chung offered several possible reasons as to why monitoring may be associated with a higher risk of vocal cord paralysis, including presence of a learning curve, substitution of monitoring for direct visualization of the nerve, and false-negatives whereby a lack of signal from the monitor may lead to more aggressive ablation when the nerve is in fact nearby.
The study had its limitations, he acknowledged. “Nerve monitoring may not be coded all the time,” he said. Information about prior neck radiation and surgery, which increase the risk of vocal cord paralysis, was unavailable. “In the group with thyroidectomy with neck dissection, there is no code for central neck dissection. And even if it is a partial thyroidectomy with neck dissection, the central neck dissection would put both nerves at risk and therefore certainly increase the risk of vocal cord paralysis,” he noted.
Invited discussant Julie Ann Sosa, chief of endocrine surgery at the Duke Cancer Institute in Durham, N.C., said, “I would like to congratulate you and your whole group for tackling what is perhaps one of the most highly contested and contentious issues within endocrine surgery and otolaryngology. It’s also I think a very important area for study because there is a relative paucity of data demonstrating for or against the use of this technology as an adjunct. Current guidelines basically say it’s a wash: We can’t say one way or the other whether folks should be using it. And the anticipated guidelines, those coming out from the American Thyroid Association, similarly will say that more data are needed. So I think you are filling a clear vacuum.”
Dr. Sosa questioned the generalizability of the findings, noting that nearly two-thirds of thyroid procedures are now done in the ambulatory setting. “You used the Nationwide Inpatient Sample, so I think you are looking at a minority of cases and highly complex cases, with a length of stay on the order of 2-3 days, which is really exceptional. Most of us send home patients the same day. So how generalizable do you think your conclusions are, and have you thought about potentially using some of the ambulatory surgery databases to try to ask similar questions?” she queried.
The investigators plan to repeat analyses using the Nationwide Inpatient Sample’s ambulatory data set next, according to Dr. Chung. “Being able to see whether or not this still holds true in an outpatient setting is definitely worthwhile,” he agreed.
Dr. Sosa further wondered about the roles of bilateral versus unilateral monitoring, and continuous versus intermittent monitoring, saying, “I think the approach an individual surgeon takes could definitely result in different outcomes. So I wonder, were you able to address at a more granular level the specific technologies employed?”
The Nationwide Inpatient Sample unfortunately does not capture information on these aspects of monitoring, said Dr. Chung. However, “with respect to continuous versus intermittent, we do think that that’s actually an important variable. It is possible that those who are using nerve monitoring are doing this in a continuous fashion, so when they perhaps injure the first side of the vocal cords, they may stop. So what was originally planned to be a total thyroidectomy from the get-go that had an intraoperative nerve injury may be aborted so as to not create any disastrous airway complications. That may also artificially increase the partial thyroidectomy results, thereby increasing vocal cord paralysis complications in the partial thyroidectomy group.”
SAN FRANCISCO – Use of intraoperative nerve monitoring during thyroidectomy to avoid injuring the recurrent laryngeal nerve is counterintuitively associated with a higher risk of vocal cord paralysis, in a cohort study of data from the Nationwide Inpatient Sample.
“We do caution against perhaps the broad adoption of nerve monitoring until we can really study this further,” said Dr. Thomas K. Chung, a research fellow in the department of surgery, division of otolaryngology, at the University of Alabama at Birmingham, and the study’s lead investigator.
He and his colleagues compared outcomes between 12,742 patients who had nerve monitoring and 230,433 patients who did not (the conventional practice) while undergoing thyroidectomy between 2008 and 2011.
The proportion of patients who developed vocal cord paralysis was significantly higher with monitoring than without it (1.9% vs. 1.4%), he reported at the annual clinical congress of the American College of Surgeons. The findings were essentially the same in propensity-adjusted analyses that took into account differences between groups in preoperative factors (1.8% vs. 1.3%).
There was no evidence that the difference was related to differences in the use of laryngoscopy to check for paralysis, in hospitals’ coding and billing for monitoring, or in payers’ coverage of this surgical adjunct.
Stratified analyses looking at the extent of surgery showed total thyroidectomy with neck dissection to be the exception, as patients monitored during these more complex operations were significantly less likely to develop vocal cord paralysis than were nonmonitored counterparts (2.8% vs. 4.5%).
The more often hospitals used nerve monitoring as indicated by the volume of thyroidectomy cases, the lower the rate of vocal cord paralysis – with the exception of cases of partial thyroidectomy, in which more frequent use was associated with a counterintuitive increase in the rate of this complication, according to Dr. Chung, who disclosed that he had no relevant conflicts of interest.
“Nerve monitoring demonstrates a significant benefit particularly in complex cases such as total thyroidectomy with neck dissection,” he said. “Low nerve monitoring and utilization with partial thyroidectomy appears to be associated with higher vocal cord paralysis; with respect to the partial thyroidectomies, this may be due to the fact that the burden of complication is already so low, with vocal cord paralysis rates of about 0.8%, that additional use of nerve monitoring may not confer any benefit.”
Dr. Chung offered several possible reasons as to why monitoring may be associated with a higher risk of vocal cord paralysis, including presence of a learning curve, substitution of monitoring for direct visualization of the nerve, and false-negatives whereby a lack of signal from the monitor may lead to more aggressive ablation when the nerve is in fact nearby.
The study had its limitations, he acknowledged. “Nerve monitoring may not be coded all the time,” he said. Information about prior neck radiation and surgery, which increase the risk of vocal cord paralysis, was unavailable. “In the group with thyroidectomy with neck dissection, there is no code for central neck dissection. And even if it is a partial thyroidectomy with neck dissection, the central neck dissection would put both nerves at risk and therefore certainly increase the risk of vocal cord paralysis,” he noted.
Invited discussant Julie Ann Sosa, chief of endocrine surgery at the Duke Cancer Institute in Durham, N.C., said, “I would like to congratulate you and your whole group for tackling what is perhaps one of the most highly contested and contentious issues within endocrine surgery and otolaryngology. It’s also I think a very important area for study because there is a relative paucity of data demonstrating for or against the use of this technology as an adjunct. Current guidelines basically say it’s a wash: We can’t say one way or the other whether folks should be using it. And the anticipated guidelines, those coming out from the American Thyroid Association, similarly will say that more data are needed. So I think you are filling a clear vacuum.”
Dr. Sosa questioned the generalizability of the findings, noting that nearly two-thirds of thyroid procedures are now done in the ambulatory setting. “You used the Nationwide Inpatient Sample, so I think you are looking at a minority of cases and highly complex cases, with a length of stay on the order of 2-3 days, which is really exceptional. Most of us send home patients the same day. So how generalizable do you think your conclusions are, and have you thought about potentially using some of the ambulatory surgery databases to try to ask similar questions?” she queried.
The investigators plan to repeat analyses using the Nationwide Inpatient Sample’s ambulatory data set next, according to Dr. Chung. “Being able to see whether or not this still holds true in an outpatient setting is definitely worthwhile,” he agreed.
Dr. Sosa further wondered about the roles of bilateral versus unilateral monitoring, and continuous versus intermittent monitoring, saying, “I think the approach an individual surgeon takes could definitely result in different outcomes. So I wonder, were you able to address at a more granular level the specific technologies employed?”
The Nationwide Inpatient Sample unfortunately does not capture information on these aspects of monitoring, said Dr. Chung. However, “with respect to continuous versus intermittent, we do think that that’s actually an important variable. It is possible that those who are using nerve monitoring are doing this in a continuous fashion, so when they perhaps injure the first side of the vocal cords, they may stop. So what was originally planned to be a total thyroidectomy from the get-go that had an intraoperative nerve injury may be aborted so as to not create any disastrous airway complications. That may also artificially increase the partial thyroidectomy results, thereby increasing vocal cord paralysis complications in the partial thyroidectomy group.”
AT THE ACS CLINICAL CONGRESS
Key clinical point: Patients who had intraoperative nerve monitoring were more likely to develop vocal cord paralysis.
Major finding: The propensity-adjusted rate of vocal cord paralysis was 1.3% without monitoring and 1.8% with monitoring.
Data source: A retrospective cohort study of 243,175 patients undergoing thyroidectomy.
Disclosures: Dr. Chung disclosed that he had no relevant conflicts of interest.
Palliative consult helps geriatric trauma patients avoid futile interventions
SAN FRANCISCO – Obtaining palliative medicine consultations for geriatric trauma patients may help avoid futile interventions, suggests a retrospective cohort study reported at the annual clinical congress of the American College of Surgeons.
“The bulk of trauma in the United States has become geriatrics, and it’s falls from standing height,” noted lead investigator Dr. Christine C. Toevs, a trauma surgeon at Allegheny General Hospital in Pittsburgh; these older patients often have multiple comorbidities and are frail, and thus have a poor prognosis even with the best of care. “Clearly, this is a patient population that would benefit greatly from routine palliative medicine consultation,” she said.
Dr. Toevs and her colleagues performed a retrospective study of the charts of 5,261 trauma patients treated at their Level 1 trauma center during 2011-2013. One-third were geriatric, defined as aged 65 years or older.
Overall, 15% of geriatric patients and 2% of nongeriatric patients received a palliative medicine consult. The majority in both groups had a traumatic brain injury.
Within the geriatric age-group, about 90% of the patients who had a consult did not undergo tracheostomy and percutaneous endoscopic gastrostomy (PEG) tube placement. Mortality was about 8% in this age-group overall, but 16% in the subset who received a consult.
“It seems that palliative medicine consult within the geriatric patient population does result in [fewer] procedures,” Dr. Toevs commented. “And studies have shown that when we talk to families and patients who participate in their care, they really do not want these procedures.”
Within the nongeriatric age–group, roughly 60% of patients with a consult did not undergo tracheostomy and percutaneous endoscopic gastrostomy (PEG) tube placement. Mortality was about 3% in this age-group overall but 30% for those receiving the consult.
“Younger patients who receive palliative medicine consults seem to have the most severe injuries, not unexpectedly. These tend to be patients with the most severe traumatic brain injuries who still during their hospitalization are not demonstrating any signs of waking up. I think we all agree younger patients need a little more time than older patients, but some families don’t want to go down that route at all,” Dr. Toevs said. “So it’s reasonable before placing a trach in these patients with brain injuries, young or old, to have these discussions.”
Among all patients with a palliative medicine consult, geriatric patients were more likely to be discharged to a skilled nursing facility (32% vs. 15%), whereas nongeriatric patients were more likely to be discharged to a long-term acute care facility (13% vs. 5%) or rehabilitation facility (18% vs. 12%).
Whether avoiding long-term acute care facilities is a better outcome for geriatric patients “depends on how you look at it,” according to Dr. Toevs. “The bulk of the data suggest that 90% of all patients say that they really don’t want all that we do for them at the end of life, so most of us would consider this a better outcome.”
Three-fourths of all geriatric patients with a tracheostomy were discharged to a long-term acute care facility, although data suggest that few such patients survive to discharge. “So what we are doing is we are relocating the death rather than actually addressing the issues of what kind of life do they want,” she commented. “Do they really want the end of their lives to be in an ICU or a step-down ICU in a long-term acute care hospital? So if the patients ultimately get trached, the outcomes tend to be much worse as you can imagine and, in my mind, we have not done nearly as good a job as we should have initially; we should have in some way preempted this, and we didn’t explain to everyone well enough that this really was not considered a good outcome.”
The investigators plan further research in this area, according to Dr. Toevs, who disclosed that she had no relevant conflicts of interest. “We are looking at long-term survival data if we do send them to places after geriatric trauma – what really happens to them, what’s their survival at 6 months and a year – so that we can give [these] data to their families,” she elaborated. “We are also working with our rehab doctors to look at functional assessments and prognostication of these patients, and ultimately, really being able to quantify the benefits of palliative medicine and the goals of care discussions with these patients.”
Invited discussant Dr. Henri R. Ford, chief of surgery at the Children’s Hospital Los Angeles asked, “What were the specific criteria used, on average, to decide whether somebody should get a palliative medicine consultation? Have you tried to standardize that pretty much across the board for all of your trauma patients?”
Use of these consults at her hospital has increased since she began pushing for them, according to Dr. Toevs. “What I would like to do is to make it as routine as possible – every person on the trauma service gets a rehab consult; to some degree, every person on the trauma service should get a palliative medicine consult. It ought to be a checkbox. We are not quite there yet. But right now, I’m pushing for 80% and above, just to make it routine to begin the discussion: Do they have an advance directive? Do they have a power of attorney? Have they thought about these things long term?”
“Did you also compare the injury severity scores for the various patients, not only for the geriatric but also for those who received palliative medicine consultations versus those who did not?” Dr. Ford further asked. “That would be very, very interesting for us in terms of understanding selection bias.”
The investigators looked at these scores in another study, finding that they were lower for geriatric patients than for nongeriatric patients, as expected. “But because of their frailty, they do much poorer. And we are trying to correlate that long term when we are working with our rehab doctors and trying to look at the ability to prognosticate basically upon functional status prior to injury.”
Dr. Toevs disclosed that she had no relevant conflicts of interest.
SAN FRANCISCO – Obtaining palliative medicine consultations for geriatric trauma patients may help avoid futile interventions, suggests a retrospective cohort study reported at the annual clinical congress of the American College of Surgeons.
“The bulk of trauma in the United States has become geriatrics, and it’s falls from standing height,” noted lead investigator Dr. Christine C. Toevs, a trauma surgeon at Allegheny General Hospital in Pittsburgh; these older patients often have multiple comorbidities and are frail, and thus have a poor prognosis even with the best of care. “Clearly, this is a patient population that would benefit greatly from routine palliative medicine consultation,” she said.
Dr. Toevs and her colleagues performed a retrospective study of the charts of 5,261 trauma patients treated at their Level 1 trauma center during 2011-2013. One-third were geriatric, defined as aged 65 years or older.
Overall, 15% of geriatric patients and 2% of nongeriatric patients received a palliative medicine consult. The majority in both groups had a traumatic brain injury.
Within the geriatric age-group, about 90% of the patients who had a consult did not undergo tracheostomy and percutaneous endoscopic gastrostomy (PEG) tube placement. Mortality was about 8% in this age-group overall, but 16% in the subset who received a consult.
“It seems that palliative medicine consult within the geriatric patient population does result in [fewer] procedures,” Dr. Toevs commented. “And studies have shown that when we talk to families and patients who participate in their care, they really do not want these procedures.”
Within the nongeriatric age–group, roughly 60% of patients with a consult did not undergo tracheostomy and percutaneous endoscopic gastrostomy (PEG) tube placement. Mortality was about 3% in this age-group overall but 30% for those receiving the consult.
“Younger patients who receive palliative medicine consults seem to have the most severe injuries, not unexpectedly. These tend to be patients with the most severe traumatic brain injuries who still during their hospitalization are not demonstrating any signs of waking up. I think we all agree younger patients need a little more time than older patients, but some families don’t want to go down that route at all,” Dr. Toevs said. “So it’s reasonable before placing a trach in these patients with brain injuries, young or old, to have these discussions.”
Among all patients with a palliative medicine consult, geriatric patients were more likely to be discharged to a skilled nursing facility (32% vs. 15%), whereas nongeriatric patients were more likely to be discharged to a long-term acute care facility (13% vs. 5%) or rehabilitation facility (18% vs. 12%).
Whether avoiding long-term acute care facilities is a better outcome for geriatric patients “depends on how you look at it,” according to Dr. Toevs. “The bulk of the data suggest that 90% of all patients say that they really don’t want all that we do for them at the end of life, so most of us would consider this a better outcome.”
Three-fourths of all geriatric patients with a tracheostomy were discharged to a long-term acute care facility, although data suggest that few such patients survive to discharge. “So what we are doing is we are relocating the death rather than actually addressing the issues of what kind of life do they want,” she commented. “Do they really want the end of their lives to be in an ICU or a step-down ICU in a long-term acute care hospital? So if the patients ultimately get trached, the outcomes tend to be much worse as you can imagine and, in my mind, we have not done nearly as good a job as we should have initially; we should have in some way preempted this, and we didn’t explain to everyone well enough that this really was not considered a good outcome.”
The investigators plan further research in this area, according to Dr. Toevs, who disclosed that she had no relevant conflicts of interest. “We are looking at long-term survival data if we do send them to places after geriatric trauma – what really happens to them, what’s their survival at 6 months and a year – so that we can give [these] data to their families,” she elaborated. “We are also working with our rehab doctors to look at functional assessments and prognostication of these patients, and ultimately, really being able to quantify the benefits of palliative medicine and the goals of care discussions with these patients.”
Invited discussant Dr. Henri R. Ford, chief of surgery at the Children’s Hospital Los Angeles asked, “What were the specific criteria used, on average, to decide whether somebody should get a palliative medicine consultation? Have you tried to standardize that pretty much across the board for all of your trauma patients?”
Use of these consults at her hospital has increased since she began pushing for them, according to Dr. Toevs. “What I would like to do is to make it as routine as possible – every person on the trauma service gets a rehab consult; to some degree, every person on the trauma service should get a palliative medicine consult. It ought to be a checkbox. We are not quite there yet. But right now, I’m pushing for 80% and above, just to make it routine to begin the discussion: Do they have an advance directive? Do they have a power of attorney? Have they thought about these things long term?”
“Did you also compare the injury severity scores for the various patients, not only for the geriatric but also for those who received palliative medicine consultations versus those who did not?” Dr. Ford further asked. “That would be very, very interesting for us in terms of understanding selection bias.”
The investigators looked at these scores in another study, finding that they were lower for geriatric patients than for nongeriatric patients, as expected. “But because of their frailty, they do much poorer. And we are trying to correlate that long term when we are working with our rehab doctors and trying to look at the ability to prognosticate basically upon functional status prior to injury.”
Dr. Toevs disclosed that she had no relevant conflicts of interest.
SAN FRANCISCO – Obtaining palliative medicine consultations for geriatric trauma patients may help avoid futile interventions, suggests a retrospective cohort study reported at the annual clinical congress of the American College of Surgeons.
“The bulk of trauma in the United States has become geriatrics, and it’s falls from standing height,” noted lead investigator Dr. Christine C. Toevs, a trauma surgeon at Allegheny General Hospital in Pittsburgh; these older patients often have multiple comorbidities and are frail, and thus have a poor prognosis even with the best of care. “Clearly, this is a patient population that would benefit greatly from routine palliative medicine consultation,” she said.
Dr. Toevs and her colleagues performed a retrospective study of the charts of 5,261 trauma patients treated at their Level 1 trauma center during 2011-2013. One-third were geriatric, defined as aged 65 years or older.
Overall, 15% of geriatric patients and 2% of nongeriatric patients received a palliative medicine consult. The majority in both groups had a traumatic brain injury.
Within the geriatric age-group, about 90% of the patients who had a consult did not undergo tracheostomy and percutaneous endoscopic gastrostomy (PEG) tube placement. Mortality was about 8% in this age-group overall, but 16% in the subset who received a consult.
“It seems that palliative medicine consult within the geriatric patient population does result in [fewer] procedures,” Dr. Toevs commented. “And studies have shown that when we talk to families and patients who participate in their care, they really do not want these procedures.”
Within the nongeriatric age–group, roughly 60% of patients with a consult did not undergo tracheostomy and percutaneous endoscopic gastrostomy (PEG) tube placement. Mortality was about 3% in this age-group overall but 30% for those receiving the consult.
“Younger patients who receive palliative medicine consults seem to have the most severe injuries, not unexpectedly. These tend to be patients with the most severe traumatic brain injuries who still during their hospitalization are not demonstrating any signs of waking up. I think we all agree younger patients need a little more time than older patients, but some families don’t want to go down that route at all,” Dr. Toevs said. “So it’s reasonable before placing a trach in these patients with brain injuries, young or old, to have these discussions.”
Among all patients with a palliative medicine consult, geriatric patients were more likely to be discharged to a skilled nursing facility (32% vs. 15%), whereas nongeriatric patients were more likely to be discharged to a long-term acute care facility (13% vs. 5%) or rehabilitation facility (18% vs. 12%).
Whether avoiding long-term acute care facilities is a better outcome for geriatric patients “depends on how you look at it,” according to Dr. Toevs. “The bulk of the data suggest that 90% of all patients say that they really don’t want all that we do for them at the end of life, so most of us would consider this a better outcome.”
Three-fourths of all geriatric patients with a tracheostomy were discharged to a long-term acute care facility, although data suggest that few such patients survive to discharge. “So what we are doing is we are relocating the death rather than actually addressing the issues of what kind of life do they want,” she commented. “Do they really want the end of their lives to be in an ICU or a step-down ICU in a long-term acute care hospital? So if the patients ultimately get trached, the outcomes tend to be much worse as you can imagine and, in my mind, we have not done nearly as good a job as we should have initially; we should have in some way preempted this, and we didn’t explain to everyone well enough that this really was not considered a good outcome.”
The investigators plan further research in this area, according to Dr. Toevs, who disclosed that she had no relevant conflicts of interest. “We are looking at long-term survival data if we do send them to places after geriatric trauma – what really happens to them, what’s their survival at 6 months and a year – so that we can give [these] data to their families,” she elaborated. “We are also working with our rehab doctors to look at functional assessments and prognostication of these patients, and ultimately, really being able to quantify the benefits of palliative medicine and the goals of care discussions with these patients.”
Invited discussant Dr. Henri R. Ford, chief of surgery at the Children’s Hospital Los Angeles asked, “What were the specific criteria used, on average, to decide whether somebody should get a palliative medicine consultation? Have you tried to standardize that pretty much across the board for all of your trauma patients?”
Use of these consults at her hospital has increased since she began pushing for them, according to Dr. Toevs. “What I would like to do is to make it as routine as possible – every person on the trauma service gets a rehab consult; to some degree, every person on the trauma service should get a palliative medicine consult. It ought to be a checkbox. We are not quite there yet. But right now, I’m pushing for 80% and above, just to make it routine to begin the discussion: Do they have an advance directive? Do they have a power of attorney? Have they thought about these things long term?”
“Did you also compare the injury severity scores for the various patients, not only for the geriatric but also for those who received palliative medicine consultations versus those who did not?” Dr. Ford further asked. “That would be very, very interesting for us in terms of understanding selection bias.”
The investigators looked at these scores in another study, finding that they were lower for geriatric patients than for nongeriatric patients, as expected. “But because of their frailty, they do much poorer. And we are trying to correlate that long term when we are working with our rehab doctors and trying to look at the ability to prognosticate basically upon functional status prior to injury.”
Dr. Toevs disclosed that she had no relevant conflicts of interest.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Geriatric patients who receive a palliative medicine consult usually forgo procedures.
Major finding: About 90% of patients aged 65 years or older who had a consult did not undergo tracheostomy or PEG tube placement.
Data source: A retrospective cohort study of 5,261 trauma patients.
Disclosures: Dr. Toevs disclosed that she had no relevant conflicts of interest.
Regional lymph node mets not a risk factor for death in adrenocortical carcinoma
SAN FRANCISCO– Positive regional lymph nodes are not an independent risk factor for death from adrenocortical carcinoma, finds a cohort study presented at the annual clinical congress of the American College of Surgeons.
“High tumor grade and distant metastasis were the only independent prognostic factors,” reported lead researcher Dr. Kun-Tai Hsu, a surgical resident formerly with the University of Wisconsin–Madison and currently at Michigan State University in East Lansing.
“While regional lymph node metastasis was not associated with worse outcome, it was associated with local tumor invasion. More importantly, regional lymph node status and local tumor invasion had equivalent impact on disease-specific mortality, but lymph node status was not a marker for local tumor invasion,” he added.
Using the Surveillance, Epidemiology, and End Results (SEER) database, the researchers analyzed data for 1,202 adults who underwent surgery for unilateral adrenocortical carcinoma between 1973 and 2010. A total of 10% had regional lymph node metastases, as ascertained by sampling, imaging, or both.
Median survival was 46 months for the cohort overall, and the 5-year rate of disease-specific mortality was 55%, Dr. Hsu reported. Patients with regional lymph node metastases had higher significantly disease-specific mortality in unadjusted analyses but not in adjusted analysis. However, high tumor grade and distant metastases were both strong independent risk factors (hazard ratios, 2.37 and 2.87).
Patients were more likely to have regional lymph node metastases if they had local invasion. When peers having neither of these factors were the comparator, risk was elevated for patients with only positive lymph nodes (HR, 9.9) and for patients with only local invasion (HR, 6.7), and most for patients having both factors (HR, 18.0).
“The effect appears to be additive rather than a true interaction,” commented Dr. Hsu, who disclosed that he had no conflicts of interest relevant to the research. “Therefore, there was no synergistic interaction between local tumor invasion and regional lymph node metastases: these two disease factors equally predict disease-specific mortality and are not simply a marker of one another.”
“We are aware that there are several limitations of the SEER database,” he acknowledged. “Nevertheless, given the rare nature of adrenocortical carcinoma, SEER provided enough data to have the statistical power and objectivity not available from single-institution studies.”
In an interview, session comoderator Dr. Amelia C. Grover of the Department of Surgery’s division of surgical oncology, Virginia Commonwealth University in Richmond, said that the findings reinforce earlier research on this cancer. “The problem is, adrenocortical carcinoma is such a uncommon disease, it makes drawing a large enough group difficult. So the SEER database was a great resource,” she agreed. “However, because of its limitations, it makes it hard to draw any significant conclusions, again stressing that for these unusual endocrine neoplasms, it’s really great to have collaborative efforts from multiple institutions in driving that research forward and collecting that data so that we can better care for those patients.”
SAN FRANCISCO– Positive regional lymph nodes are not an independent risk factor for death from adrenocortical carcinoma, finds a cohort study presented at the annual clinical congress of the American College of Surgeons.
“High tumor grade and distant metastasis were the only independent prognostic factors,” reported lead researcher Dr. Kun-Tai Hsu, a surgical resident formerly with the University of Wisconsin–Madison and currently at Michigan State University in East Lansing.
“While regional lymph node metastasis was not associated with worse outcome, it was associated with local tumor invasion. More importantly, regional lymph node status and local tumor invasion had equivalent impact on disease-specific mortality, but lymph node status was not a marker for local tumor invasion,” he added.
Using the Surveillance, Epidemiology, and End Results (SEER) database, the researchers analyzed data for 1,202 adults who underwent surgery for unilateral adrenocortical carcinoma between 1973 and 2010. A total of 10% had regional lymph node metastases, as ascertained by sampling, imaging, or both.
Median survival was 46 months for the cohort overall, and the 5-year rate of disease-specific mortality was 55%, Dr. Hsu reported. Patients with regional lymph node metastases had higher significantly disease-specific mortality in unadjusted analyses but not in adjusted analysis. However, high tumor grade and distant metastases were both strong independent risk factors (hazard ratios, 2.37 and 2.87).
Patients were more likely to have regional lymph node metastases if they had local invasion. When peers having neither of these factors were the comparator, risk was elevated for patients with only positive lymph nodes (HR, 9.9) and for patients with only local invasion (HR, 6.7), and most for patients having both factors (HR, 18.0).
“The effect appears to be additive rather than a true interaction,” commented Dr. Hsu, who disclosed that he had no conflicts of interest relevant to the research. “Therefore, there was no synergistic interaction between local tumor invasion and regional lymph node metastases: these two disease factors equally predict disease-specific mortality and are not simply a marker of one another.”
“We are aware that there are several limitations of the SEER database,” he acknowledged. “Nevertheless, given the rare nature of adrenocortical carcinoma, SEER provided enough data to have the statistical power and objectivity not available from single-institution studies.”
In an interview, session comoderator Dr. Amelia C. Grover of the Department of Surgery’s division of surgical oncology, Virginia Commonwealth University in Richmond, said that the findings reinforce earlier research on this cancer. “The problem is, adrenocortical carcinoma is such a uncommon disease, it makes drawing a large enough group difficult. So the SEER database was a great resource,” she agreed. “However, because of its limitations, it makes it hard to draw any significant conclusions, again stressing that for these unusual endocrine neoplasms, it’s really great to have collaborative efforts from multiple institutions in driving that research forward and collecting that data so that we can better care for those patients.”
SAN FRANCISCO– Positive regional lymph nodes are not an independent risk factor for death from adrenocortical carcinoma, finds a cohort study presented at the annual clinical congress of the American College of Surgeons.
“High tumor grade and distant metastasis were the only independent prognostic factors,” reported lead researcher Dr. Kun-Tai Hsu, a surgical resident formerly with the University of Wisconsin–Madison and currently at Michigan State University in East Lansing.
“While regional lymph node metastasis was not associated with worse outcome, it was associated with local tumor invasion. More importantly, regional lymph node status and local tumor invasion had equivalent impact on disease-specific mortality, but lymph node status was not a marker for local tumor invasion,” he added.
Using the Surveillance, Epidemiology, and End Results (SEER) database, the researchers analyzed data for 1,202 adults who underwent surgery for unilateral adrenocortical carcinoma between 1973 and 2010. A total of 10% had regional lymph node metastases, as ascertained by sampling, imaging, or both.
Median survival was 46 months for the cohort overall, and the 5-year rate of disease-specific mortality was 55%, Dr. Hsu reported. Patients with regional lymph node metastases had higher significantly disease-specific mortality in unadjusted analyses but not in adjusted analysis. However, high tumor grade and distant metastases were both strong independent risk factors (hazard ratios, 2.37 and 2.87).
Patients were more likely to have regional lymph node metastases if they had local invasion. When peers having neither of these factors were the comparator, risk was elevated for patients with only positive lymph nodes (HR, 9.9) and for patients with only local invasion (HR, 6.7), and most for patients having both factors (HR, 18.0).
“The effect appears to be additive rather than a true interaction,” commented Dr. Hsu, who disclosed that he had no conflicts of interest relevant to the research. “Therefore, there was no synergistic interaction between local tumor invasion and regional lymph node metastases: these two disease factors equally predict disease-specific mortality and are not simply a marker of one another.”
“We are aware that there are several limitations of the SEER database,” he acknowledged. “Nevertheless, given the rare nature of adrenocortical carcinoma, SEER provided enough data to have the statistical power and objectivity not available from single-institution studies.”
In an interview, session comoderator Dr. Amelia C. Grover of the Department of Surgery’s division of surgical oncology, Virginia Commonwealth University in Richmond, said that the findings reinforce earlier research on this cancer. “The problem is, adrenocortical carcinoma is such a uncommon disease, it makes drawing a large enough group difficult. So the SEER database was a great resource,” she agreed. “However, because of its limitations, it makes it hard to draw any significant conclusions, again stressing that for these unusual endocrine neoplasms, it’s really great to have collaborative efforts from multiple institutions in driving that research forward and collecting that data so that we can better care for those patients.”
AT THE ACS CLINICAL CONGRESS
Key clinical point: Regional lymph node metastasis does not independently predict disease-specific mortality.
Major finding: Patients with involved regional nodes were not more likely to die from their cancer after other factors were taken in account.
Data source: A retrospective cohort study of 1,202 adults who had surgery for unilateral adrenocortical carcinoma.
Disclosures: Dr. Hsu disclosed that he had no relevant conflicts of interest.
High failure rate seen with limited parathyroidectomy in patients with MEN-1
SAN FRANCISCO – Patients with hyperparathyroidism due to multiple endocrine neoplasia type 1 (MEN-1) have a 4 in 10 chance of persistent hyperparathyroidism if they undergo surgery that leaves at least one gland in place, according to a retrospective cohort study presented at the annual clinical congress of the American College of Surgeons.
“Limited initial parathyroidectomy in patients with MEN-1–associated primary hyperparathyroidism results in a high failure rate. Additional enlarged contralateral parathyroid glands are frequently missed by preoperative localizing studies,” commented lead investigator Dr. Naris Nilubol, a staff clinician with the endocrine oncology branch of the Center for Cancer Research, National Cancer Institute, Bethesda, Md.
“We conclude that limited parathyroidectomy in MEN-1 guided by preoperative localizing studies is associated with high failure rates and therefore should not be performed,” he maintained.
In an interview, session comoderator Dr. Marybeth S. Hughes, a staff clinician with the thoracic and gastrointestinal oncology branch, Center for Cancer Research, National Cancer Institute, commented, “In general, I would say that the data presented just reiterates the standard of care, that MEN-1 patients should have bilateral neck exploration with [removal of] three and half glands, or four glands with autotransplantation. So it just basically solidifies what is being done standardly. I don’t think there is a compelling argument to change the standard.”
Dr. Nilubol and colleagues reviewed the charts of 99 patients with MEN-1 who underwent at least one parathyroidectomy at the National Institutes of Health (NIH).
Of the 64 patients who had initial surgery at NIH and had preoperative localizing studies done, 32 had only a single enlarged gland identified by the tests, suggesting they would be good candidates for limited surgery, according to Dr. Nilubol. Bilateral neck dissection at the time of parathyroidectomy showed that in 22 (69%) of these 32 patients, the studies had correctly identified the largest gland; however, in 19 (87%) of those 22, it missed another enlarged gland on the contralateral side. Furthermore, in 5 (16%) of the 32, the largest gland was found on the contralateral side.
With a median follow-up of 23 months, the risk of persistent hyperparathyroidism was 41% for patients who had limited parathyroidectomy (three or fewer glands removed) at initial surgery, significantly and sharply higher than the 6% seen in patients who had subtotal parathyroidectomy or more extensive surgery (at least three and a half glands removed).
Looking at the cumulative number of glands removed during initial and subsequent surgeries, 57% of patients having two or fewer glands removed and 45% of those having two and a half to three glands removed had persistent hyperparathyroidism – both significantly higher than the 5% of patients having at least three and a half glands removed.
Regarding complications, 10% of the patients who had their initial surgery at NIH developed permanent hypoparathyroidism, reported Dr. Nilubol, who disclosed that he had no relevant conflicts of interest.
Session attendees asked about the use of parathyroid hormone levels intraoperatively to guide surgery and what strategy surgeons follow at his institution in this patient population.
Previous research has suggested that intraoperative parathyroid hormone levels do not add any information that would change the operative plan, Dr. Nilubol replied. “Everybody at NIH has preop localizing studies as part of the clinical investigation, but it doesn’t change the way we approach it. Everybody gets a bilateral neck exploration and three and a half–gland removal,” provided all glands can be found, he said.
Session attendee Dr. Michael J. Campbell, a surgeon at the University California, Davis, commented, “A 10% permanent hypoparathyroidism rate in these patients – and they have a tendency to be young, most of them in their late teens, early 20s – that’s a major complication. So could you take your data and make exactly the opposite argument, that maybe you should be doing less to these patients to limit that fairly life-altering complication?” Permanent hypothyroidism at that age is “a significant medical problem,” Dr. Nilubol agreed. However, “at the NIH, we don’t operate on everybody just because they have primary hyperparathyroidism. They have to fulfill metabolic complications before we choose to operate on them. We want to delay the surgeries and [time] between the surgeries because if they live long enough, it will recur, so we want to operate when we can make the most difference, meaning [addressing] kidney stone, bone loss, etc. The most common reason for young patients is they have kidney stones, which leads to surgery.”
SAN FRANCISCO – Patients with hyperparathyroidism due to multiple endocrine neoplasia type 1 (MEN-1) have a 4 in 10 chance of persistent hyperparathyroidism if they undergo surgery that leaves at least one gland in place, according to a retrospective cohort study presented at the annual clinical congress of the American College of Surgeons.
“Limited initial parathyroidectomy in patients with MEN-1–associated primary hyperparathyroidism results in a high failure rate. Additional enlarged contralateral parathyroid glands are frequently missed by preoperative localizing studies,” commented lead investigator Dr. Naris Nilubol, a staff clinician with the endocrine oncology branch of the Center for Cancer Research, National Cancer Institute, Bethesda, Md.
“We conclude that limited parathyroidectomy in MEN-1 guided by preoperative localizing studies is associated with high failure rates and therefore should not be performed,” he maintained.
In an interview, session comoderator Dr. Marybeth S. Hughes, a staff clinician with the thoracic and gastrointestinal oncology branch, Center for Cancer Research, National Cancer Institute, commented, “In general, I would say that the data presented just reiterates the standard of care, that MEN-1 patients should have bilateral neck exploration with [removal of] three and half glands, or four glands with autotransplantation. So it just basically solidifies what is being done standardly. I don’t think there is a compelling argument to change the standard.”
Dr. Nilubol and colleagues reviewed the charts of 99 patients with MEN-1 who underwent at least one parathyroidectomy at the National Institutes of Health (NIH).
Of the 64 patients who had initial surgery at NIH and had preoperative localizing studies done, 32 had only a single enlarged gland identified by the tests, suggesting they would be good candidates for limited surgery, according to Dr. Nilubol. Bilateral neck dissection at the time of parathyroidectomy showed that in 22 (69%) of these 32 patients, the studies had correctly identified the largest gland; however, in 19 (87%) of those 22, it missed another enlarged gland on the contralateral side. Furthermore, in 5 (16%) of the 32, the largest gland was found on the contralateral side.
With a median follow-up of 23 months, the risk of persistent hyperparathyroidism was 41% for patients who had limited parathyroidectomy (three or fewer glands removed) at initial surgery, significantly and sharply higher than the 6% seen in patients who had subtotal parathyroidectomy or more extensive surgery (at least three and a half glands removed).
Looking at the cumulative number of glands removed during initial and subsequent surgeries, 57% of patients having two or fewer glands removed and 45% of those having two and a half to three glands removed had persistent hyperparathyroidism – both significantly higher than the 5% of patients having at least three and a half glands removed.
Regarding complications, 10% of the patients who had their initial surgery at NIH developed permanent hypoparathyroidism, reported Dr. Nilubol, who disclosed that he had no relevant conflicts of interest.
Session attendees asked about the use of parathyroid hormone levels intraoperatively to guide surgery and what strategy surgeons follow at his institution in this patient population.
Previous research has suggested that intraoperative parathyroid hormone levels do not add any information that would change the operative plan, Dr. Nilubol replied. “Everybody at NIH has preop localizing studies as part of the clinical investigation, but it doesn’t change the way we approach it. Everybody gets a bilateral neck exploration and three and a half–gland removal,” provided all glands can be found, he said.
Session attendee Dr. Michael J. Campbell, a surgeon at the University California, Davis, commented, “A 10% permanent hypoparathyroidism rate in these patients – and they have a tendency to be young, most of them in their late teens, early 20s – that’s a major complication. So could you take your data and make exactly the opposite argument, that maybe you should be doing less to these patients to limit that fairly life-altering complication?” Permanent hypothyroidism at that age is “a significant medical problem,” Dr. Nilubol agreed. However, “at the NIH, we don’t operate on everybody just because they have primary hyperparathyroidism. They have to fulfill metabolic complications before we choose to operate on them. We want to delay the surgeries and [time] between the surgeries because if they live long enough, it will recur, so we want to operate when we can make the most difference, meaning [addressing] kidney stone, bone loss, etc. The most common reason for young patients is they have kidney stones, which leads to surgery.”
SAN FRANCISCO – Patients with hyperparathyroidism due to multiple endocrine neoplasia type 1 (MEN-1) have a 4 in 10 chance of persistent hyperparathyroidism if they undergo surgery that leaves at least one gland in place, according to a retrospective cohort study presented at the annual clinical congress of the American College of Surgeons.
“Limited initial parathyroidectomy in patients with MEN-1–associated primary hyperparathyroidism results in a high failure rate. Additional enlarged contralateral parathyroid glands are frequently missed by preoperative localizing studies,” commented lead investigator Dr. Naris Nilubol, a staff clinician with the endocrine oncology branch of the Center for Cancer Research, National Cancer Institute, Bethesda, Md.
“We conclude that limited parathyroidectomy in MEN-1 guided by preoperative localizing studies is associated with high failure rates and therefore should not be performed,” he maintained.
In an interview, session comoderator Dr. Marybeth S. Hughes, a staff clinician with the thoracic and gastrointestinal oncology branch, Center for Cancer Research, National Cancer Institute, commented, “In general, I would say that the data presented just reiterates the standard of care, that MEN-1 patients should have bilateral neck exploration with [removal of] three and half glands, or four glands with autotransplantation. So it just basically solidifies what is being done standardly. I don’t think there is a compelling argument to change the standard.”
Dr. Nilubol and colleagues reviewed the charts of 99 patients with MEN-1 who underwent at least one parathyroidectomy at the National Institutes of Health (NIH).
Of the 64 patients who had initial surgery at NIH and had preoperative localizing studies done, 32 had only a single enlarged gland identified by the tests, suggesting they would be good candidates for limited surgery, according to Dr. Nilubol. Bilateral neck dissection at the time of parathyroidectomy showed that in 22 (69%) of these 32 patients, the studies had correctly identified the largest gland; however, in 19 (87%) of those 22, it missed another enlarged gland on the contralateral side. Furthermore, in 5 (16%) of the 32, the largest gland was found on the contralateral side.
With a median follow-up of 23 months, the risk of persistent hyperparathyroidism was 41% for patients who had limited parathyroidectomy (three or fewer glands removed) at initial surgery, significantly and sharply higher than the 6% seen in patients who had subtotal parathyroidectomy or more extensive surgery (at least three and a half glands removed).
Looking at the cumulative number of glands removed during initial and subsequent surgeries, 57% of patients having two or fewer glands removed and 45% of those having two and a half to three glands removed had persistent hyperparathyroidism – both significantly higher than the 5% of patients having at least three and a half glands removed.
Regarding complications, 10% of the patients who had their initial surgery at NIH developed permanent hypoparathyroidism, reported Dr. Nilubol, who disclosed that he had no relevant conflicts of interest.
Session attendees asked about the use of parathyroid hormone levels intraoperatively to guide surgery and what strategy surgeons follow at his institution in this patient population.
Previous research has suggested that intraoperative parathyroid hormone levels do not add any information that would change the operative plan, Dr. Nilubol replied. “Everybody at NIH has preop localizing studies as part of the clinical investigation, but it doesn’t change the way we approach it. Everybody gets a bilateral neck exploration and three and a half–gland removal,” provided all glands can be found, he said.
Session attendee Dr. Michael J. Campbell, a surgeon at the University California, Davis, commented, “A 10% permanent hypoparathyroidism rate in these patients – and they have a tendency to be young, most of them in their late teens, early 20s – that’s a major complication. So could you take your data and make exactly the opposite argument, that maybe you should be doing less to these patients to limit that fairly life-altering complication?” Permanent hypothyroidism at that age is “a significant medical problem,” Dr. Nilubol agreed. However, “at the NIH, we don’t operate on everybody just because they have primary hyperparathyroidism. They have to fulfill metabolic complications before we choose to operate on them. We want to delay the surgeries and [time] between the surgeries because if they live long enough, it will recur, so we want to operate when we can make the most difference, meaning [addressing] kidney stone, bone loss, etc. The most common reason for young patients is they have kidney stones, which leads to surgery.”
AT THE ACS CLINICAL CONGRESS
Key clinical point: Patients are more likely to have persistent hyperparathyroidism if a gland is left behind.
Major finding: The failure rate after initial parathyroidectomy was 41% with limited surgery versus 6% with subtotal or more extensive surgery.
Data source: A retrospective chart review of 99 patients with MEN-1–associated hyperparathyroidism.
Disclosures: Dr. Nilubol disclosed that he had no relevant conflicts of interest.
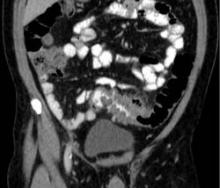
CT overutilized to diagnose appendicitis
SAN FRANCISCO – At least 25% of CT scans to diagnose appendicitis were unnecessary, potentially resulting in $1.8 million in costs at one institution and up to four new cancers from the radiation exposure, a retrospective study suggests.
The review of 1,054 patients who underwent appendectomy at the University of California, Davis, in 2005-2010 focused on costs for the patients who had high Alvarado scores, a clinical scoring system used to diagnose appendicitis, before they underwent appendectomy. CT scans to help diagnose appendicitis were performed on 77% of all patients.
Records showed that 26% of patients had an Alvarado score of 8-10, meaning that appendicitis was highly likely. CT was performed on 70% of patients with an Alvarado score of 8 and 77% of patients with a score of 9-10, comprising nearly 25% of all CT scans. That resulted in an estimated $1,813,399 in unnecessary costs for imaging, Dr. Adam Dougherty and his associates reported at the annual clinical congress of the American College of Surgeons.
This “overutilization” of CT scans delivered more than 4,009 mSv in unnecessary radiation exposure, averaging 19.75 mSV per scan, which is 20 times the annual limit suggested for safety, said Dr. Dougherty of the university. That excess radiation could be expected to produce up to four new cancers down the line, resulting in additional costs, he said.
The investigators also looked at the 9% of patients with low Alvarado scores, meaning that appendicitis was unlikely. CT scans were performed in 75% of patients with a score of 0-3 and 80% of patients with an Alvarado score of 4. In this subgroup, 24% showed normal/early pathology on appendectomy, which “argues against imaging and surgical treatment,” Dr. Dougherty said. The 44 CT scans in this subgroup resulted in an estimated $393,052 in unnecessary costs, he said.
That doesn’t include additional costs that could be expected from imaging, such as wait time, appendectomy and its sequelae, and potential workups of incidentalomas in the low-risk group, he added.
Previous studies have shown that a comprehensive clinical exam is as accurate as CT in diagnosing appendicitis, and that clinical assessment unaided by CT can reliably diagnose acute appendicitis, Dr. Dougherty said.
With a 72% increase in abdominal CT scans documented in other U.S. data from 2000 to 2005, he called for a “necessary, fundamental culture change” to restrain resource utilization “in order to maximize the value of the health care dollar while doing what is best for the patient.”
The investigators proposed a clinical pathway for the workup of suspected appendicitis that places greater emphasis on ultrasound imaging and conservative pathways, such as 23-hour admission for observation and next-day follow-up.
In the study, ultrasonography was underutilized across all subgroups as a viable alternative to CT scans, he said.
Dr. Dougherty reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – At least 25% of CT scans to diagnose appendicitis were unnecessary, potentially resulting in $1.8 million in costs at one institution and up to four new cancers from the radiation exposure, a retrospective study suggests.
The review of 1,054 patients who underwent appendectomy at the University of California, Davis, in 2005-2010 focused on costs for the patients who had high Alvarado scores, a clinical scoring system used to diagnose appendicitis, before they underwent appendectomy. CT scans to help diagnose appendicitis were performed on 77% of all patients.
Records showed that 26% of patients had an Alvarado score of 8-10, meaning that appendicitis was highly likely. CT was performed on 70% of patients with an Alvarado score of 8 and 77% of patients with a score of 9-10, comprising nearly 25% of all CT scans. That resulted in an estimated $1,813,399 in unnecessary costs for imaging, Dr. Adam Dougherty and his associates reported at the annual clinical congress of the American College of Surgeons.
This “overutilization” of CT scans delivered more than 4,009 mSv in unnecessary radiation exposure, averaging 19.75 mSV per scan, which is 20 times the annual limit suggested for safety, said Dr. Dougherty of the university. That excess radiation could be expected to produce up to four new cancers down the line, resulting in additional costs, he said.
The investigators also looked at the 9% of patients with low Alvarado scores, meaning that appendicitis was unlikely. CT scans were performed in 75% of patients with a score of 0-3 and 80% of patients with an Alvarado score of 4. In this subgroup, 24% showed normal/early pathology on appendectomy, which “argues against imaging and surgical treatment,” Dr. Dougherty said. The 44 CT scans in this subgroup resulted in an estimated $393,052 in unnecessary costs, he said.
That doesn’t include additional costs that could be expected from imaging, such as wait time, appendectomy and its sequelae, and potential workups of incidentalomas in the low-risk group, he added.
Previous studies have shown that a comprehensive clinical exam is as accurate as CT in diagnosing appendicitis, and that clinical assessment unaided by CT can reliably diagnose acute appendicitis, Dr. Dougherty said.
With a 72% increase in abdominal CT scans documented in other U.S. data from 2000 to 2005, he called for a “necessary, fundamental culture change” to restrain resource utilization “in order to maximize the value of the health care dollar while doing what is best for the patient.”
The investigators proposed a clinical pathway for the workup of suspected appendicitis that places greater emphasis on ultrasound imaging and conservative pathways, such as 23-hour admission for observation and next-day follow-up.
In the study, ultrasonography was underutilized across all subgroups as a viable alternative to CT scans, he said.
Dr. Dougherty reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – At least 25% of CT scans to diagnose appendicitis were unnecessary, potentially resulting in $1.8 million in costs at one institution and up to four new cancers from the radiation exposure, a retrospective study suggests.
The review of 1,054 patients who underwent appendectomy at the University of California, Davis, in 2005-2010 focused on costs for the patients who had high Alvarado scores, a clinical scoring system used to diagnose appendicitis, before they underwent appendectomy. CT scans to help diagnose appendicitis were performed on 77% of all patients.
Records showed that 26% of patients had an Alvarado score of 8-10, meaning that appendicitis was highly likely. CT was performed on 70% of patients with an Alvarado score of 8 and 77% of patients with a score of 9-10, comprising nearly 25% of all CT scans. That resulted in an estimated $1,813,399 in unnecessary costs for imaging, Dr. Adam Dougherty and his associates reported at the annual clinical congress of the American College of Surgeons.
This “overutilization” of CT scans delivered more than 4,009 mSv in unnecessary radiation exposure, averaging 19.75 mSV per scan, which is 20 times the annual limit suggested for safety, said Dr. Dougherty of the university. That excess radiation could be expected to produce up to four new cancers down the line, resulting in additional costs, he said.
The investigators also looked at the 9% of patients with low Alvarado scores, meaning that appendicitis was unlikely. CT scans were performed in 75% of patients with a score of 0-3 and 80% of patients with an Alvarado score of 4. In this subgroup, 24% showed normal/early pathology on appendectomy, which “argues against imaging and surgical treatment,” Dr. Dougherty said. The 44 CT scans in this subgroup resulted in an estimated $393,052 in unnecessary costs, he said.
That doesn’t include additional costs that could be expected from imaging, such as wait time, appendectomy and its sequelae, and potential workups of incidentalomas in the low-risk group, he added.
Previous studies have shown that a comprehensive clinical exam is as accurate as CT in diagnosing appendicitis, and that clinical assessment unaided by CT can reliably diagnose acute appendicitis, Dr. Dougherty said.
With a 72% increase in abdominal CT scans documented in other U.S. data from 2000 to 2005, he called for a “necessary, fundamental culture change” to restrain resource utilization “in order to maximize the value of the health care dollar while doing what is best for the patient.”
The investigators proposed a clinical pathway for the workup of suspected appendicitis that places greater emphasis on ultrasound imaging and conservative pathways, such as 23-hour admission for observation and next-day follow-up.
In the study, ultrasonography was underutilized across all subgroups as a viable alternative to CT scans, he said.
Dr. Dougherty reported having no financial disclosures.
On Twitter @sherryboschert
AT THE ACS CLINICAL CONGRESS
Key clinical point: Records showed that 26% of patients who had CT scans for suspect appendicitis had an Alvarado score of 8-10.
Major finding: A quarter of CT scans were on patients with likely appendicitis by Alvarado score, producing $1.8 million in unnecessary costs.
Data source: A retrospective study of 1,054 patients undergoing appendectomy in 2005-2010 at one institution.
Disclosures: Dr. Dougherty reported having no financial disclosures.
Corticosteroids didn’t help pediatric septic shock
SAN FRANCISCO – Adjunctive corticosteroid therapy for pediatric septic shock was associated with increased risks for a complicated course or death within 28 days in a retrospective study of data on 496 patients.
The investigators hypothesized that any potential benefit from adjunctive corticosteroids might depend on the patient’s initial risk of death, but they found no significant differences in outcomes between subgroups of patients that were rated as low risk, intermediate risk, or high risk at baseline using the Pediatric Sepsis Biomarker Risk Model (PERSEVERE) and received corticosteroids.
Among the 252 patients who received corticosteroids, 17% died within 38 days and 32% had a complicated course, defined as persistence of two or more organ failures at day 7 of septic shock or death within 28 days. Those rates were significantly higher than among the 244 patients who did not get corticosteroids, 8% of whom died within 28 days and 22% of whom had a complicated course, Dr. Sarah J. Atkinson and her associates reported.
The PERSEVERE-based mortality probability at baseline did not differ significantly between patients who did or did not get corticosteroids, though those who got corticosteroids had higher risk scores at baseline when assessed using the Pediatric Risk of Mortality score (PRISM).
Patients who got corticosteroids were twice as likely to die and nearly twice as likely to have a complicated course, compared with the no-corticosteroid group, she said at the annual clinical congress of the American College of Surgeons. The risks of death or complicated course did not differ significantly based on steroid use, however, in the 323 patients deemed to be low risk, the 117 intermediate-risk patients, or the 56 high-risk patients as rated by PERSEVERE. “Even in high-risk patients, the sickest patients, we do not even see a trend for benefit” from the use of corticosteroids, she said.
Because the corticosteroid group had a higher rate of comorbidity (42%), compared with the no-corticosteroid group (29%), the investigators conducted a sensitivity analysis of data on a subset of 321 patients without any comorbidities. Steroid use was associated with a 2.6 odds ratio for dying within 28 days and a doubling in odds for a complicated course, reported Dr. Atkinson of the University of Cincinnati.
“Risk-stratified analysis failed to demonstrate any benefit associated with corticosteroid use as adjunctive therapy for pediatric septic shock and suggests the possibility for harm in some patients,” Dr. Atkinson said. A randomized, controlled trial would be needed to identify any efficacy of corticosteroids as adjunct therapy in children with septic shock, she added.
Use of steroids in septic shock remains heavily debated, with no consensus and varying practices among physicians, she said. The 2012 update of Surviving Sepsis guidelines suggests “timely hydrocortisone therapy in children with fluid-refractory, catecholamine-resistant shock and suspected or proven absolute [classic] adrenal insufficiency,” Dr. Atkinson noted.
The current study analyzed data from a database of 27 pediatric centers on children who received corticosteroids within 7 days of ICU admission. In the corticosteroid group, 79% received hydrocortisone, 15% got methylprednisolone, and 6% received dexamethasone. Fluticasone, budesonide, or less than 48 hours of dexamethasone were classified as no steroids. Corticosteroids were administered for a median of 5 days starting on the day patients met criteria for septic shock.
Dr. Atkinson reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Adjunctive corticosteroid therapy for pediatric septic shock was associated with increased risks for a complicated course or death within 28 days in a retrospective study of data on 496 patients.
The investigators hypothesized that any potential benefit from adjunctive corticosteroids might depend on the patient’s initial risk of death, but they found no significant differences in outcomes between subgroups of patients that were rated as low risk, intermediate risk, or high risk at baseline using the Pediatric Sepsis Biomarker Risk Model (PERSEVERE) and received corticosteroids.
Among the 252 patients who received corticosteroids, 17% died within 38 days and 32% had a complicated course, defined as persistence of two or more organ failures at day 7 of septic shock or death within 28 days. Those rates were significantly higher than among the 244 patients who did not get corticosteroids, 8% of whom died within 28 days and 22% of whom had a complicated course, Dr. Sarah J. Atkinson and her associates reported.
The PERSEVERE-based mortality probability at baseline did not differ significantly between patients who did or did not get corticosteroids, though those who got corticosteroids had higher risk scores at baseline when assessed using the Pediatric Risk of Mortality score (PRISM).
Patients who got corticosteroids were twice as likely to die and nearly twice as likely to have a complicated course, compared with the no-corticosteroid group, she said at the annual clinical congress of the American College of Surgeons. The risks of death or complicated course did not differ significantly based on steroid use, however, in the 323 patients deemed to be low risk, the 117 intermediate-risk patients, or the 56 high-risk patients as rated by PERSEVERE. “Even in high-risk patients, the sickest patients, we do not even see a trend for benefit” from the use of corticosteroids, she said.
Because the corticosteroid group had a higher rate of comorbidity (42%), compared with the no-corticosteroid group (29%), the investigators conducted a sensitivity analysis of data on a subset of 321 patients without any comorbidities. Steroid use was associated with a 2.6 odds ratio for dying within 28 days and a doubling in odds for a complicated course, reported Dr. Atkinson of the University of Cincinnati.
“Risk-stratified analysis failed to demonstrate any benefit associated with corticosteroid use as adjunctive therapy for pediatric septic shock and suggests the possibility for harm in some patients,” Dr. Atkinson said. A randomized, controlled trial would be needed to identify any efficacy of corticosteroids as adjunct therapy in children with septic shock, she added.
Use of steroids in septic shock remains heavily debated, with no consensus and varying practices among physicians, she said. The 2012 update of Surviving Sepsis guidelines suggests “timely hydrocortisone therapy in children with fluid-refractory, catecholamine-resistant shock and suspected or proven absolute [classic] adrenal insufficiency,” Dr. Atkinson noted.
The current study analyzed data from a database of 27 pediatric centers on children who received corticosteroids within 7 days of ICU admission. In the corticosteroid group, 79% received hydrocortisone, 15% got methylprednisolone, and 6% received dexamethasone. Fluticasone, budesonide, or less than 48 hours of dexamethasone were classified as no steroids. Corticosteroids were administered for a median of 5 days starting on the day patients met criteria for septic shock.
Dr. Atkinson reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Adjunctive corticosteroid therapy for pediatric septic shock was associated with increased risks for a complicated course or death within 28 days in a retrospective study of data on 496 patients.
The investigators hypothesized that any potential benefit from adjunctive corticosteroids might depend on the patient’s initial risk of death, but they found no significant differences in outcomes between subgroups of patients that were rated as low risk, intermediate risk, or high risk at baseline using the Pediatric Sepsis Biomarker Risk Model (PERSEVERE) and received corticosteroids.
Among the 252 patients who received corticosteroids, 17% died within 38 days and 32% had a complicated course, defined as persistence of two or more organ failures at day 7 of septic shock or death within 28 days. Those rates were significantly higher than among the 244 patients who did not get corticosteroids, 8% of whom died within 28 days and 22% of whom had a complicated course, Dr. Sarah J. Atkinson and her associates reported.
The PERSEVERE-based mortality probability at baseline did not differ significantly between patients who did or did not get corticosteroids, though those who got corticosteroids had higher risk scores at baseline when assessed using the Pediatric Risk of Mortality score (PRISM).
Patients who got corticosteroids were twice as likely to die and nearly twice as likely to have a complicated course, compared with the no-corticosteroid group, she said at the annual clinical congress of the American College of Surgeons. The risks of death or complicated course did not differ significantly based on steroid use, however, in the 323 patients deemed to be low risk, the 117 intermediate-risk patients, or the 56 high-risk patients as rated by PERSEVERE. “Even in high-risk patients, the sickest patients, we do not even see a trend for benefit” from the use of corticosteroids, she said.
Because the corticosteroid group had a higher rate of comorbidity (42%), compared with the no-corticosteroid group (29%), the investigators conducted a sensitivity analysis of data on a subset of 321 patients without any comorbidities. Steroid use was associated with a 2.6 odds ratio for dying within 28 days and a doubling in odds for a complicated course, reported Dr. Atkinson of the University of Cincinnati.
“Risk-stratified analysis failed to demonstrate any benefit associated with corticosteroid use as adjunctive therapy for pediatric septic shock and suggests the possibility for harm in some patients,” Dr. Atkinson said. A randomized, controlled trial would be needed to identify any efficacy of corticosteroids as adjunct therapy in children with septic shock, she added.
Use of steroids in septic shock remains heavily debated, with no consensus and varying practices among physicians, she said. The 2012 update of Surviving Sepsis guidelines suggests “timely hydrocortisone therapy in children with fluid-refractory, catecholamine-resistant shock and suspected or proven absolute [classic] adrenal insufficiency,” Dr. Atkinson noted.
The current study analyzed data from a database of 27 pediatric centers on children who received corticosteroids within 7 days of ICU admission. In the corticosteroid group, 79% received hydrocortisone, 15% got methylprednisolone, and 6% received dexamethasone. Fluticasone, budesonide, or less than 48 hours of dexamethasone were classified as no steroids. Corticosteroids were administered for a median of 5 days starting on the day patients met criteria for septic shock.
Dr. Atkinson reported having no financial disclosures.
On Twitter @sherryboschert
AT THE ACS CLINICAL CONGRESS
Key clinical point: Adjunctive corticosteroid therapy didn’t offer benefits to pediatric patients with septic shock, regardless of initial mortality risk.
Major finding: With steroids, 17% died and 32% had a complicated course, versus 8% and 22% without steroids, respectively.
Data source: A retrospective analysis of multicenter data on 496 cases of pediatric septic shock.
Disclosures: Dr. Atkinson reported having no financial disclosures.
Nonoperative management okay after draining diverticular-associated abscess
SAN FRANCISCO – Patients who did not undergo elective surgical resection after successful percutaneous drainage of a diverticular-associated abscess had low rates of recurrent diverticulitis in a retrospective study, a finding that suggests nonoperative management is a reasonable option in such patients, Dr. Tarek K. Jalouta said.
Percutaneous drainage of diverticular-associated abscess resolved symptoms in 118 of 165 (72%) patients who underwent the procedure at two teaching hospitals in 2001-2013. Sixty of the patients with successful drainage did not undergo elective surgical resection, and eight of these died within a year of the drainage procedure.
Among the remaining 52 patients who had nonoperative management, 72% remained free of diverticulitis after 5 years, Dr. Jalouta and his associates reported at the annual clinical congress of the American College of Surgeons.
“A significant number of patients successfully recover from complicated diverticulitis following percutaneous drainage,” Dr. Jalouta said. “Subsequent nonoperative management carries an acceptable risk for recurrent episodes and may be considered as a reasonable management option.”
All patients diagnosed with diverticular-associated abscess received IV antibiotics within 24-48 hours of diagnosis. The decision to perform percutaneous drainage was at the discretion of the consulting surgeon and the interventional radiologist.
Practice parameters issued by the American Society of Colon and Rectal Surgeons in 2014 suggest that elective colectomy “should typically be advised” following successful medical treatment of diverticular-associated abscess with or without percutaneous drainage, noted Dr. Jalouta of Spectrum Health System, Grand Rapids, Mich. Separate guidelines from the Association of Coloproctology of Great Britain and Ireland state that there is not sufficient evidence to make a formal recommendation on this topic, he added.
For the cohort of 165 patients, the abscesses averaged 6 cm in diameter and were pelvic in 73% of patients, abdominal in 22%, and in both locations in 5%. Multiple abscesses were present in 17%. Patients had a mean age of 61 years and a mean body mass index of 21 kg/m2, and 52% were female.
The patients who did not undergo surgery after successful percutaneous drainage were significantly older than those who had surgery – 62 years vs. 55 years. Those subgroups did not differ in other respects.
An estimated 130,000 U.S. hospitalizations each year are due to diverticulitis, with 10%-20% of cases complicated by an associated intra-abdominal abscess, he said. Most diverticular-associated abscesses smaller than 5 cm in diameter will respond to antibiotic therapy, but patients with larger abscesses or associated sepsis often get percutaneous drainage.
The results were slightly better than those seen in two previous studies. In one study of 511 patients admitted for acute diverticulitis in 1994-2003, 5 of 12 patients (42%) who did not undergo surgery after percutaneous drainage of abscesses averaging 7 cm in size had a recurrence of diverticulitis (Am. J. Gastroenterol. 2005;100:910-7), Dr. Jalouta said. A separate study of 32 patients managed without surgery after percutaneous drainage of diverticular-associated abscesses found a recurrence-free survival rate of 58% after 7 years (Dis. Colon Rectum 2013;56:622-6).
Dr. Jalouta reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Patients who did not undergo elective surgical resection after successful percutaneous drainage of a diverticular-associated abscess had low rates of recurrent diverticulitis in a retrospective study, a finding that suggests nonoperative management is a reasonable option in such patients, Dr. Tarek K. Jalouta said.
Percutaneous drainage of diverticular-associated abscess resolved symptoms in 118 of 165 (72%) patients who underwent the procedure at two teaching hospitals in 2001-2013. Sixty of the patients with successful drainage did not undergo elective surgical resection, and eight of these died within a year of the drainage procedure.
Among the remaining 52 patients who had nonoperative management, 72% remained free of diverticulitis after 5 years, Dr. Jalouta and his associates reported at the annual clinical congress of the American College of Surgeons.
“A significant number of patients successfully recover from complicated diverticulitis following percutaneous drainage,” Dr. Jalouta said. “Subsequent nonoperative management carries an acceptable risk for recurrent episodes and may be considered as a reasonable management option.”
All patients diagnosed with diverticular-associated abscess received IV antibiotics within 24-48 hours of diagnosis. The decision to perform percutaneous drainage was at the discretion of the consulting surgeon and the interventional radiologist.
Practice parameters issued by the American Society of Colon and Rectal Surgeons in 2014 suggest that elective colectomy “should typically be advised” following successful medical treatment of diverticular-associated abscess with or without percutaneous drainage, noted Dr. Jalouta of Spectrum Health System, Grand Rapids, Mich. Separate guidelines from the Association of Coloproctology of Great Britain and Ireland state that there is not sufficient evidence to make a formal recommendation on this topic, he added.
For the cohort of 165 patients, the abscesses averaged 6 cm in diameter and were pelvic in 73% of patients, abdominal in 22%, and in both locations in 5%. Multiple abscesses were present in 17%. Patients had a mean age of 61 years and a mean body mass index of 21 kg/m2, and 52% were female.
The patients who did not undergo surgery after successful percutaneous drainage were significantly older than those who had surgery – 62 years vs. 55 years. Those subgroups did not differ in other respects.
An estimated 130,000 U.S. hospitalizations each year are due to diverticulitis, with 10%-20% of cases complicated by an associated intra-abdominal abscess, he said. Most diverticular-associated abscesses smaller than 5 cm in diameter will respond to antibiotic therapy, but patients with larger abscesses or associated sepsis often get percutaneous drainage.
The results were slightly better than those seen in two previous studies. In one study of 511 patients admitted for acute diverticulitis in 1994-2003, 5 of 12 patients (42%) who did not undergo surgery after percutaneous drainage of abscesses averaging 7 cm in size had a recurrence of diverticulitis (Am. J. Gastroenterol. 2005;100:910-7), Dr. Jalouta said. A separate study of 32 patients managed without surgery after percutaneous drainage of diverticular-associated abscesses found a recurrence-free survival rate of 58% after 7 years (Dis. Colon Rectum 2013;56:622-6).
Dr. Jalouta reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Patients who did not undergo elective surgical resection after successful percutaneous drainage of a diverticular-associated abscess had low rates of recurrent diverticulitis in a retrospective study, a finding that suggests nonoperative management is a reasonable option in such patients, Dr. Tarek K. Jalouta said.
Percutaneous drainage of diverticular-associated abscess resolved symptoms in 118 of 165 (72%) patients who underwent the procedure at two teaching hospitals in 2001-2013. Sixty of the patients with successful drainage did not undergo elective surgical resection, and eight of these died within a year of the drainage procedure.
Among the remaining 52 patients who had nonoperative management, 72% remained free of diverticulitis after 5 years, Dr. Jalouta and his associates reported at the annual clinical congress of the American College of Surgeons.
“A significant number of patients successfully recover from complicated diverticulitis following percutaneous drainage,” Dr. Jalouta said. “Subsequent nonoperative management carries an acceptable risk for recurrent episodes and may be considered as a reasonable management option.”
All patients diagnosed with diverticular-associated abscess received IV antibiotics within 24-48 hours of diagnosis. The decision to perform percutaneous drainage was at the discretion of the consulting surgeon and the interventional radiologist.
Practice parameters issued by the American Society of Colon and Rectal Surgeons in 2014 suggest that elective colectomy “should typically be advised” following successful medical treatment of diverticular-associated abscess with or without percutaneous drainage, noted Dr. Jalouta of Spectrum Health System, Grand Rapids, Mich. Separate guidelines from the Association of Coloproctology of Great Britain and Ireland state that there is not sufficient evidence to make a formal recommendation on this topic, he added.
For the cohort of 165 patients, the abscesses averaged 6 cm in diameter and were pelvic in 73% of patients, abdominal in 22%, and in both locations in 5%. Multiple abscesses were present in 17%. Patients had a mean age of 61 years and a mean body mass index of 21 kg/m2, and 52% were female.
The patients who did not undergo surgery after successful percutaneous drainage were significantly older than those who had surgery – 62 years vs. 55 years. Those subgroups did not differ in other respects.
An estimated 130,000 U.S. hospitalizations each year are due to diverticulitis, with 10%-20% of cases complicated by an associated intra-abdominal abscess, he said. Most diverticular-associated abscesses smaller than 5 cm in diameter will respond to antibiotic therapy, but patients with larger abscesses or associated sepsis often get percutaneous drainage.
The results were slightly better than those seen in two previous studies. In one study of 511 patients admitted for acute diverticulitis in 1994-2003, 5 of 12 patients (42%) who did not undergo surgery after percutaneous drainage of abscesses averaging 7 cm in size had a recurrence of diverticulitis (Am. J. Gastroenterol. 2005;100:910-7), Dr. Jalouta said. A separate study of 32 patients managed without surgery after percutaneous drainage of diverticular-associated abscesses found a recurrence-free survival rate of 58% after 7 years (Dis. Colon Rectum 2013;56:622-6).
Dr. Jalouta reported having no financial disclosures.
On Twitter @sherryboschert
AT THE ACS CLINICAL CONGRESS
Key clinical point: Patients can do well without elective surgical resection following successful percutaneous drainage of diverticular-associated abscess.
Major finding: No recurrent diverticulitis was seen at 5 years in 37 of 52 patients who did not have surgery.
Data source: A retrospective review of all 165 patients who underwent percutaneous drainage of diverticular-associated abscesses in 12 years at two hospitals.
Disclosures: Dr. Jalouta reported having no financial disclosures.
VIDEO: Mortality rate after elective colorectal surgery hits 2%
SAN FRANCISCO– Patients undergoing elective colorectal surgery had an overall mortality rate of 1.7% after 30 days, an analysis of data from 65,716 patients showed.
Patients with significant preoperative morbidity had a significantly higher risk of dying after the surgery, Dr. Alodia Gabre-Kidan and her associates reported at the annual clinical congress of the American College of Surgeons.
In a video interview, Dr. Gabre-Kidan discusses the results of the retrospective study, including the especially high risk for patients with preoperative renal failure or heart failure. The findings should help clinicians better counsel patients who are considering elective colorectal surgery, said Dr. Gabre-Kidan of Columbia University, New York.
Dr. Gabre-Kidan reporting having no financial disclosures.
On Twitter @sherryboschert
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO– Patients undergoing elective colorectal surgery had an overall mortality rate of 1.7% after 30 days, an analysis of data from 65,716 patients showed.
Patients with significant preoperative morbidity had a significantly higher risk of dying after the surgery, Dr. Alodia Gabre-Kidan and her associates reported at the annual clinical congress of the American College of Surgeons.
In a video interview, Dr. Gabre-Kidan discusses the results of the retrospective study, including the especially high risk for patients with preoperative renal failure or heart failure. The findings should help clinicians better counsel patients who are considering elective colorectal surgery, said Dr. Gabre-Kidan of Columbia University, New York.
Dr. Gabre-Kidan reporting having no financial disclosures.
On Twitter @sherryboschert
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO– Patients undergoing elective colorectal surgery had an overall mortality rate of 1.7% after 30 days, an analysis of data from 65,716 patients showed.
Patients with significant preoperative morbidity had a significantly higher risk of dying after the surgery, Dr. Alodia Gabre-Kidan and her associates reported at the annual clinical congress of the American College of Surgeons.
In a video interview, Dr. Gabre-Kidan discusses the results of the retrospective study, including the especially high risk for patients with preoperative renal failure or heart failure. The findings should help clinicians better counsel patients who are considering elective colorectal surgery, said Dr. Gabre-Kidan of Columbia University, New York.
Dr. Gabre-Kidan reporting having no financial disclosures.
On Twitter @sherryboschert
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACS CLINICAL CONGRESS
Mismatch seen between trends in elective, emergent colectomies for diverticulitis
SAN FRANCISCO – Performance of more elective colectomies for diverticulitis in recent years does not seem to be preventing the need for emergent or urgent colectomies, investigators reported at the annual clinical congress of the American College of Surgeons.
The investigators analyzed data from the Comprehensive Hospital Abstract Reporting System (CHARS), a Washington State inpatient database, for the years 1987-2012.
Results showed that the age- and sex-adjusted rate of elective colectomies for diverticulitis increased from about 7 per 100,000 people to more than 20 per 100,000 people. But the rate of nonelective (emergent or urgent) colectomies for this indication remained fairly stable, if anything, increasing slightly.
“Despite 15 years of evolving guidelines to operate less, we are actually seeing a threefold increase in elective colectomy for diverticulitis. We did not see a decrease in emergency surgery during the same time,” commented lead investigator Dr. Vlad V. Simianu, a research fellow in the department of surgery, University of Washington, Seattle.
Several hypotheses might explain this disconnect, he proposed: a rising incidence of diverticulitis, increasing severity of disease (although data do not support this), or surgeons’ adoption of a lower threshold for elective colectomy. “In fact, if you look at where the biggest climb in elective surgery was, it was sort of in the early 2000s, which was the time contemporaneous to when the first laparoscopic colorectal randomized trials were being published, and training programs were incorporating laparoscopy into their training. That’s really where we see the biggest jump. So it may be that what we are seeing is an increase in this procedure [laparoscopic colectomy], the same as what we saw with laparoscopic cholecystectomy.”
“Whatever you choose ... to believe about what’s driving this, what remains certain going forward is that routine elective colectomy is not supported by the most recent guidelines [from the American Society of Colon and Rectal Surgeons], and actually these guidelines are for the first time recommending that the decision to offer elective surgery be individualized,” Dr. Simianu noted.
“Our group is actually doing some neat work in this space trying to identify which metrics should be used to individualize surgery, so we look forward to sharing that with you in the future,” he added.
Session comoderator Dr. James J. Mezhir of the University of Iowa, Iowa City, asked, “It may be difficult, but are you able to look at general surgeons versus those who are colorectal trained?”
The database does not specify surgeon training, according to Dr. Simianu, who disclosed that he had no relevant conflicts of interest. “What is interesting is that in Washington State, about half the surgery is done laparoscopically, in recent years at least. Whether laparoscopy is lowering the threshold, we know that colorectal surgeons are trained to do more laparoscopic colectomy maybe than their general surgeon counterparts.”
Another state database has provided some additional relevant information, he noted. “When laparoscopy first started being adopted, we saw a spike in right-sided colon surgery, which was previously a pretty rare colectomy for diverticulitis. So it is hard to know who is sort of driving this.”
Dr. Mezhir also wanted to know, “How generalizable is this across the United States? Have you looked at something like the nationwide inpatient sample or some other data set to say whether this is something you are seeing in Washington or is this something across the U.S.?”
Similar national trends have been reported in studies using that database, according to Dr. Simianu. “One of the things they point out is that there is a spike in diverticulitis in the younger population, which is something we are seeing in Washington State as well,” he noted.
Another session attendee noted that patients with acute diverticulitis sometimes have immediate procedures, such as drainage, but then go on to have colectomy not long afterward. Thus, he wondered about misclassification, asking, “Are you capturing it as elective although it’s sorted out as an acute episode?”
“That’s a great question, said another way, are we actually just delaying things into the elective category, as opposed to operating on them emergently?” Dr. Simianu replied. “It’s a little hard to tell. We do know that during this time, rates of percutaneous drainage have gone up. So it’s sort of the same conclusion that we are doing more elective surgery but we are not really preventing complications. But I think the crux of that is when these patients have complications and have emergency surgery, they have it on their first episode, 80%-90% of them. So offering a delayed operation ... to prevent [complications] where the likelihood is highest of having a complication, doesn’t seem to bear out in the data.”
SAN FRANCISCO – Performance of more elective colectomies for diverticulitis in recent years does not seem to be preventing the need for emergent or urgent colectomies, investigators reported at the annual clinical congress of the American College of Surgeons.
The investigators analyzed data from the Comprehensive Hospital Abstract Reporting System (CHARS), a Washington State inpatient database, for the years 1987-2012.
Results showed that the age- and sex-adjusted rate of elective colectomies for diverticulitis increased from about 7 per 100,000 people to more than 20 per 100,000 people. But the rate of nonelective (emergent or urgent) colectomies for this indication remained fairly stable, if anything, increasing slightly.
“Despite 15 years of evolving guidelines to operate less, we are actually seeing a threefold increase in elective colectomy for diverticulitis. We did not see a decrease in emergency surgery during the same time,” commented lead investigator Dr. Vlad V. Simianu, a research fellow in the department of surgery, University of Washington, Seattle.
Several hypotheses might explain this disconnect, he proposed: a rising incidence of diverticulitis, increasing severity of disease (although data do not support this), or surgeons’ adoption of a lower threshold for elective colectomy. “In fact, if you look at where the biggest climb in elective surgery was, it was sort of in the early 2000s, which was the time contemporaneous to when the first laparoscopic colorectal randomized trials were being published, and training programs were incorporating laparoscopy into their training. That’s really where we see the biggest jump. So it may be that what we are seeing is an increase in this procedure [laparoscopic colectomy], the same as what we saw with laparoscopic cholecystectomy.”
“Whatever you choose ... to believe about what’s driving this, what remains certain going forward is that routine elective colectomy is not supported by the most recent guidelines [from the American Society of Colon and Rectal Surgeons], and actually these guidelines are for the first time recommending that the decision to offer elective surgery be individualized,” Dr. Simianu noted.
“Our group is actually doing some neat work in this space trying to identify which metrics should be used to individualize surgery, so we look forward to sharing that with you in the future,” he added.
Session comoderator Dr. James J. Mezhir of the University of Iowa, Iowa City, asked, “It may be difficult, but are you able to look at general surgeons versus those who are colorectal trained?”
The database does not specify surgeon training, according to Dr. Simianu, who disclosed that he had no relevant conflicts of interest. “What is interesting is that in Washington State, about half the surgery is done laparoscopically, in recent years at least. Whether laparoscopy is lowering the threshold, we know that colorectal surgeons are trained to do more laparoscopic colectomy maybe than their general surgeon counterparts.”
Another state database has provided some additional relevant information, he noted. “When laparoscopy first started being adopted, we saw a spike in right-sided colon surgery, which was previously a pretty rare colectomy for diverticulitis. So it is hard to know who is sort of driving this.”
Dr. Mezhir also wanted to know, “How generalizable is this across the United States? Have you looked at something like the nationwide inpatient sample or some other data set to say whether this is something you are seeing in Washington or is this something across the U.S.?”
Similar national trends have been reported in studies using that database, according to Dr. Simianu. “One of the things they point out is that there is a spike in diverticulitis in the younger population, which is something we are seeing in Washington State as well,” he noted.
Another session attendee noted that patients with acute diverticulitis sometimes have immediate procedures, such as drainage, but then go on to have colectomy not long afterward. Thus, he wondered about misclassification, asking, “Are you capturing it as elective although it’s sorted out as an acute episode?”
“That’s a great question, said another way, are we actually just delaying things into the elective category, as opposed to operating on them emergently?” Dr. Simianu replied. “It’s a little hard to tell. We do know that during this time, rates of percutaneous drainage have gone up. So it’s sort of the same conclusion that we are doing more elective surgery but we are not really preventing complications. But I think the crux of that is when these patients have complications and have emergency surgery, they have it on their first episode, 80%-90% of them. So offering a delayed operation ... to prevent [complications] where the likelihood is highest of having a complication, doesn’t seem to bear out in the data.”
SAN FRANCISCO – Performance of more elective colectomies for diverticulitis in recent years does not seem to be preventing the need for emergent or urgent colectomies, investigators reported at the annual clinical congress of the American College of Surgeons.
The investigators analyzed data from the Comprehensive Hospital Abstract Reporting System (CHARS), a Washington State inpatient database, for the years 1987-2012.
Results showed that the age- and sex-adjusted rate of elective colectomies for diverticulitis increased from about 7 per 100,000 people to more than 20 per 100,000 people. But the rate of nonelective (emergent or urgent) colectomies for this indication remained fairly stable, if anything, increasing slightly.
“Despite 15 years of evolving guidelines to operate less, we are actually seeing a threefold increase in elective colectomy for diverticulitis. We did not see a decrease in emergency surgery during the same time,” commented lead investigator Dr. Vlad V. Simianu, a research fellow in the department of surgery, University of Washington, Seattle.
Several hypotheses might explain this disconnect, he proposed: a rising incidence of diverticulitis, increasing severity of disease (although data do not support this), or surgeons’ adoption of a lower threshold for elective colectomy. “In fact, if you look at where the biggest climb in elective surgery was, it was sort of in the early 2000s, which was the time contemporaneous to when the first laparoscopic colorectal randomized trials were being published, and training programs were incorporating laparoscopy into their training. That’s really where we see the biggest jump. So it may be that what we are seeing is an increase in this procedure [laparoscopic colectomy], the same as what we saw with laparoscopic cholecystectomy.”
“Whatever you choose ... to believe about what’s driving this, what remains certain going forward is that routine elective colectomy is not supported by the most recent guidelines [from the American Society of Colon and Rectal Surgeons], and actually these guidelines are for the first time recommending that the decision to offer elective surgery be individualized,” Dr. Simianu noted.
“Our group is actually doing some neat work in this space trying to identify which metrics should be used to individualize surgery, so we look forward to sharing that with you in the future,” he added.
Session comoderator Dr. James J. Mezhir of the University of Iowa, Iowa City, asked, “It may be difficult, but are you able to look at general surgeons versus those who are colorectal trained?”
The database does not specify surgeon training, according to Dr. Simianu, who disclosed that he had no relevant conflicts of interest. “What is interesting is that in Washington State, about half the surgery is done laparoscopically, in recent years at least. Whether laparoscopy is lowering the threshold, we know that colorectal surgeons are trained to do more laparoscopic colectomy maybe than their general surgeon counterparts.”
Another state database has provided some additional relevant information, he noted. “When laparoscopy first started being adopted, we saw a spike in right-sided colon surgery, which was previously a pretty rare colectomy for diverticulitis. So it is hard to know who is sort of driving this.”
Dr. Mezhir also wanted to know, “How generalizable is this across the United States? Have you looked at something like the nationwide inpatient sample or some other data set to say whether this is something you are seeing in Washington or is this something across the U.S.?”
Similar national trends have been reported in studies using that database, according to Dr. Simianu. “One of the things they point out is that there is a spike in diverticulitis in the younger population, which is something we are seeing in Washington State as well,” he noted.
Another session attendee noted that patients with acute diverticulitis sometimes have immediate procedures, such as drainage, but then go on to have colectomy not long afterward. Thus, he wondered about misclassification, asking, “Are you capturing it as elective although it’s sorted out as an acute episode?”
“That’s a great question, said another way, are we actually just delaying things into the elective category, as opposed to operating on them emergently?” Dr. Simianu replied. “It’s a little hard to tell. We do know that during this time, rates of percutaneous drainage have gone up. So it’s sort of the same conclusion that we are doing more elective surgery but we are not really preventing complications. But I think the crux of that is when these patients have complications and have emergency surgery, they have it on their first episode, 80%-90% of them. So offering a delayed operation ... to prevent [complications] where the likelihood is highest of having a complication, doesn’t seem to bear out in the data.”
AT THE ACS CLINICAL CONGRESS
Key clinical point: An increase in elective colectomies has not been accompanied by a decrease in emergent/urgent colectomies.
Major finding: The adjusted rate of elective colectomies tripled, but the rate of emergent/urgent colectomies remained stable.
Data source: A cohort study of colectomies for diverticulitis in Washington State between 1987 and 2012.
Disclosures: Dr. Simianu disclosed that he had no relevant conflicts of interest.
Perioperative fluid levels increase ileus risk
SAN FRANCISCO – Too much or too little IV fluid on the day of surgery was associated with a 10%-12% increased risk for postoperative ileus in a retrospective study of 84,722 patients undergoing colon surgery.
Patients who received more than 5 liters of IV fluid on the day of surgery had a 10% increased risk of postoperative ileus and patients who received no more than 1.7 L on the surgery had a 12% increased risk of postoperative ileus, compared with patients who received 1.71-5 L of fluid, Dr. Julie K. Marosky Thacker and her associates reported at the annual clinical congress of the American College of Surgeons.
“This is one of the first studies to show that in a U.S.-based review, we have a significant number of patients getting over 5 L of fluid on the day of colon operation,” and that both high and low fluids increase the risk of postoperative ileus, Dr. Thacker said. “Observed fluid use is not compliant with the recommendations that are widespread and described in the principles of Enhance Recovery After Surgery.”
Perhaps optimizing fluids could decrease postoperative ileus and improve outcomes, she added.
The observational study of data on adults undergoing colon surgery at 524 U.S. hospitals found a wide variation in the amount of IV fluids used on the day of surgery, ranging from none to more than 8 L, with a median of 3.1 L, Dr. Thacker of Duke University, Durham, N.C., said. The researchers defined excessive fluids as the highest quartile of fluid levels and low fluids as the lowest quartile.
Overall, 18% of patients developed postoperative ileus. The higher risk for ileus with low or high IV fluids on the day of surgery was seen in open and laparoscopic procedures.
Patients with ileus had significantly longer hospitalizations, higher costs, and increased likelihood of readmission, compared with patients without ileus. The hospital length of stay averaged 10 days with ileus and 6 days without ileus. Total costs averaged $20,734 per patient with ileus and $13,865 without ileus. Among patients with ileus, readmission rates were 14% within 30 days, 17% within 60 days, and 20% within 90 days. Among patients without ileus, readmission rates were 9%, 12%, and 14% at those time points, respectively.
Data for the study came from the Premier Data research database of a nationally representative sample of adult patients having colon surgery from January 1, 2008 through June 30, 2012. Procedures included laparoscopic partial excision of the large intestine, isolation of a segment of the large intestine, open and other partial excisions of the large intestine, total intra-abdominal colectomy, anastomosis of the small intestine to the rectal stump, and other small-to-large intestinal anastomoses.
Patients had a mean age of 62 years, 46% were male, and 73% were white. Forty-six percent of patients were covered by Medicare and 36% by managed care plans. Sixty-one percent of hospitals were nonteaching hospitals, and 89% were in an urban location.
The analysis adjusted for the influence of multiple other factors that may be associated with the risk of ileus, she said.
Deltex Medical, which markets fluid monitoring systems, funded the study. Dr. Thacker has been a consultant for Deltex and for Premier Data Inc., which acquired the data.
On Twitter @sherryboschert
SAN FRANCISCO – Too much or too little IV fluid on the day of surgery was associated with a 10%-12% increased risk for postoperative ileus in a retrospective study of 84,722 patients undergoing colon surgery.
Patients who received more than 5 liters of IV fluid on the day of surgery had a 10% increased risk of postoperative ileus and patients who received no more than 1.7 L on the surgery had a 12% increased risk of postoperative ileus, compared with patients who received 1.71-5 L of fluid, Dr. Julie K. Marosky Thacker and her associates reported at the annual clinical congress of the American College of Surgeons.
“This is one of the first studies to show that in a U.S.-based review, we have a significant number of patients getting over 5 L of fluid on the day of colon operation,” and that both high and low fluids increase the risk of postoperative ileus, Dr. Thacker said. “Observed fluid use is not compliant with the recommendations that are widespread and described in the principles of Enhance Recovery After Surgery.”
Perhaps optimizing fluids could decrease postoperative ileus and improve outcomes, she added.
The observational study of data on adults undergoing colon surgery at 524 U.S. hospitals found a wide variation in the amount of IV fluids used on the day of surgery, ranging from none to more than 8 L, with a median of 3.1 L, Dr. Thacker of Duke University, Durham, N.C., said. The researchers defined excessive fluids as the highest quartile of fluid levels and low fluids as the lowest quartile.
Overall, 18% of patients developed postoperative ileus. The higher risk for ileus with low or high IV fluids on the day of surgery was seen in open and laparoscopic procedures.
Patients with ileus had significantly longer hospitalizations, higher costs, and increased likelihood of readmission, compared with patients without ileus. The hospital length of stay averaged 10 days with ileus and 6 days without ileus. Total costs averaged $20,734 per patient with ileus and $13,865 without ileus. Among patients with ileus, readmission rates were 14% within 30 days, 17% within 60 days, and 20% within 90 days. Among patients without ileus, readmission rates were 9%, 12%, and 14% at those time points, respectively.
Data for the study came from the Premier Data research database of a nationally representative sample of adult patients having colon surgery from January 1, 2008 through June 30, 2012. Procedures included laparoscopic partial excision of the large intestine, isolation of a segment of the large intestine, open and other partial excisions of the large intestine, total intra-abdominal colectomy, anastomosis of the small intestine to the rectal stump, and other small-to-large intestinal anastomoses.
Patients had a mean age of 62 years, 46% were male, and 73% were white. Forty-six percent of patients were covered by Medicare and 36% by managed care plans. Sixty-one percent of hospitals were nonteaching hospitals, and 89% were in an urban location.
The analysis adjusted for the influence of multiple other factors that may be associated with the risk of ileus, she said.
Deltex Medical, which markets fluid monitoring systems, funded the study. Dr. Thacker has been a consultant for Deltex and for Premier Data Inc., which acquired the data.
On Twitter @sherryboschert
SAN FRANCISCO – Too much or too little IV fluid on the day of surgery was associated with a 10%-12% increased risk for postoperative ileus in a retrospective study of 84,722 patients undergoing colon surgery.
Patients who received more than 5 liters of IV fluid on the day of surgery had a 10% increased risk of postoperative ileus and patients who received no more than 1.7 L on the surgery had a 12% increased risk of postoperative ileus, compared with patients who received 1.71-5 L of fluid, Dr. Julie K. Marosky Thacker and her associates reported at the annual clinical congress of the American College of Surgeons.
“This is one of the first studies to show that in a U.S.-based review, we have a significant number of patients getting over 5 L of fluid on the day of colon operation,” and that both high and low fluids increase the risk of postoperative ileus, Dr. Thacker said. “Observed fluid use is not compliant with the recommendations that are widespread and described in the principles of Enhance Recovery After Surgery.”
Perhaps optimizing fluids could decrease postoperative ileus and improve outcomes, she added.
The observational study of data on adults undergoing colon surgery at 524 U.S. hospitals found a wide variation in the amount of IV fluids used on the day of surgery, ranging from none to more than 8 L, with a median of 3.1 L, Dr. Thacker of Duke University, Durham, N.C., said. The researchers defined excessive fluids as the highest quartile of fluid levels and low fluids as the lowest quartile.
Overall, 18% of patients developed postoperative ileus. The higher risk for ileus with low or high IV fluids on the day of surgery was seen in open and laparoscopic procedures.
Patients with ileus had significantly longer hospitalizations, higher costs, and increased likelihood of readmission, compared with patients without ileus. The hospital length of stay averaged 10 days with ileus and 6 days without ileus. Total costs averaged $20,734 per patient with ileus and $13,865 without ileus. Among patients with ileus, readmission rates were 14% within 30 days, 17% within 60 days, and 20% within 90 days. Among patients without ileus, readmission rates were 9%, 12%, and 14% at those time points, respectively.
Data for the study came from the Premier Data research database of a nationally representative sample of adult patients having colon surgery from January 1, 2008 through June 30, 2012. Procedures included laparoscopic partial excision of the large intestine, isolation of a segment of the large intestine, open and other partial excisions of the large intestine, total intra-abdominal colectomy, anastomosis of the small intestine to the rectal stump, and other small-to-large intestinal anastomoses.
Patients had a mean age of 62 years, 46% were male, and 73% were white. Forty-six percent of patients were covered by Medicare and 36% by managed care plans. Sixty-one percent of hospitals were nonteaching hospitals, and 89% were in an urban location.
The analysis adjusted for the influence of multiple other factors that may be associated with the risk of ileus, she said.
Deltex Medical, which markets fluid monitoring systems, funded the study. Dr. Thacker has been a consultant for Deltex and for Premier Data Inc., which acquired the data.
On Twitter @sherryboschert
AT THE ACS CLINICAL CONGRESS
Key clinical point: Giving no more than 1.7 liters or more than 5 liters of IV fluids on the day of surgery increased the risk of ileus.
Major finding: The ileus risk was 10% higher with excessive IV fluids and 12% higher with low fluids.
Data source: A retrospective observational cohort study of data on 84,722 patients undergoing colon surgery.
Disclosures: Deltex Medical, which markets fluid monitoring systems, funded the study. Dr. Thacker has been a consultant for Deltex and for Premier Data Inc., which acquired the data.