User login
Oncology treatment errors: Emerging data shed light on risk factors, prevention
ORLANDO – Accumulating evidence is helping researchers better understand why errors occur during the delivery of cancer treatment and how to prevent them. Findings from a trio of studies were reported at a symposium on quality care sponsored by the American Society of Clinical Oncology.
Identifying causes of incidents in radiation therapy
In the first study, Greg D. Judy, MD, a radiation oncology resident at the University of North Carolina at Chapel Hill, and his colleagues retrospectively reviewed records in their institution’s reporting system, called Good Catch, to identify near-miss incidents (ones that didn’t reach the patient) and safety incidents (ones that did) among patients undergoing radiation therapy from October 2014 through April 2016.
Multivariate analysis showed that patients had a significantly higher risk of near-miss or safety incidents if they had stage T2 disease (odds ratio, 3.3), were being treated for cancer involving the head and neck (5.2), or were receiving image-guided intensity-modulated radiation therapy (3.0) or daily imaging as part of their treatment (7.0), Dr. Judy reported.
“Head and neck site and image-guided IMRT [intensity-modulated radiation therapy] are complex entities: They have multiple steps in both the planning and delivery phase,” he said. “Daily imaging as well. It’s a much more complex process to do daily imaging for setup verification than it is to do once-a-week or even once-every-2-weeks setup verification.”
On the other hand, it was unclear why T2 stage was a risk factor. “We kind of hypothesized that it might be more of the disease site that really drives this, as you can have HPV-positive oropharyngeal cancer which usually has lower T stages and more advanced nodal stages, but even then, that’s a head and neck site and we usually use image-guided IMRT, which are both very complex entities,” he said. The most common root causes for the incidents were issues related to documentation and scheduling (29% each), followed by issues related to communication (22%), technical treatment planning (14%), and technical treatment delivery (6%).
Incidents having a communication root cause were more likely than were others to affect patients (P less than .001), and those having a technical treatment delivery root cause were more likely to have higher severity (P = .005).
“Like some other studies, we found really the key factor was the complexity of the treatment plan and complexity of the overall process that is the real driving factor. This is important to understand because it promotes the idea of developing a more dedicated and robust QA system for complex cases,” said Dr. Judy. “It also highlights the importance of a strong reporting system to support a safety culture, as well as promote the continuous learning improvements within a department.”
The national Radiation Oncology Incident Learning System (RO-ILS) has been developed by the American Society for Radiation Oncology (ASTRO). “This is gaining membership very rapidly, and it’s good because it facilitates cooperative research and also safety standards for our field,” he maintained.
“I’ll argue that they did that for a variety of reasons,” he elaborated. “Strong and effective leadership by Dr. Larry Marks, who’s really created a departmental culture of safety in which people can feel free to speak up. They have this wonderful Good Catch program in place. And they have these simulation review huddles ... where people feel free to talk about what happened yesterday or today that may be relevant moving forward.”
As for the national RO-ILS initiative, “I would look out to the audience and say, why is it that we don’t have such a program in medical oncology?” Dr. Jacobson said. “It’s probably time for us to do this,” he maintained.
Reducing chemotherapy errors in pediatric oncology
In the second study, Brian D. Weiss, MD, associate director of safety and compliance at Cincinnati Children’s Hospital Medical Center, and his colleagues studied the impact of a safety initiative to prevent chemotherapy errors at their large urban pediatric academic center (J Clin Oncol 35, 2017 [suppl 8S; abstract 37]).
“Pediatric chemotherapy protocols are different from adult protocols. We dose based on age or weight or body surface area, and that can change within a protocol. You have to do adjustments every time they gain weight or grow some, which is different than for adult protocols,” he explained. “We have parents administering chemo at home. And the protocols most patients are on are very complicated, but there is no standardized format, so it makes crucial information for dose adjustments difficult to find.”
The team successively implemented about half a dozen interventions, such as dedicated chemotherapy safety zones where staff were not to be disturbed while checking orders and ear protectors as a visual deterrent to interruptions; a new chemotherapy registered nurse role with a detailed list of responsibilities; an event-reporting system to supplement the center’s error-reporting system and capture events not reaching the patient (near-miss events); and a daily chemotherapy huddle to discuss errors in a nonpunitive setting and review upcoming chemotherapy for readiness.
In the 6 years after the start of the initiative, 105,187 chemotherapy doses were administered at the center and 998 errors occurred, including 250 errors that reached the patient, according to results reported at the symposium and recently published (J Oncol Pract. 2017 April;13:e329-e336).
At the 22-month mark, the rate of chemotherapy errors reaching the patient had fallen from 3.8 in 1,000 doses at baseline to 1.9 in 1,000 doses. The reduction has since persisted for more than 4 years and translates to an estimated 155 fewer predicted errors reaching the patient because of the initiative.
“The errors that reached the patient were more often administration and dispensing errors,” Dr. Weiss said. “About two-thirds of those errors that didn’t reach the patient – because they got caught by the pharmacists and the nurses – were prescription errors.
“Our chemotherapy huddle has certainly increased our reporting of errors. We also now use it for patients on clinical trials ... any patient getting PK [pharmacokinetics] or PD [pharmacodynamics] sampled within the next 24 hours is reviewed at that meeting. And our missed samples have gone down significantly,” he noted. “It’s allowed us to manage our bed space better because now everybody knows who’s definitely coming in the next day and who’s maybe coming in the next day.”
“We are a large urban academic pediatric medical center. Some of these things may seem difficult to translate [to smaller facilities], but I’m not sure they are,” concluded Dr. Weiss.
Dr. Jacobson, the discussant, noted that the initiative was in keeping with this health system’s longstanding “obsessive” focus on patient safety and commended its rigorousness in, for example, setting clear goals, focusing on key drivers [processes] needed for change, and selecting a good outcome metric.
“This is very successful project,” he said. The success can be attributed to “strong and effective organization and leadership, building a culture of safety at Cincinnati Children’s Hospital, and an important predefined measurement program and methodology.”
Building chemotherapy regimens more accurately
In the third study, a team led by Andrea Crespo, BSc, BScPhm, BCOP, an oncology pharmacist and member of the Systemic Treatment Team at Cancer Care Ontario, Toronto, studied errors introduced when chemotherapy regimens were moved from publications into orders used by centers in the province (J Clin Oncol. 35, 2017 [suppl 8S; abstract 51]).
Nearly all outpatient intravenous systemic treatment visits in Ontario are supported by a Systemic Treatment Computerized Prescriber Order Entry (ST-CPOE) system, she noted. Such systems can reduce error rates but are not foolproof.
She and her colleagues asked all Ontario treatment centers to review their active chemotherapy regimens. Data were analyzed to determine whether the regimens were built as intended with respect to their component drugs and doses, leading to identification of any unintentional discrepancies with the original regimen.
A total of 33 centers performed the review, and the median number of regimens reviewed was 375 per center, Ms. Crespo reported.
Unintentional discrepancies in regimens were found at 27% of centers. The total number reported was 369 discrepancies, with a range from 2 to 198 per center.
All of the nine centers where discrepancies were found participated in the provincial ST-CPOE system, and most had for at least 20 years. Furthermore, eight of them used a team of at least two pharmacists and one oncologist to build their regimens. “So you can see that discrepancies occurred despite a fairly rigorous regimen-build process and many years of experience with the system,” she said.
Of the 369 total discrepancies, 41% were related to alignment with the Systemic Treatment Quality-Based Program regimen, and 32% were regimens flagged to be inactivated because of outdated information, new standards, or lack of use.
A detailed analysis of the remaining 27%, or 101 unintentional discrepancies, showed that the majority were due to missing information (35.6%) or missing drugs (13.9%), incorrect doses (10.9%), and incorrect or missing schedules (10.9%). Potential to cause harm was mild for 55%, moderate for 28%, and none for 17%.
“Corrective action has been taken to address the discrepancies identified,” said Ms. Crespo.
Only 6% of the 33 centers reported having an established regimen review and maintenance process in place before the study, but all now have such a process. In addition, some centers that did not find any regimen discrepancies nonetheless reported adding quality improvement activities, such as changes in the ways regimens were built and documented, and revising regimen names to facilitate accurate selection.
In discussing the study, Dr. Jacobson noted the low proportion of centers having an established process at baseline to ensure appropriate regimen maintenance and updates. “You might want to think to yourselves, the medical oncologists in the group, whether your center has such a process in place,” he proposed.
It is not yet known whether the project has met its goal of improving the quality and accuracy of oncology regimens in Ontario, he maintained. “We are going to have to invite [Ms. Crespo] back in a year or two to see whether that turns out to be true.” On the other hand, “clearly what they have achieved was the ability to measure the variance between what was intended and what was actually built.”
Chief among the reasons for success, again, “was a strong and effective leadership and organizational structure, not at the department level or hospital level, but across the entire province through Cancer Care Ontario,” Dr. Jacobson said. “It’s clear that they have a focus on quality and patient safety, and this measurement program that they have put in place turned out to be useful.”
Dr. Judy, Dr. Weiss, and Ms. Crespo disclosed that they had no relevant conflicts of interest.
ORLANDO – Accumulating evidence is helping researchers better understand why errors occur during the delivery of cancer treatment and how to prevent them. Findings from a trio of studies were reported at a symposium on quality care sponsored by the American Society of Clinical Oncology.
Identifying causes of incidents in radiation therapy
In the first study, Greg D. Judy, MD, a radiation oncology resident at the University of North Carolina at Chapel Hill, and his colleagues retrospectively reviewed records in their institution’s reporting system, called Good Catch, to identify near-miss incidents (ones that didn’t reach the patient) and safety incidents (ones that did) among patients undergoing radiation therapy from October 2014 through April 2016.
Multivariate analysis showed that patients had a significantly higher risk of near-miss or safety incidents if they had stage T2 disease (odds ratio, 3.3), were being treated for cancer involving the head and neck (5.2), or were receiving image-guided intensity-modulated radiation therapy (3.0) or daily imaging as part of their treatment (7.0), Dr. Judy reported.
“Head and neck site and image-guided IMRT [intensity-modulated radiation therapy] are complex entities: They have multiple steps in both the planning and delivery phase,” he said. “Daily imaging as well. It’s a much more complex process to do daily imaging for setup verification than it is to do once-a-week or even once-every-2-weeks setup verification.”
On the other hand, it was unclear why T2 stage was a risk factor. “We kind of hypothesized that it might be more of the disease site that really drives this, as you can have HPV-positive oropharyngeal cancer which usually has lower T stages and more advanced nodal stages, but even then, that’s a head and neck site and we usually use image-guided IMRT, which are both very complex entities,” he said. The most common root causes for the incidents were issues related to documentation and scheduling (29% each), followed by issues related to communication (22%), technical treatment planning (14%), and technical treatment delivery (6%).
Incidents having a communication root cause were more likely than were others to affect patients (P less than .001), and those having a technical treatment delivery root cause were more likely to have higher severity (P = .005).
“Like some other studies, we found really the key factor was the complexity of the treatment plan and complexity of the overall process that is the real driving factor. This is important to understand because it promotes the idea of developing a more dedicated and robust QA system for complex cases,” said Dr. Judy. “It also highlights the importance of a strong reporting system to support a safety culture, as well as promote the continuous learning improvements within a department.”
The national Radiation Oncology Incident Learning System (RO-ILS) has been developed by the American Society for Radiation Oncology (ASTRO). “This is gaining membership very rapidly, and it’s good because it facilitates cooperative research and also safety standards for our field,” he maintained.
“I’ll argue that they did that for a variety of reasons,” he elaborated. “Strong and effective leadership by Dr. Larry Marks, who’s really created a departmental culture of safety in which people can feel free to speak up. They have this wonderful Good Catch program in place. And they have these simulation review huddles ... where people feel free to talk about what happened yesterday or today that may be relevant moving forward.”
As for the national RO-ILS initiative, “I would look out to the audience and say, why is it that we don’t have such a program in medical oncology?” Dr. Jacobson said. “It’s probably time for us to do this,” he maintained.
Reducing chemotherapy errors in pediatric oncology
In the second study, Brian D. Weiss, MD, associate director of safety and compliance at Cincinnati Children’s Hospital Medical Center, and his colleagues studied the impact of a safety initiative to prevent chemotherapy errors at their large urban pediatric academic center (J Clin Oncol 35, 2017 [suppl 8S; abstract 37]).
“Pediatric chemotherapy protocols are different from adult protocols. We dose based on age or weight or body surface area, and that can change within a protocol. You have to do adjustments every time they gain weight or grow some, which is different than for adult protocols,” he explained. “We have parents administering chemo at home. And the protocols most patients are on are very complicated, but there is no standardized format, so it makes crucial information for dose adjustments difficult to find.”
The team successively implemented about half a dozen interventions, such as dedicated chemotherapy safety zones where staff were not to be disturbed while checking orders and ear protectors as a visual deterrent to interruptions; a new chemotherapy registered nurse role with a detailed list of responsibilities; an event-reporting system to supplement the center’s error-reporting system and capture events not reaching the patient (near-miss events); and a daily chemotherapy huddle to discuss errors in a nonpunitive setting and review upcoming chemotherapy for readiness.
In the 6 years after the start of the initiative, 105,187 chemotherapy doses were administered at the center and 998 errors occurred, including 250 errors that reached the patient, according to results reported at the symposium and recently published (J Oncol Pract. 2017 April;13:e329-e336).
At the 22-month mark, the rate of chemotherapy errors reaching the patient had fallen from 3.8 in 1,000 doses at baseline to 1.9 in 1,000 doses. The reduction has since persisted for more than 4 years and translates to an estimated 155 fewer predicted errors reaching the patient because of the initiative.
“The errors that reached the patient were more often administration and dispensing errors,” Dr. Weiss said. “About two-thirds of those errors that didn’t reach the patient – because they got caught by the pharmacists and the nurses – were prescription errors.
“Our chemotherapy huddle has certainly increased our reporting of errors. We also now use it for patients on clinical trials ... any patient getting PK [pharmacokinetics] or PD [pharmacodynamics] sampled within the next 24 hours is reviewed at that meeting. And our missed samples have gone down significantly,” he noted. “It’s allowed us to manage our bed space better because now everybody knows who’s definitely coming in the next day and who’s maybe coming in the next day.”
“We are a large urban academic pediatric medical center. Some of these things may seem difficult to translate [to smaller facilities], but I’m not sure they are,” concluded Dr. Weiss.
Dr. Jacobson, the discussant, noted that the initiative was in keeping with this health system’s longstanding “obsessive” focus on patient safety and commended its rigorousness in, for example, setting clear goals, focusing on key drivers [processes] needed for change, and selecting a good outcome metric.
“This is very successful project,” he said. The success can be attributed to “strong and effective organization and leadership, building a culture of safety at Cincinnati Children’s Hospital, and an important predefined measurement program and methodology.”
Building chemotherapy regimens more accurately
In the third study, a team led by Andrea Crespo, BSc, BScPhm, BCOP, an oncology pharmacist and member of the Systemic Treatment Team at Cancer Care Ontario, Toronto, studied errors introduced when chemotherapy regimens were moved from publications into orders used by centers in the province (J Clin Oncol. 35, 2017 [suppl 8S; abstract 51]).
Nearly all outpatient intravenous systemic treatment visits in Ontario are supported by a Systemic Treatment Computerized Prescriber Order Entry (ST-CPOE) system, she noted. Such systems can reduce error rates but are not foolproof.
She and her colleagues asked all Ontario treatment centers to review their active chemotherapy regimens. Data were analyzed to determine whether the regimens were built as intended with respect to their component drugs and doses, leading to identification of any unintentional discrepancies with the original regimen.
A total of 33 centers performed the review, and the median number of regimens reviewed was 375 per center, Ms. Crespo reported.
Unintentional discrepancies in regimens were found at 27% of centers. The total number reported was 369 discrepancies, with a range from 2 to 198 per center.
All of the nine centers where discrepancies were found participated in the provincial ST-CPOE system, and most had for at least 20 years. Furthermore, eight of them used a team of at least two pharmacists and one oncologist to build their regimens. “So you can see that discrepancies occurred despite a fairly rigorous regimen-build process and many years of experience with the system,” she said.
Of the 369 total discrepancies, 41% were related to alignment with the Systemic Treatment Quality-Based Program regimen, and 32% were regimens flagged to be inactivated because of outdated information, new standards, or lack of use.
A detailed analysis of the remaining 27%, or 101 unintentional discrepancies, showed that the majority were due to missing information (35.6%) or missing drugs (13.9%), incorrect doses (10.9%), and incorrect or missing schedules (10.9%). Potential to cause harm was mild for 55%, moderate for 28%, and none for 17%.
“Corrective action has been taken to address the discrepancies identified,” said Ms. Crespo.
Only 6% of the 33 centers reported having an established regimen review and maintenance process in place before the study, but all now have such a process. In addition, some centers that did not find any regimen discrepancies nonetheless reported adding quality improvement activities, such as changes in the ways regimens were built and documented, and revising regimen names to facilitate accurate selection.
In discussing the study, Dr. Jacobson noted the low proportion of centers having an established process at baseline to ensure appropriate regimen maintenance and updates. “You might want to think to yourselves, the medical oncologists in the group, whether your center has such a process in place,” he proposed.
It is not yet known whether the project has met its goal of improving the quality and accuracy of oncology regimens in Ontario, he maintained. “We are going to have to invite [Ms. Crespo] back in a year or two to see whether that turns out to be true.” On the other hand, “clearly what they have achieved was the ability to measure the variance between what was intended and what was actually built.”
Chief among the reasons for success, again, “was a strong and effective leadership and organizational structure, not at the department level or hospital level, but across the entire province through Cancer Care Ontario,” Dr. Jacobson said. “It’s clear that they have a focus on quality and patient safety, and this measurement program that they have put in place turned out to be useful.”
Dr. Judy, Dr. Weiss, and Ms. Crespo disclosed that they had no relevant conflicts of interest.
ORLANDO – Accumulating evidence is helping researchers better understand why errors occur during the delivery of cancer treatment and how to prevent them. Findings from a trio of studies were reported at a symposium on quality care sponsored by the American Society of Clinical Oncology.
Identifying causes of incidents in radiation therapy
In the first study, Greg D. Judy, MD, a radiation oncology resident at the University of North Carolina at Chapel Hill, and his colleagues retrospectively reviewed records in their institution’s reporting system, called Good Catch, to identify near-miss incidents (ones that didn’t reach the patient) and safety incidents (ones that did) among patients undergoing radiation therapy from October 2014 through April 2016.
Multivariate analysis showed that patients had a significantly higher risk of near-miss or safety incidents if they had stage T2 disease (odds ratio, 3.3), were being treated for cancer involving the head and neck (5.2), or were receiving image-guided intensity-modulated radiation therapy (3.0) or daily imaging as part of their treatment (7.0), Dr. Judy reported.
“Head and neck site and image-guided IMRT [intensity-modulated radiation therapy] are complex entities: They have multiple steps in both the planning and delivery phase,” he said. “Daily imaging as well. It’s a much more complex process to do daily imaging for setup verification than it is to do once-a-week or even once-every-2-weeks setup verification.”
On the other hand, it was unclear why T2 stage was a risk factor. “We kind of hypothesized that it might be more of the disease site that really drives this, as you can have HPV-positive oropharyngeal cancer which usually has lower T stages and more advanced nodal stages, but even then, that’s a head and neck site and we usually use image-guided IMRT, which are both very complex entities,” he said. The most common root causes for the incidents were issues related to documentation and scheduling (29% each), followed by issues related to communication (22%), technical treatment planning (14%), and technical treatment delivery (6%).
Incidents having a communication root cause were more likely than were others to affect patients (P less than .001), and those having a technical treatment delivery root cause were more likely to have higher severity (P = .005).
“Like some other studies, we found really the key factor was the complexity of the treatment plan and complexity of the overall process that is the real driving factor. This is important to understand because it promotes the idea of developing a more dedicated and robust QA system for complex cases,” said Dr. Judy. “It also highlights the importance of a strong reporting system to support a safety culture, as well as promote the continuous learning improvements within a department.”
The national Radiation Oncology Incident Learning System (RO-ILS) has been developed by the American Society for Radiation Oncology (ASTRO). “This is gaining membership very rapidly, and it’s good because it facilitates cooperative research and also safety standards for our field,” he maintained.
“I’ll argue that they did that for a variety of reasons,” he elaborated. “Strong and effective leadership by Dr. Larry Marks, who’s really created a departmental culture of safety in which people can feel free to speak up. They have this wonderful Good Catch program in place. And they have these simulation review huddles ... where people feel free to talk about what happened yesterday or today that may be relevant moving forward.”
As for the national RO-ILS initiative, “I would look out to the audience and say, why is it that we don’t have such a program in medical oncology?” Dr. Jacobson said. “It’s probably time for us to do this,” he maintained.
Reducing chemotherapy errors in pediatric oncology
In the second study, Brian D. Weiss, MD, associate director of safety and compliance at Cincinnati Children’s Hospital Medical Center, and his colleagues studied the impact of a safety initiative to prevent chemotherapy errors at their large urban pediatric academic center (J Clin Oncol 35, 2017 [suppl 8S; abstract 37]).
“Pediatric chemotherapy protocols are different from adult protocols. We dose based on age or weight or body surface area, and that can change within a protocol. You have to do adjustments every time they gain weight or grow some, which is different than for adult protocols,” he explained. “We have parents administering chemo at home. And the protocols most patients are on are very complicated, but there is no standardized format, so it makes crucial information for dose adjustments difficult to find.”
The team successively implemented about half a dozen interventions, such as dedicated chemotherapy safety zones where staff were not to be disturbed while checking orders and ear protectors as a visual deterrent to interruptions; a new chemotherapy registered nurse role with a detailed list of responsibilities; an event-reporting system to supplement the center’s error-reporting system and capture events not reaching the patient (near-miss events); and a daily chemotherapy huddle to discuss errors in a nonpunitive setting and review upcoming chemotherapy for readiness.
In the 6 years after the start of the initiative, 105,187 chemotherapy doses were administered at the center and 998 errors occurred, including 250 errors that reached the patient, according to results reported at the symposium and recently published (J Oncol Pract. 2017 April;13:e329-e336).
At the 22-month mark, the rate of chemotherapy errors reaching the patient had fallen from 3.8 in 1,000 doses at baseline to 1.9 in 1,000 doses. The reduction has since persisted for more than 4 years and translates to an estimated 155 fewer predicted errors reaching the patient because of the initiative.
“The errors that reached the patient were more often administration and dispensing errors,” Dr. Weiss said. “About two-thirds of those errors that didn’t reach the patient – because they got caught by the pharmacists and the nurses – were prescription errors.
“Our chemotherapy huddle has certainly increased our reporting of errors. We also now use it for patients on clinical trials ... any patient getting PK [pharmacokinetics] or PD [pharmacodynamics] sampled within the next 24 hours is reviewed at that meeting. And our missed samples have gone down significantly,” he noted. “It’s allowed us to manage our bed space better because now everybody knows who’s definitely coming in the next day and who’s maybe coming in the next day.”
“We are a large urban academic pediatric medical center. Some of these things may seem difficult to translate [to smaller facilities], but I’m not sure they are,” concluded Dr. Weiss.
Dr. Jacobson, the discussant, noted that the initiative was in keeping with this health system’s longstanding “obsessive” focus on patient safety and commended its rigorousness in, for example, setting clear goals, focusing on key drivers [processes] needed for change, and selecting a good outcome metric.
“This is very successful project,” he said. The success can be attributed to “strong and effective organization and leadership, building a culture of safety at Cincinnati Children’s Hospital, and an important predefined measurement program and methodology.”
Building chemotherapy regimens more accurately
In the third study, a team led by Andrea Crespo, BSc, BScPhm, BCOP, an oncology pharmacist and member of the Systemic Treatment Team at Cancer Care Ontario, Toronto, studied errors introduced when chemotherapy regimens were moved from publications into orders used by centers in the province (J Clin Oncol. 35, 2017 [suppl 8S; abstract 51]).
Nearly all outpatient intravenous systemic treatment visits in Ontario are supported by a Systemic Treatment Computerized Prescriber Order Entry (ST-CPOE) system, she noted. Such systems can reduce error rates but are not foolproof.
She and her colleagues asked all Ontario treatment centers to review their active chemotherapy regimens. Data were analyzed to determine whether the regimens were built as intended with respect to their component drugs and doses, leading to identification of any unintentional discrepancies with the original regimen.
A total of 33 centers performed the review, and the median number of regimens reviewed was 375 per center, Ms. Crespo reported.
Unintentional discrepancies in regimens were found at 27% of centers. The total number reported was 369 discrepancies, with a range from 2 to 198 per center.
All of the nine centers where discrepancies were found participated in the provincial ST-CPOE system, and most had for at least 20 years. Furthermore, eight of them used a team of at least two pharmacists and one oncologist to build their regimens. “So you can see that discrepancies occurred despite a fairly rigorous regimen-build process and many years of experience with the system,” she said.
Of the 369 total discrepancies, 41% were related to alignment with the Systemic Treatment Quality-Based Program regimen, and 32% were regimens flagged to be inactivated because of outdated information, new standards, or lack of use.
A detailed analysis of the remaining 27%, or 101 unintentional discrepancies, showed that the majority were due to missing information (35.6%) or missing drugs (13.9%), incorrect doses (10.9%), and incorrect or missing schedules (10.9%). Potential to cause harm was mild for 55%, moderate for 28%, and none for 17%.
“Corrective action has been taken to address the discrepancies identified,” said Ms. Crespo.
Only 6% of the 33 centers reported having an established regimen review and maintenance process in place before the study, but all now have such a process. In addition, some centers that did not find any regimen discrepancies nonetheless reported adding quality improvement activities, such as changes in the ways regimens were built and documented, and revising regimen names to facilitate accurate selection.
In discussing the study, Dr. Jacobson noted the low proportion of centers having an established process at baseline to ensure appropriate regimen maintenance and updates. “You might want to think to yourselves, the medical oncologists in the group, whether your center has such a process in place,” he proposed.
It is not yet known whether the project has met its goal of improving the quality and accuracy of oncology regimens in Ontario, he maintained. “We are going to have to invite [Ms. Crespo] back in a year or two to see whether that turns out to be true.” On the other hand, “clearly what they have achieved was the ability to measure the variance between what was intended and what was actually built.”
Chief among the reasons for success, again, “was a strong and effective leadership and organizational structure, not at the department level or hospital level, but across the entire province through Cancer Care Ontario,” Dr. Jacobson said. “It’s clear that they have a focus on quality and patient safety, and this measurement program that they have put in place turned out to be useful.”
Dr. Judy, Dr. Weiss, and Ms. Crespo disclosed that they had no relevant conflicts of interest.
AT THE QUALITY CARE SYMPOSIUM
Key clinical point:
Major finding: Risk factors for radiation therapy near-miss and safety incidents were T2 stage, H&N site, and more complex techniques (odds ratios, 3.0-7.0). A quality improvement initiative halved the rate of chemotherapy errors reaching the patient from 3.8 to 1.9 per 1,000 doses. Twenty-seven percent of centers found unintentional discrepancies in their chemotherapy regimens, 83% with potential to cause harm.
Data source: A retrospective case-control study of 400 patients receiving radiation therapy, a longitudinal cohort study of a quality improvement initiative at an urban pediatric academic medical center involving administration of 105,187 chemotherapy doses, and a cohort study of 33 Ontario treatment centers that reviewed a median of 375 chemotherapy regimens.
Disclosures: Dr. Judy, Dr. Weiss, and Ms. Crespo disclosed that they had no relevant conflicts of interest.
Survivorship care models work, some better than others
ORLANDO – Accumulating experience is showing the benefits of various models of care for cancer survivors in terms of health care use and costs, while also suggesting that some provide higher-quality care than others, according to a pair of studies reported at a symposium on quality care sponsored by the American Society of Clinical Oncology.
Initiative for breast cancer survivors
“In 2011, Cancer Care Ontario did a quick environmental scan of our 14 regional cancer centers and found that the transition of breast cancer survivors from oncologists to primary care was very variable, and that centers often didn’t transition patients very frequently,” said Nicole Mittmann, PhD, first author on one of the studies, chief research officer for Cancer Care Ontario, and an investigator at Sunnybrook Research Institute, Toronto.
The advisory organization therefore implemented the Well Follow-Up Care Initiative to facilitate appropriate transition of breast cancer survivors. Each regional center was given a $100,000 incentive to roll out a model of the initiative.
Dr. Mittmann and her coinvestigators used provincial administrative databases to compare health care use and associated costs between 2,324 breast cancer survivors who were transitioned with the initiative and 2,324 propensity-matched control survivors who were not. The survivors were about 5 years out from their breast cancer diagnosis at baseline and had median follow-up of 2 years.
Study results reported at the symposium showed that the mean annual total cost of care per patient paid for by the provincial health ministry was $6,575 for the transitioned group and $10,832 for the nontransitioned group, a difference of $4,257 (39%). The main drivers were reduced costs of long-term care and cancer clinic visits.
Findings were similar for median annual costs, which amounted to $2,261 for the transitioned group and $2,903 for the control group, a difference of $638.
Compared with the nontransitioned group, the transitioned group had significantly fewer annual visits to medical oncologists (0.39 vs. 1.29) and radiation oncologists (0.16 vs. 0.36), while visits to general or family practitioners were statistically indistinguishable (7.35 and 7.91), Dr. Mittmann reported. There was also a trend toward fewer emergency department visits.
The transitioned group had fewer bone scans, CT and MRI scans, and radiographs annually, but differences were not significant.
Reassuringly, Dr. Mittmann said, survivors who were transitioned did not fare worse than their nontransitioned counterparts in overall survival; if anything, they tended to live longer. “We think that because the individual cancer centers enrolled patients that they thought were very well that this is a very well and highly selected and maybe a biased group,” Dr. Mittmann acknowledged. “But we certainly see that they are not doing worse than the control group.”
“About $1.4 million was distributed to the cancer centers” for the initiative, she noted. “That generated a savings for the health system of $1.5 million, if you are looking at median costs, to $9.9 million, if you are looking at mean costs.
“The transition of appropriate breast cancer survivors to the community appears to be safe and effective outside of a clinical trial, at least based on this particular retrospective analysis using databases,” she said. “The overall costs are not increased, and they may actually be decreased based on our data, and certainly these results will inform policy.”
The investigators plan several next steps, such as encouraging senior leadership at Cancer Care Ontario and the Ministry of Health to endorse the findings, according to Dr. Mittmann. In addition, “[we plan to] engage with both oncology and primary care leadership and think about how we can potentially roll out a program like this, and develop tools, whether those are letters or information packages, and education, to … appropriately transition individuals.”
Considerations in interpreting the study’s findings include the quality of the matching of survivors, according to invited discussant Monika K. Krzyzanowska, MD, a medical oncologist at Princess Margaret Cancer Centre, an associate professor at the University of Toronto, and a clinical lead of Quality Care and Access, Systemic Treatment Program, at Cancer Care Ontario. “The quality of that match depends on what’s in the model, so there could be potential for residual confounding, and administrative data may not have all of the elements that you would need to get a perfect match.”
Additional considerations include costs not covered by the payer, impact of the initiative on delivery of guideline-recommended care and patient and provider satisfaction, generalizability of the findings, and long-term outcomes.
“This is a proof of concept, certainly, that transition of low-risk cancer survivors to primary care is feasible and potentially economically attractive,” Dr. Krzyzanowska concluded. “It would be useful to have a formal evaluation of effectiveness that would inform a comprehensive value assessment. And we do have data from a randomized trial about the safety of this particular approach, but it would be nice to see that following implementation in real practices, those safety considerations played out the same way.”
Comparison of survivorship care models
Two-thirds of the large and growing population of cancer survivors are at least 5 years out from diagnosis, stimulating considerable discussion in the oncology community about how to best address their needs, according to Sarah Raskin, PhD, senior author on the second study and a research scientist at the Institute for Patient-Centered Initiatives and Health Equity at George Washington University Cancer Center, Washington.
“Yet, for a lack of cancer survivorship–specific guidelines from research or practice, cancer centers are increasingly developing survivorship care in a variety of ways, many of which are ad hoc or unproven as yet,” she said.
Dr. Raskin and her colleagues compared three emerging models of survivorship care: a specialized consultative model and a specialized longitudinal model – whereby patients have a single or multiple formalized survivorship visits, respectively, with care typically led by an oncology nurse-practitioner – and an oncology-embedded model – whereby survivorship is addressed as a part of ongoing oncology follow-up care, typically by the oncologist.
The investigators worked with survivors to develop the Patient-Prioritized Measure of High-Quality Survivorship Care, a 46-question scale assessing nine components of survivorship care that capture the health care priorities and needs that matter most to patients. Each component is rated on a scale from 0 (not at all met) to 1 (somewhat met) to 2 (definitely met).
Analyses were based on responses of 827 survivors of breast, colorectal, and prostate cancer who received care at 28 U.S. institutions using one of the above models and who were surveyed by telephone about the care received 1 week after their initial survivorship visit.
Results showed that survivors cared for under the three models differed significantly with respect to scores for seven of the nine components of quality of care, Dr. Raskin reported. The exceptions were practical life support, where the mean score was about 0.6-0.8 across the board, and having a medical home, where the mean score was about 1.8-1.9 across the board.
The specialized consult model of care had the highest scores for mental health and social support, information and resources, and supportive and prepared clinicians. The specialized longitudinal model of care had the highest scores for empowered and engaged patients, open patient-clinician communication, care coordination and transitions, and access to full spectrum of care. The oncology-embedded model had the lowest scores. Analysis of the tool’s 46 individual questions showed that patients cared for at institutions using the oncology-embedded model were significantly less likely than were counterparts cared for at institutions using the specialized models to report that the institution performed various activities such as offering a treatment summary, inquiring about the patient’s biggest worries or problems, and explaining the reasons why tests were needed (P less than .05 for each).
For some metrics, the overall proportion reporting that an activity was performed was low, regardless of the model being used. For example, only 48% of all patients reported being helped to set goals or make short-term plans to manage follow-up care and improve health, merely 24% reported being provided emotional and social support to deal with changes in relationships, and just 19% reported being referred to special providers for other medical problems.
“Overall, all three models are performing highly in terms of providing survivors with a medical home and communicating with patients. However, all three are performing quite low in terms of providing mental health and social support, as well as practical life support,” said Dr. Raskin.
“By model, we see that the embedded ongoing care model is significantly underperforming compared with both specialized models on seven of nine components, and we have some hypotheses from our early work with [Commission on Cancer]–accredited centers to explain this,” she added. “Embedded survivorship models have a lot of variability – many are high performers but others are low performers as compared with specialized programs. Embedded survivorship care models are typically led by the treating oncologist, who historically has focused on treating sick patients and less so on providing social supports for follow-up of well patients or ‘well-er’ patients. At the same time, specialized models focus predominantly on survivorship care and providing services and referrals for survivors, which may explain their high scores.
“We know that the higher quality of care measures presented here do not necessarily translate to better patient outcomes, and that’s actually going to be the next phase of our analysis,” she concluded.
The study sample may have had some selection bias, and it is unclear how well validated the tool was, according to Dr. Krzyzanowska, the discussant. Another issue was its assessment of quality of care at only a single time point.
Nonetheless, the findings show “that measuring quality of survivorship care from a patient perspective is feasible and valuable. We have already heard about [need for] survivorship plans in survivorship care, so certainly the work that was just presented is extremely important to help to fill some of these gaps,” she said.
“I’m not sure that we yet know what the optimal model of survivorship care is without the information of the other outcomes. Furthermore, there’s different survivor populations and different ways that health care is organized, so perhaps there isn’t really one optimal model, but the model has to fit with the context,” Dr. Krzyzanowska concluded. “That being said … the tool that they have created can be a great tool for existing survivorship care programs to assess and improve the quality of their care.”
Dr. Mittmann and Dr. Raskin had no disclosures to report.
ORLANDO – Accumulating experience is showing the benefits of various models of care for cancer survivors in terms of health care use and costs, while also suggesting that some provide higher-quality care than others, according to a pair of studies reported at a symposium on quality care sponsored by the American Society of Clinical Oncology.
Initiative for breast cancer survivors
“In 2011, Cancer Care Ontario did a quick environmental scan of our 14 regional cancer centers and found that the transition of breast cancer survivors from oncologists to primary care was very variable, and that centers often didn’t transition patients very frequently,” said Nicole Mittmann, PhD, first author on one of the studies, chief research officer for Cancer Care Ontario, and an investigator at Sunnybrook Research Institute, Toronto.
The advisory organization therefore implemented the Well Follow-Up Care Initiative to facilitate appropriate transition of breast cancer survivors. Each regional center was given a $100,000 incentive to roll out a model of the initiative.
Dr. Mittmann and her coinvestigators used provincial administrative databases to compare health care use and associated costs between 2,324 breast cancer survivors who were transitioned with the initiative and 2,324 propensity-matched control survivors who were not. The survivors were about 5 years out from their breast cancer diagnosis at baseline and had median follow-up of 2 years.
Study results reported at the symposium showed that the mean annual total cost of care per patient paid for by the provincial health ministry was $6,575 for the transitioned group and $10,832 for the nontransitioned group, a difference of $4,257 (39%). The main drivers were reduced costs of long-term care and cancer clinic visits.
Findings were similar for median annual costs, which amounted to $2,261 for the transitioned group and $2,903 for the control group, a difference of $638.
Compared with the nontransitioned group, the transitioned group had significantly fewer annual visits to medical oncologists (0.39 vs. 1.29) and radiation oncologists (0.16 vs. 0.36), while visits to general or family practitioners were statistically indistinguishable (7.35 and 7.91), Dr. Mittmann reported. There was also a trend toward fewer emergency department visits.
The transitioned group had fewer bone scans, CT and MRI scans, and radiographs annually, but differences were not significant.
Reassuringly, Dr. Mittmann said, survivors who were transitioned did not fare worse than their nontransitioned counterparts in overall survival; if anything, they tended to live longer. “We think that because the individual cancer centers enrolled patients that they thought were very well that this is a very well and highly selected and maybe a biased group,” Dr. Mittmann acknowledged. “But we certainly see that they are not doing worse than the control group.”
“About $1.4 million was distributed to the cancer centers” for the initiative, she noted. “That generated a savings for the health system of $1.5 million, if you are looking at median costs, to $9.9 million, if you are looking at mean costs.
“The transition of appropriate breast cancer survivors to the community appears to be safe and effective outside of a clinical trial, at least based on this particular retrospective analysis using databases,” she said. “The overall costs are not increased, and they may actually be decreased based on our data, and certainly these results will inform policy.”
The investigators plan several next steps, such as encouraging senior leadership at Cancer Care Ontario and the Ministry of Health to endorse the findings, according to Dr. Mittmann. In addition, “[we plan to] engage with both oncology and primary care leadership and think about how we can potentially roll out a program like this, and develop tools, whether those are letters or information packages, and education, to … appropriately transition individuals.”
Considerations in interpreting the study’s findings include the quality of the matching of survivors, according to invited discussant Monika K. Krzyzanowska, MD, a medical oncologist at Princess Margaret Cancer Centre, an associate professor at the University of Toronto, and a clinical lead of Quality Care and Access, Systemic Treatment Program, at Cancer Care Ontario. “The quality of that match depends on what’s in the model, so there could be potential for residual confounding, and administrative data may not have all of the elements that you would need to get a perfect match.”
Additional considerations include costs not covered by the payer, impact of the initiative on delivery of guideline-recommended care and patient and provider satisfaction, generalizability of the findings, and long-term outcomes.
“This is a proof of concept, certainly, that transition of low-risk cancer survivors to primary care is feasible and potentially economically attractive,” Dr. Krzyzanowska concluded. “It would be useful to have a formal evaluation of effectiveness that would inform a comprehensive value assessment. And we do have data from a randomized trial about the safety of this particular approach, but it would be nice to see that following implementation in real practices, those safety considerations played out the same way.”
Comparison of survivorship care models
Two-thirds of the large and growing population of cancer survivors are at least 5 years out from diagnosis, stimulating considerable discussion in the oncology community about how to best address their needs, according to Sarah Raskin, PhD, senior author on the second study and a research scientist at the Institute for Patient-Centered Initiatives and Health Equity at George Washington University Cancer Center, Washington.
“Yet, for a lack of cancer survivorship–specific guidelines from research or practice, cancer centers are increasingly developing survivorship care in a variety of ways, many of which are ad hoc or unproven as yet,” she said.
Dr. Raskin and her colleagues compared three emerging models of survivorship care: a specialized consultative model and a specialized longitudinal model – whereby patients have a single or multiple formalized survivorship visits, respectively, with care typically led by an oncology nurse-practitioner – and an oncology-embedded model – whereby survivorship is addressed as a part of ongoing oncology follow-up care, typically by the oncologist.
The investigators worked with survivors to develop the Patient-Prioritized Measure of High-Quality Survivorship Care, a 46-question scale assessing nine components of survivorship care that capture the health care priorities and needs that matter most to patients. Each component is rated on a scale from 0 (not at all met) to 1 (somewhat met) to 2 (definitely met).
Analyses were based on responses of 827 survivors of breast, colorectal, and prostate cancer who received care at 28 U.S. institutions using one of the above models and who were surveyed by telephone about the care received 1 week after their initial survivorship visit.
Results showed that survivors cared for under the three models differed significantly with respect to scores for seven of the nine components of quality of care, Dr. Raskin reported. The exceptions were practical life support, where the mean score was about 0.6-0.8 across the board, and having a medical home, where the mean score was about 1.8-1.9 across the board.
The specialized consult model of care had the highest scores for mental health and social support, information and resources, and supportive and prepared clinicians. The specialized longitudinal model of care had the highest scores for empowered and engaged patients, open patient-clinician communication, care coordination and transitions, and access to full spectrum of care. The oncology-embedded model had the lowest scores. Analysis of the tool’s 46 individual questions showed that patients cared for at institutions using the oncology-embedded model were significantly less likely than were counterparts cared for at institutions using the specialized models to report that the institution performed various activities such as offering a treatment summary, inquiring about the patient’s biggest worries or problems, and explaining the reasons why tests were needed (P less than .05 for each).
For some metrics, the overall proportion reporting that an activity was performed was low, regardless of the model being used. For example, only 48% of all patients reported being helped to set goals or make short-term plans to manage follow-up care and improve health, merely 24% reported being provided emotional and social support to deal with changes in relationships, and just 19% reported being referred to special providers for other medical problems.
“Overall, all three models are performing highly in terms of providing survivors with a medical home and communicating with patients. However, all three are performing quite low in terms of providing mental health and social support, as well as practical life support,” said Dr. Raskin.
“By model, we see that the embedded ongoing care model is significantly underperforming compared with both specialized models on seven of nine components, and we have some hypotheses from our early work with [Commission on Cancer]–accredited centers to explain this,” she added. “Embedded survivorship models have a lot of variability – many are high performers but others are low performers as compared with specialized programs. Embedded survivorship care models are typically led by the treating oncologist, who historically has focused on treating sick patients and less so on providing social supports for follow-up of well patients or ‘well-er’ patients. At the same time, specialized models focus predominantly on survivorship care and providing services and referrals for survivors, which may explain their high scores.
“We know that the higher quality of care measures presented here do not necessarily translate to better patient outcomes, and that’s actually going to be the next phase of our analysis,” she concluded.
The study sample may have had some selection bias, and it is unclear how well validated the tool was, according to Dr. Krzyzanowska, the discussant. Another issue was its assessment of quality of care at only a single time point.
Nonetheless, the findings show “that measuring quality of survivorship care from a patient perspective is feasible and valuable. We have already heard about [need for] survivorship plans in survivorship care, so certainly the work that was just presented is extremely important to help to fill some of these gaps,” she said.
“I’m not sure that we yet know what the optimal model of survivorship care is without the information of the other outcomes. Furthermore, there’s different survivor populations and different ways that health care is organized, so perhaps there isn’t really one optimal model, but the model has to fit with the context,” Dr. Krzyzanowska concluded. “That being said … the tool that they have created can be a great tool for existing survivorship care programs to assess and improve the quality of their care.”
Dr. Mittmann and Dr. Raskin had no disclosures to report.
ORLANDO – Accumulating experience is showing the benefits of various models of care for cancer survivors in terms of health care use and costs, while also suggesting that some provide higher-quality care than others, according to a pair of studies reported at a symposium on quality care sponsored by the American Society of Clinical Oncology.
Initiative for breast cancer survivors
“In 2011, Cancer Care Ontario did a quick environmental scan of our 14 regional cancer centers and found that the transition of breast cancer survivors from oncologists to primary care was very variable, and that centers often didn’t transition patients very frequently,” said Nicole Mittmann, PhD, first author on one of the studies, chief research officer for Cancer Care Ontario, and an investigator at Sunnybrook Research Institute, Toronto.
The advisory organization therefore implemented the Well Follow-Up Care Initiative to facilitate appropriate transition of breast cancer survivors. Each regional center was given a $100,000 incentive to roll out a model of the initiative.
Dr. Mittmann and her coinvestigators used provincial administrative databases to compare health care use and associated costs between 2,324 breast cancer survivors who were transitioned with the initiative and 2,324 propensity-matched control survivors who were not. The survivors were about 5 years out from their breast cancer diagnosis at baseline and had median follow-up of 2 years.
Study results reported at the symposium showed that the mean annual total cost of care per patient paid for by the provincial health ministry was $6,575 for the transitioned group and $10,832 for the nontransitioned group, a difference of $4,257 (39%). The main drivers were reduced costs of long-term care and cancer clinic visits.
Findings were similar for median annual costs, which amounted to $2,261 for the transitioned group and $2,903 for the control group, a difference of $638.
Compared with the nontransitioned group, the transitioned group had significantly fewer annual visits to medical oncologists (0.39 vs. 1.29) and radiation oncologists (0.16 vs. 0.36), while visits to general or family practitioners were statistically indistinguishable (7.35 and 7.91), Dr. Mittmann reported. There was also a trend toward fewer emergency department visits.
The transitioned group had fewer bone scans, CT and MRI scans, and radiographs annually, but differences were not significant.
Reassuringly, Dr. Mittmann said, survivors who were transitioned did not fare worse than their nontransitioned counterparts in overall survival; if anything, they tended to live longer. “We think that because the individual cancer centers enrolled patients that they thought were very well that this is a very well and highly selected and maybe a biased group,” Dr. Mittmann acknowledged. “But we certainly see that they are not doing worse than the control group.”
“About $1.4 million was distributed to the cancer centers” for the initiative, she noted. “That generated a savings for the health system of $1.5 million, if you are looking at median costs, to $9.9 million, if you are looking at mean costs.
“The transition of appropriate breast cancer survivors to the community appears to be safe and effective outside of a clinical trial, at least based on this particular retrospective analysis using databases,” she said. “The overall costs are not increased, and they may actually be decreased based on our data, and certainly these results will inform policy.”
The investigators plan several next steps, such as encouraging senior leadership at Cancer Care Ontario and the Ministry of Health to endorse the findings, according to Dr. Mittmann. In addition, “[we plan to] engage with both oncology and primary care leadership and think about how we can potentially roll out a program like this, and develop tools, whether those are letters or information packages, and education, to … appropriately transition individuals.”
Considerations in interpreting the study’s findings include the quality of the matching of survivors, according to invited discussant Monika K. Krzyzanowska, MD, a medical oncologist at Princess Margaret Cancer Centre, an associate professor at the University of Toronto, and a clinical lead of Quality Care and Access, Systemic Treatment Program, at Cancer Care Ontario. “The quality of that match depends on what’s in the model, so there could be potential for residual confounding, and administrative data may not have all of the elements that you would need to get a perfect match.”
Additional considerations include costs not covered by the payer, impact of the initiative on delivery of guideline-recommended care and patient and provider satisfaction, generalizability of the findings, and long-term outcomes.
“This is a proof of concept, certainly, that transition of low-risk cancer survivors to primary care is feasible and potentially economically attractive,” Dr. Krzyzanowska concluded. “It would be useful to have a formal evaluation of effectiveness that would inform a comprehensive value assessment. And we do have data from a randomized trial about the safety of this particular approach, but it would be nice to see that following implementation in real practices, those safety considerations played out the same way.”
Comparison of survivorship care models
Two-thirds of the large and growing population of cancer survivors are at least 5 years out from diagnosis, stimulating considerable discussion in the oncology community about how to best address their needs, according to Sarah Raskin, PhD, senior author on the second study and a research scientist at the Institute for Patient-Centered Initiatives and Health Equity at George Washington University Cancer Center, Washington.
“Yet, for a lack of cancer survivorship–specific guidelines from research or practice, cancer centers are increasingly developing survivorship care in a variety of ways, many of which are ad hoc or unproven as yet,” she said.
Dr. Raskin and her colleagues compared three emerging models of survivorship care: a specialized consultative model and a specialized longitudinal model – whereby patients have a single or multiple formalized survivorship visits, respectively, with care typically led by an oncology nurse-practitioner – and an oncology-embedded model – whereby survivorship is addressed as a part of ongoing oncology follow-up care, typically by the oncologist.
The investigators worked with survivors to develop the Patient-Prioritized Measure of High-Quality Survivorship Care, a 46-question scale assessing nine components of survivorship care that capture the health care priorities and needs that matter most to patients. Each component is rated on a scale from 0 (not at all met) to 1 (somewhat met) to 2 (definitely met).
Analyses were based on responses of 827 survivors of breast, colorectal, and prostate cancer who received care at 28 U.S. institutions using one of the above models and who were surveyed by telephone about the care received 1 week after their initial survivorship visit.
Results showed that survivors cared for under the three models differed significantly with respect to scores for seven of the nine components of quality of care, Dr. Raskin reported. The exceptions were practical life support, where the mean score was about 0.6-0.8 across the board, and having a medical home, where the mean score was about 1.8-1.9 across the board.
The specialized consult model of care had the highest scores for mental health and social support, information and resources, and supportive and prepared clinicians. The specialized longitudinal model of care had the highest scores for empowered and engaged patients, open patient-clinician communication, care coordination and transitions, and access to full spectrum of care. The oncology-embedded model had the lowest scores. Analysis of the tool’s 46 individual questions showed that patients cared for at institutions using the oncology-embedded model were significantly less likely than were counterparts cared for at institutions using the specialized models to report that the institution performed various activities such as offering a treatment summary, inquiring about the patient’s biggest worries or problems, and explaining the reasons why tests were needed (P less than .05 for each).
For some metrics, the overall proportion reporting that an activity was performed was low, regardless of the model being used. For example, only 48% of all patients reported being helped to set goals or make short-term plans to manage follow-up care and improve health, merely 24% reported being provided emotional and social support to deal with changes in relationships, and just 19% reported being referred to special providers for other medical problems.
“Overall, all three models are performing highly in terms of providing survivors with a medical home and communicating with patients. However, all three are performing quite low in terms of providing mental health and social support, as well as practical life support,” said Dr. Raskin.
“By model, we see that the embedded ongoing care model is significantly underperforming compared with both specialized models on seven of nine components, and we have some hypotheses from our early work with [Commission on Cancer]–accredited centers to explain this,” she added. “Embedded survivorship models have a lot of variability – many are high performers but others are low performers as compared with specialized programs. Embedded survivorship care models are typically led by the treating oncologist, who historically has focused on treating sick patients and less so on providing social supports for follow-up of well patients or ‘well-er’ patients. At the same time, specialized models focus predominantly on survivorship care and providing services and referrals for survivors, which may explain their high scores.
“We know that the higher quality of care measures presented here do not necessarily translate to better patient outcomes, and that’s actually going to be the next phase of our analysis,” she concluded.
The study sample may have had some selection bias, and it is unclear how well validated the tool was, according to Dr. Krzyzanowska, the discussant. Another issue was its assessment of quality of care at only a single time point.
Nonetheless, the findings show “that measuring quality of survivorship care from a patient perspective is feasible and valuable. We have already heard about [need for] survivorship plans in survivorship care, so certainly the work that was just presented is extremely important to help to fill some of these gaps,” she said.
“I’m not sure that we yet know what the optimal model of survivorship care is without the information of the other outcomes. Furthermore, there’s different survivor populations and different ways that health care is organized, so perhaps there isn’t really one optimal model, but the model has to fit with the context,” Dr. Krzyzanowska concluded. “That being said … the tool that they have created can be a great tool for existing survivorship care programs to assess and improve the quality of their care.”
Dr. Mittmann and Dr. Raskin had no disclosures to report.
AT THE QUALITY CARE SYMPOSIUM
Key clinical point:
Major finding: Mean annual health care costs were $4,257 (39%) lower for breast cancer survivors actively transitioned to primary care versus control peers. Specialized consult and specialized longitudinal models outperformed an oncology-embedded model on seven quality metrics.
Data source: A cohort study of 2,324 breast cancer survivors transitioned to primary care and 2,324 not transitioned. A cohort study of 827 survivors of breast, colorectal, and prostate cancer receiving care under three differing models.
Disclosures: Dr. Mittmann and Dr. Raskin had no disclosures to report.
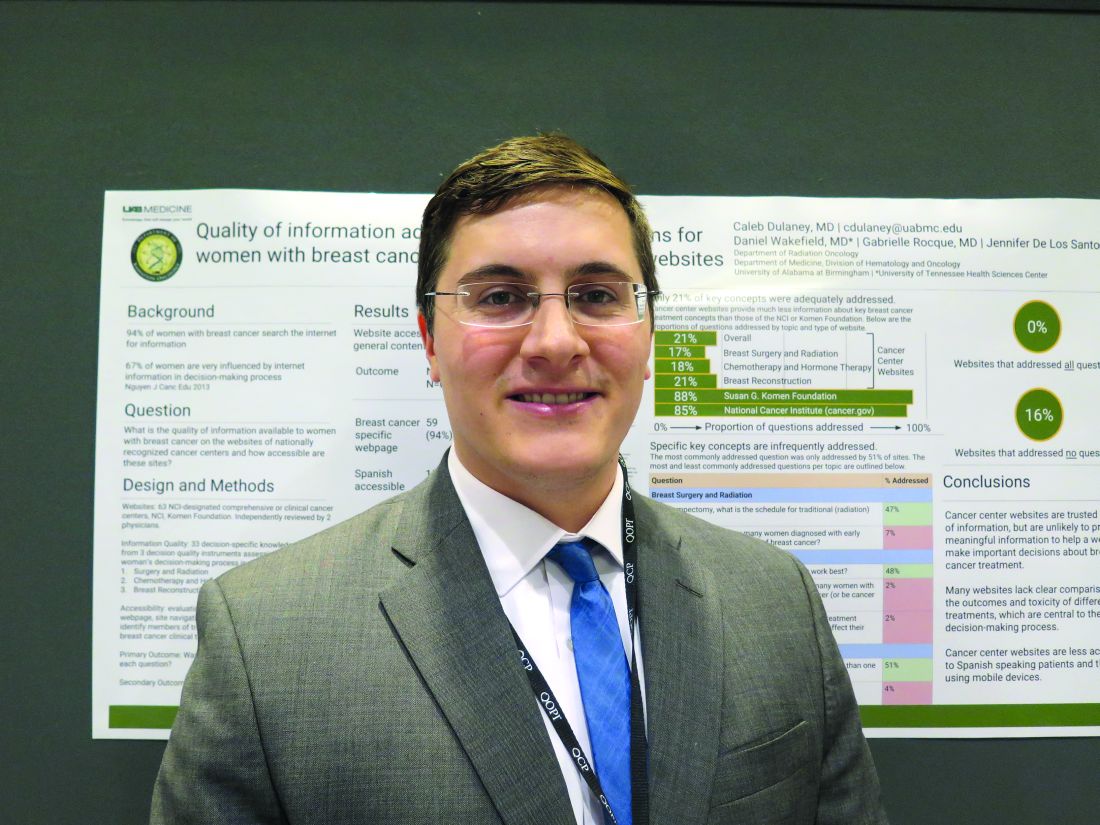
Breast cancer info on centers’ sites leaves room for improvement
ORLANDO – Women with breast cancer who look for well-rounded information about treatment on the websites of prominent U.S. cancer centers are likely to come up short, suggests a study presented at a symposium on quality care sponsored by the American Society of Clinical Oncology.
Research has shown that nearly all women with breast cancer search the Internet for information about its treatment, and two-thirds report that what they find has a strong influence on their decision-making process (J Cancer Educ. 2013;28[4]:662-8).
But the analysis of content on the websites of 63 National Cancer Institute–designated comprehensive cancer centers or clinical cancer centers found that, on average, they addressed only 21% of a set of key concepts that women need to understand to make informed decisions about surgery, radiation therapy, chemotherapy, hormone therapy, and breast reconstruction. This contrasted starkly with 85% for the National Cancer Institute’s own website (cancer.gov) and 88% for the Susan G. Komen Foundation’s website (komen.org).
“These are websites that we think are reliable, cancer center websites, and these are the most prominent cancer centers in the country,” first author Caleb Dulaney, MD, a resident in radiation oncology at the University of Alabama at Birmingham, said in an interview. “This is where a lot of people receive their care, so they should be very reliable as to the information they provide.
“A lot of websites just had information from the NCI basically integrated into their website or a link to the NCI website,” he acknowledged. “Is it really the goal of the cancer center’s website to provide information? It may not be. But you have to take responsibility for being a trusted source of information. So if you are not going to provide it, you should at least direct people to very accurate, reliable information, and it can also kind of inform what you talk about in clinic.”
All of the investigators evaluating sites in the study were medical professionals, so the team has initiated a new study in which patients will instead perform the evaluations.
“We found that for a few websites, one person found a lot of information and another found no information. So the information may technically be there, but is it transmitted to the patient? Can they find it, and do they understand it?” Dr. Dulaney said. “So it will be interesting when we use patients to evaluate these websites. I’ll be curious to see how many questions they are able to find answers to.”
Study details
For the study, the investigators developed a list of 33 decision-specific knowledge questions about breast cancer treatment by drawing on decision quality instruments that assess how informed a woman’s decision-making process is. The primary outcome was whether the website provided sufficient information to answer each question. The researchers assessed seven measures of accessibility as secondary outcomes.
Results showed that websites contained sufficient content to address only 21% of the decision-specific knowledge questions, Dr. Dulaney reported in a poster session. The value was 17% for questions pertaining to breast surgery and radiation therapy, 18% for those pertaining to chemotherapy and hormone therapy, and 21% for those pertaining to breast reconstruction.
In addition, “a lot of websites put the information in silos,” he noted. “You can read about mastectomy, you can read about lumpectomy, you can read about chemo. But you can’t really get the big picture, which is how do these compare to each other, and which treatment is best for me.”
Even the most commonly addressed single question – what type of reconstruction is most likely to require more than one surgery or procedure – was addressed by only 51% of sites. Proportions were similar for questions pertaining to the type of tumors against which hormone therapy works best (48%) and the schedule for radiation therapy after lumpectomy (47%).
At the other extreme, however, very small proportions of sites addressed questions pertaining to how many women with treated early breast cancer will die from the disease (7%), how many undergoing breast reconstruction will experience complications requiring hospitalization or an unplanned procedure (4%), how skipping chemotherapy and hormone therapy influences risk of death (2%), and whether waiting several weeks to decide about those therapies affects survival (2%). These topics are more negative, Dr. Dulaney observed, “but these are things women need to know.”
None of the websites provided sufficient information to answer all 33 knowledge questions. But perhaps more worrisome, 16% did not provide sufficient information to answer any of them, he said.
When it came to accessibility of information, 94% of sites clearly had a breast cancer–specific page, 87% had information about breast cancer–specific trials, and 86% showed members of the center’s breast cancer team. But only 59% were mobile device friendly as assessed with a Google tool, and merely 24% had obvious links to view information in Spanish.
“A lot of minorities and people of lower socioeconomic status exclusively access the Internet via mobile devices, so they may not have a computer or [other] access to the Internet. But they have a cell phone that is probably a smartphone, and they can get online and search for information that way,” Dr. Dulaney said.
Many oncologists may not have had any say regarding the content and accessibility features of their institution’s website, he acknowledged.
“So we should maybe, number one, try to have more involvement in what information goes on to the website, and two, take a look at our own websites to see what’s on there, because patients are going to look for you, and they are going to associate this information with you,” he said. “If you are at a big institution and you really can’t make a change on your website, you can use alternatives such as social media platforms, things like that, to try and get information out to people.”
From a larger perspective, oncologists have often simply counseled patients that they can’t rely on information they have found online, according to Dr. Dulaney.
“But in this day and age, that can’t really be an answer,” he concluded. “Information on the web is ubiquitous, and there is good information out there. We need to do a better job of speaking up in the conversation. We have the answers to a lot of these questions, we just need to make our voices heard and also direct patients to reliable sources of information.”
ORLANDO – Women with breast cancer who look for well-rounded information about treatment on the websites of prominent U.S. cancer centers are likely to come up short, suggests a study presented at a symposium on quality care sponsored by the American Society of Clinical Oncology.
Research has shown that nearly all women with breast cancer search the Internet for information about its treatment, and two-thirds report that what they find has a strong influence on their decision-making process (J Cancer Educ. 2013;28[4]:662-8).
But the analysis of content on the websites of 63 National Cancer Institute–designated comprehensive cancer centers or clinical cancer centers found that, on average, they addressed only 21% of a set of key concepts that women need to understand to make informed decisions about surgery, radiation therapy, chemotherapy, hormone therapy, and breast reconstruction. This contrasted starkly with 85% for the National Cancer Institute’s own website (cancer.gov) and 88% for the Susan G. Komen Foundation’s website (komen.org).
“These are websites that we think are reliable, cancer center websites, and these are the most prominent cancer centers in the country,” first author Caleb Dulaney, MD, a resident in radiation oncology at the University of Alabama at Birmingham, said in an interview. “This is where a lot of people receive their care, so they should be very reliable as to the information they provide.
“A lot of websites just had information from the NCI basically integrated into their website or a link to the NCI website,” he acknowledged. “Is it really the goal of the cancer center’s website to provide information? It may not be. But you have to take responsibility for being a trusted source of information. So if you are not going to provide it, you should at least direct people to very accurate, reliable information, and it can also kind of inform what you talk about in clinic.”
All of the investigators evaluating sites in the study were medical professionals, so the team has initiated a new study in which patients will instead perform the evaluations.
“We found that for a few websites, one person found a lot of information and another found no information. So the information may technically be there, but is it transmitted to the patient? Can they find it, and do they understand it?” Dr. Dulaney said. “So it will be interesting when we use patients to evaluate these websites. I’ll be curious to see how many questions they are able to find answers to.”
Study details
For the study, the investigators developed a list of 33 decision-specific knowledge questions about breast cancer treatment by drawing on decision quality instruments that assess how informed a woman’s decision-making process is. The primary outcome was whether the website provided sufficient information to answer each question. The researchers assessed seven measures of accessibility as secondary outcomes.
Results showed that websites contained sufficient content to address only 21% of the decision-specific knowledge questions, Dr. Dulaney reported in a poster session. The value was 17% for questions pertaining to breast surgery and radiation therapy, 18% for those pertaining to chemotherapy and hormone therapy, and 21% for those pertaining to breast reconstruction.
In addition, “a lot of websites put the information in silos,” he noted. “You can read about mastectomy, you can read about lumpectomy, you can read about chemo. But you can’t really get the big picture, which is how do these compare to each other, and which treatment is best for me.”
Even the most commonly addressed single question – what type of reconstruction is most likely to require more than one surgery or procedure – was addressed by only 51% of sites. Proportions were similar for questions pertaining to the type of tumors against which hormone therapy works best (48%) and the schedule for radiation therapy after lumpectomy (47%).
At the other extreme, however, very small proportions of sites addressed questions pertaining to how many women with treated early breast cancer will die from the disease (7%), how many undergoing breast reconstruction will experience complications requiring hospitalization or an unplanned procedure (4%), how skipping chemotherapy and hormone therapy influences risk of death (2%), and whether waiting several weeks to decide about those therapies affects survival (2%). These topics are more negative, Dr. Dulaney observed, “but these are things women need to know.”
None of the websites provided sufficient information to answer all 33 knowledge questions. But perhaps more worrisome, 16% did not provide sufficient information to answer any of them, he said.
When it came to accessibility of information, 94% of sites clearly had a breast cancer–specific page, 87% had information about breast cancer–specific trials, and 86% showed members of the center’s breast cancer team. But only 59% were mobile device friendly as assessed with a Google tool, and merely 24% had obvious links to view information in Spanish.
“A lot of minorities and people of lower socioeconomic status exclusively access the Internet via mobile devices, so they may not have a computer or [other] access to the Internet. But they have a cell phone that is probably a smartphone, and they can get online and search for information that way,” Dr. Dulaney said.
Many oncologists may not have had any say regarding the content and accessibility features of their institution’s website, he acknowledged.
“So we should maybe, number one, try to have more involvement in what information goes on to the website, and two, take a look at our own websites to see what’s on there, because patients are going to look for you, and they are going to associate this information with you,” he said. “If you are at a big institution and you really can’t make a change on your website, you can use alternatives such as social media platforms, things like that, to try and get information out to people.”
From a larger perspective, oncologists have often simply counseled patients that they can’t rely on information they have found online, according to Dr. Dulaney.
“But in this day and age, that can’t really be an answer,” he concluded. “Information on the web is ubiquitous, and there is good information out there. We need to do a better job of speaking up in the conversation. We have the answers to a lot of these questions, we just need to make our voices heard and also direct patients to reliable sources of information.”
ORLANDO – Women with breast cancer who look for well-rounded information about treatment on the websites of prominent U.S. cancer centers are likely to come up short, suggests a study presented at a symposium on quality care sponsored by the American Society of Clinical Oncology.
Research has shown that nearly all women with breast cancer search the Internet for information about its treatment, and two-thirds report that what they find has a strong influence on their decision-making process (J Cancer Educ. 2013;28[4]:662-8).
But the analysis of content on the websites of 63 National Cancer Institute–designated comprehensive cancer centers or clinical cancer centers found that, on average, they addressed only 21% of a set of key concepts that women need to understand to make informed decisions about surgery, radiation therapy, chemotherapy, hormone therapy, and breast reconstruction. This contrasted starkly with 85% for the National Cancer Institute’s own website (cancer.gov) and 88% for the Susan G. Komen Foundation’s website (komen.org).
“These are websites that we think are reliable, cancer center websites, and these are the most prominent cancer centers in the country,” first author Caleb Dulaney, MD, a resident in radiation oncology at the University of Alabama at Birmingham, said in an interview. “This is where a lot of people receive their care, so they should be very reliable as to the information they provide.
“A lot of websites just had information from the NCI basically integrated into their website or a link to the NCI website,” he acknowledged. “Is it really the goal of the cancer center’s website to provide information? It may not be. But you have to take responsibility for being a trusted source of information. So if you are not going to provide it, you should at least direct people to very accurate, reliable information, and it can also kind of inform what you talk about in clinic.”
All of the investigators evaluating sites in the study were medical professionals, so the team has initiated a new study in which patients will instead perform the evaluations.
“We found that for a few websites, one person found a lot of information and another found no information. So the information may technically be there, but is it transmitted to the patient? Can they find it, and do they understand it?” Dr. Dulaney said. “So it will be interesting when we use patients to evaluate these websites. I’ll be curious to see how many questions they are able to find answers to.”
Study details
For the study, the investigators developed a list of 33 decision-specific knowledge questions about breast cancer treatment by drawing on decision quality instruments that assess how informed a woman’s decision-making process is. The primary outcome was whether the website provided sufficient information to answer each question. The researchers assessed seven measures of accessibility as secondary outcomes.
Results showed that websites contained sufficient content to address only 21% of the decision-specific knowledge questions, Dr. Dulaney reported in a poster session. The value was 17% for questions pertaining to breast surgery and radiation therapy, 18% for those pertaining to chemotherapy and hormone therapy, and 21% for those pertaining to breast reconstruction.
In addition, “a lot of websites put the information in silos,” he noted. “You can read about mastectomy, you can read about lumpectomy, you can read about chemo. But you can’t really get the big picture, which is how do these compare to each other, and which treatment is best for me.”
Even the most commonly addressed single question – what type of reconstruction is most likely to require more than one surgery or procedure – was addressed by only 51% of sites. Proportions were similar for questions pertaining to the type of tumors against which hormone therapy works best (48%) and the schedule for radiation therapy after lumpectomy (47%).
At the other extreme, however, very small proportions of sites addressed questions pertaining to how many women with treated early breast cancer will die from the disease (7%), how many undergoing breast reconstruction will experience complications requiring hospitalization or an unplanned procedure (4%), how skipping chemotherapy and hormone therapy influences risk of death (2%), and whether waiting several weeks to decide about those therapies affects survival (2%). These topics are more negative, Dr. Dulaney observed, “but these are things women need to know.”
None of the websites provided sufficient information to answer all 33 knowledge questions. But perhaps more worrisome, 16% did not provide sufficient information to answer any of them, he said.
When it came to accessibility of information, 94% of sites clearly had a breast cancer–specific page, 87% had information about breast cancer–specific trials, and 86% showed members of the center’s breast cancer team. But only 59% were mobile device friendly as assessed with a Google tool, and merely 24% had obvious links to view information in Spanish.
“A lot of minorities and people of lower socioeconomic status exclusively access the Internet via mobile devices, so they may not have a computer or [other] access to the Internet. But they have a cell phone that is probably a smartphone, and they can get online and search for information that way,” Dr. Dulaney said.
Many oncologists may not have had any say regarding the content and accessibility features of their institution’s website, he acknowledged.
“So we should maybe, number one, try to have more involvement in what information goes on to the website, and two, take a look at our own websites to see what’s on there, because patients are going to look for you, and they are going to associate this information with you,” he said. “If you are at a big institution and you really can’t make a change on your website, you can use alternatives such as social media platforms, things like that, to try and get information out to people.”
From a larger perspective, oncologists have often simply counseled patients that they can’t rely on information they have found online, according to Dr. Dulaney.
“But in this day and age, that can’t really be an answer,” he concluded. “Information on the web is ubiquitous, and there is good information out there. We need to do a better job of speaking up in the conversation. We have the answers to a lot of these questions, we just need to make our voices heard and also direct patients to reliable sources of information.”
AT THE QUALITY CARE SYMPOSIUM
Key clinical point:
Major finding: On average, the sites addressed 21% of 33 key concepts needed to make informed decisions about treatment.
Data source: An analysis of breast cancer information on the websites of 63 NCI-designated comprehensive cancer centers or clinical cancer centers.
Disclosures: Dr. Dulaney disclosed that he had no relevant conflicts of interest.
Real-world EGFR and ALK testing of NSCLC falls short
ORLANDO – A large proportion of patients with advanced non–small cell lung cancer (NSCLC) are not being tested for tumor associated–epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK) alterations according to national guidelines. This situation may be leading to suboptimal treatment, a large retrospective cohort study suggests.
Guidelines from the American Society of Clinical Oncology and the National Comprehensive Cancer Network recommend testing before first-line therapy for all treatment-eligible patients with nonsquamous histology and for those patients with squamous histology who are nonsmokers or who have mixed cell types or small tumor samples. Additionally, the guidelines recommend that results be made available within 2 weeks of the lab’s receipt of the sample so that they can be used to inform treatment decisions.
Overall, 22% of patients with nonsquamous tumors had no evidence of EGFR and ALK testing in their records. The large majority of patients with squamous tumors did not have any evidence of testing either, and it was unclear how well testing corresponded with the criteria.
In roughly a third of cases in which testing was done, the time between diagnosis of advanced disease and availability of test results exceeded 4 weeks. Among patients with positive test results, those whose results came back after the start of first-line therapy, were about half as likely to appropriately receive a therapy that targeted their tumor’s molecular aberration.
“We observed variation in adherence to [the American Society of Clinical Oncology] and [the National Comprehensive Cancer Network] guidelines around biomarker testing in advanced NSCLC, and we saw significant variation in testing in the squamous population and the nonsquamous population across practices,” presenting author Jay Rughani, manager of Life Sciences at Flatiron Health, New York, commented in an interview. Observed delays in availability of test results were mainly driven by delays between diagnosis and submission of samples to the lab for testing.
“There may be an opportunity to educate the oncology community around testing, certainly for all nonsquamous patients, because this is a case where they all should have been tested,” he said. “And there is also an opportunity to ensure testing of the appropriate squamous cell patients, while discouraging the testing of the majority who aren’t candidates, so there may be an opportunity for education around smoking status.”
Slow uptake of the national guidelines is unlikely to explain the observed variations in testing, according to Mr. Rughani. “Since we looked at patients diagnosed after Jan. 1, 2014, our impression was that the guidelines were sort of disseminated enough and widely known enough by that point, particularly around EGFR and ALK, that we wouldn’t expect any lag there. If we had done this for PD-L1 [programmed death ligand 1] testing, perhaps we might have thought about some lag in adoption.”
The impact of variations in testing and receipt of inappropriate initial therapy on clinical outcomes is yet to be determined. “As a follow-on, some of the work we have been doing is trying to understand, for these separate cohorts of patients, depending on what they received in the front line, what their overall survival was and what their surrogate endpoints were,” Mr. Rughani concluded.
Study details
For the study, the investigators identified 16,316 patients with advanced NSCLC from 206 community clinics across the United States participating in the Flatiron Network. All patients were treated between 2014 and 2016.
Cross-checking of the total Flatiron population against the National Program of Cancer Registries and Surveillance, Epidemiology, and End Results databases suggested that it is a good national representation, according to Mr. Rughani.
A record review showed that the rate of EGFR and ALK testing among study patients ranged widely across clinics, from 0% to 100% for both the nonsquamous cases and the squamous cases, according to results reported in a poster session. The median was 79% for the former and 16% for the latter.
Overall, 22% of the nonsquamous cohort and 79% of the squamous cohort did not have any evidence of testing in their records. For the latter, a sampling of records was unable to verify whether testing was appropriately matched to eligibility criteria.
When testing was performed, 35% of EGFR test results and 37% of ALK test results were not available to the treating clinician until more than 4 weeks after the date of the advanced cancer diagnosis.
“The delays were mostly attributed to nonlab factors. When we isolated the time that the lab took to turn it around, it was under 2 weeks for the vast majority of patients,” Mr. Rughani reported. Possible nonlab culprit factors include clinic work flows, insurance-related issues, and families’ and patients’ hesitancy to be tested, he said.
Delays in receipt of positive test results appeared to influence choice of first-line therapy. Among patients in whom these results were available before first-line therapy, 80% of those found to have an EGFR-mutated tumor received an EGFR–tyrosine kinase inhibitor, and 77% of those found to have ALK-rearranged tumors received an ALK inhibitor.
In sharp contrast, among patients in whom positive test results did not become available until after the start of first-line therapy, respective values were just 43% and 42%.
“Anecdotally, we saw that some patients would go on to Avastin [bevacizumab] in the front line when the results were delayed, and then, ultimately, they would have the opportunity to receive an EGFR[–tyrosine kinase inhibitor] or something like that in later lines,” commented Mr. Rughani. “So, that impacted treatment decisions there.”
Mr. Rughani disclosed stock and other ownership interests in Flatiron Health.
ORLANDO – A large proportion of patients with advanced non–small cell lung cancer (NSCLC) are not being tested for tumor associated–epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK) alterations according to national guidelines. This situation may be leading to suboptimal treatment, a large retrospective cohort study suggests.
Guidelines from the American Society of Clinical Oncology and the National Comprehensive Cancer Network recommend testing before first-line therapy for all treatment-eligible patients with nonsquamous histology and for those patients with squamous histology who are nonsmokers or who have mixed cell types or small tumor samples. Additionally, the guidelines recommend that results be made available within 2 weeks of the lab’s receipt of the sample so that they can be used to inform treatment decisions.
Overall, 22% of patients with nonsquamous tumors had no evidence of EGFR and ALK testing in their records. The large majority of patients with squamous tumors did not have any evidence of testing either, and it was unclear how well testing corresponded with the criteria.
In roughly a third of cases in which testing was done, the time between diagnosis of advanced disease and availability of test results exceeded 4 weeks. Among patients with positive test results, those whose results came back after the start of first-line therapy, were about half as likely to appropriately receive a therapy that targeted their tumor’s molecular aberration.
“We observed variation in adherence to [the American Society of Clinical Oncology] and [the National Comprehensive Cancer Network] guidelines around biomarker testing in advanced NSCLC, and we saw significant variation in testing in the squamous population and the nonsquamous population across practices,” presenting author Jay Rughani, manager of Life Sciences at Flatiron Health, New York, commented in an interview. Observed delays in availability of test results were mainly driven by delays between diagnosis and submission of samples to the lab for testing.
“There may be an opportunity to educate the oncology community around testing, certainly for all nonsquamous patients, because this is a case where they all should have been tested,” he said. “And there is also an opportunity to ensure testing of the appropriate squamous cell patients, while discouraging the testing of the majority who aren’t candidates, so there may be an opportunity for education around smoking status.”
Slow uptake of the national guidelines is unlikely to explain the observed variations in testing, according to Mr. Rughani. “Since we looked at patients diagnosed after Jan. 1, 2014, our impression was that the guidelines were sort of disseminated enough and widely known enough by that point, particularly around EGFR and ALK, that we wouldn’t expect any lag there. If we had done this for PD-L1 [programmed death ligand 1] testing, perhaps we might have thought about some lag in adoption.”
The impact of variations in testing and receipt of inappropriate initial therapy on clinical outcomes is yet to be determined. “As a follow-on, some of the work we have been doing is trying to understand, for these separate cohorts of patients, depending on what they received in the front line, what their overall survival was and what their surrogate endpoints were,” Mr. Rughani concluded.
Study details
For the study, the investigators identified 16,316 patients with advanced NSCLC from 206 community clinics across the United States participating in the Flatiron Network. All patients were treated between 2014 and 2016.
Cross-checking of the total Flatiron population against the National Program of Cancer Registries and Surveillance, Epidemiology, and End Results databases suggested that it is a good national representation, according to Mr. Rughani.
A record review showed that the rate of EGFR and ALK testing among study patients ranged widely across clinics, from 0% to 100% for both the nonsquamous cases and the squamous cases, according to results reported in a poster session. The median was 79% for the former and 16% for the latter.
Overall, 22% of the nonsquamous cohort and 79% of the squamous cohort did not have any evidence of testing in their records. For the latter, a sampling of records was unable to verify whether testing was appropriately matched to eligibility criteria.
When testing was performed, 35% of EGFR test results and 37% of ALK test results were not available to the treating clinician until more than 4 weeks after the date of the advanced cancer diagnosis.
“The delays were mostly attributed to nonlab factors. When we isolated the time that the lab took to turn it around, it was under 2 weeks for the vast majority of patients,” Mr. Rughani reported. Possible nonlab culprit factors include clinic work flows, insurance-related issues, and families’ and patients’ hesitancy to be tested, he said.
Delays in receipt of positive test results appeared to influence choice of first-line therapy. Among patients in whom these results were available before first-line therapy, 80% of those found to have an EGFR-mutated tumor received an EGFR–tyrosine kinase inhibitor, and 77% of those found to have ALK-rearranged tumors received an ALK inhibitor.
In sharp contrast, among patients in whom positive test results did not become available until after the start of first-line therapy, respective values were just 43% and 42%.
“Anecdotally, we saw that some patients would go on to Avastin [bevacizumab] in the front line when the results were delayed, and then, ultimately, they would have the opportunity to receive an EGFR[–tyrosine kinase inhibitor] or something like that in later lines,” commented Mr. Rughani. “So, that impacted treatment decisions there.”
Mr. Rughani disclosed stock and other ownership interests in Flatiron Health.
ORLANDO – A large proportion of patients with advanced non–small cell lung cancer (NSCLC) are not being tested for tumor associated–epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK) alterations according to national guidelines. This situation may be leading to suboptimal treatment, a large retrospective cohort study suggests.
Guidelines from the American Society of Clinical Oncology and the National Comprehensive Cancer Network recommend testing before first-line therapy for all treatment-eligible patients with nonsquamous histology and for those patients with squamous histology who are nonsmokers or who have mixed cell types or small tumor samples. Additionally, the guidelines recommend that results be made available within 2 weeks of the lab’s receipt of the sample so that they can be used to inform treatment decisions.
Overall, 22% of patients with nonsquamous tumors had no evidence of EGFR and ALK testing in their records. The large majority of patients with squamous tumors did not have any evidence of testing either, and it was unclear how well testing corresponded with the criteria.
In roughly a third of cases in which testing was done, the time between diagnosis of advanced disease and availability of test results exceeded 4 weeks. Among patients with positive test results, those whose results came back after the start of first-line therapy, were about half as likely to appropriately receive a therapy that targeted their tumor’s molecular aberration.
“We observed variation in adherence to [the American Society of Clinical Oncology] and [the National Comprehensive Cancer Network] guidelines around biomarker testing in advanced NSCLC, and we saw significant variation in testing in the squamous population and the nonsquamous population across practices,” presenting author Jay Rughani, manager of Life Sciences at Flatiron Health, New York, commented in an interview. Observed delays in availability of test results were mainly driven by delays between diagnosis and submission of samples to the lab for testing.
“There may be an opportunity to educate the oncology community around testing, certainly for all nonsquamous patients, because this is a case where they all should have been tested,” he said. “And there is also an opportunity to ensure testing of the appropriate squamous cell patients, while discouraging the testing of the majority who aren’t candidates, so there may be an opportunity for education around smoking status.”
Slow uptake of the national guidelines is unlikely to explain the observed variations in testing, according to Mr. Rughani. “Since we looked at patients diagnosed after Jan. 1, 2014, our impression was that the guidelines were sort of disseminated enough and widely known enough by that point, particularly around EGFR and ALK, that we wouldn’t expect any lag there. If we had done this for PD-L1 [programmed death ligand 1] testing, perhaps we might have thought about some lag in adoption.”
The impact of variations in testing and receipt of inappropriate initial therapy on clinical outcomes is yet to be determined. “As a follow-on, some of the work we have been doing is trying to understand, for these separate cohorts of patients, depending on what they received in the front line, what their overall survival was and what their surrogate endpoints were,” Mr. Rughani concluded.
Study details
For the study, the investigators identified 16,316 patients with advanced NSCLC from 206 community clinics across the United States participating in the Flatiron Network. All patients were treated between 2014 and 2016.
Cross-checking of the total Flatiron population against the National Program of Cancer Registries and Surveillance, Epidemiology, and End Results databases suggested that it is a good national representation, according to Mr. Rughani.
A record review showed that the rate of EGFR and ALK testing among study patients ranged widely across clinics, from 0% to 100% for both the nonsquamous cases and the squamous cases, according to results reported in a poster session. The median was 79% for the former and 16% for the latter.
Overall, 22% of the nonsquamous cohort and 79% of the squamous cohort did not have any evidence of testing in their records. For the latter, a sampling of records was unable to verify whether testing was appropriately matched to eligibility criteria.
When testing was performed, 35% of EGFR test results and 37% of ALK test results were not available to the treating clinician until more than 4 weeks after the date of the advanced cancer diagnosis.
“The delays were mostly attributed to nonlab factors. When we isolated the time that the lab took to turn it around, it was under 2 weeks for the vast majority of patients,” Mr. Rughani reported. Possible nonlab culprit factors include clinic work flows, insurance-related issues, and families’ and patients’ hesitancy to be tested, he said.
Delays in receipt of positive test results appeared to influence choice of first-line therapy. Among patients in whom these results were available before first-line therapy, 80% of those found to have an EGFR-mutated tumor received an EGFR–tyrosine kinase inhibitor, and 77% of those found to have ALK-rearranged tumors received an ALK inhibitor.
In sharp contrast, among patients in whom positive test results did not become available until after the start of first-line therapy, respective values were just 43% and 42%.
“Anecdotally, we saw that some patients would go on to Avastin [bevacizumab] in the front line when the results were delayed, and then, ultimately, they would have the opportunity to receive an EGFR[–tyrosine kinase inhibitor] or something like that in later lines,” commented Mr. Rughani. “So, that impacted treatment decisions there.”
Mr. Rughani disclosed stock and other ownership interests in Flatiron Health.
Key clinical point:
Major finding: Overall, 22% of patients with nonsquamous advanced NSCLC had no evidence of EGFR and ALK tumor testing in their records.
Data source: A retrospective cohort study of 16,316 community oncology patients with advanced NSCLC.
Disclosures: Mr. Rughani disclosed that he is an employee of and has stock or other ownership interests in Flatiron Health.
Portfolio of physician-led measures nets better quality of care
ORLANDO – A multifaceted portfolio of physician-led measures with feedback and financial incentives can dramatically improve the quality of care provided at cancer centers, suggests the experience of Stanford (Calif.) Health Care.
Physician leaders of 13 disease-specific cancer care programs (CCPs) identified measures of care that were meaningful to their team and patients, spanning the spectrum from new diagnosis through end of life and survivorship care. Quality and analytics teams developed 16 corresponding metrics and performance reports used for feedback. Programs were also given a financial incentive to meet jointly set targets.
After a year, the CCPs had improved on 12 of the metrics and maintained high baseline levels of performance on the other 4 metrics, investigators reported at a symposium on quality care sponsored by the American Society of Clinical Oncology. For example, they got better at entering staging information in a dedicated field in the electronic health record (+50% absolute increase), recording hand and foot pain (+34%), performing hepatitis B testing before rituximab use (+17%), and referring patients with ovarian cancer for genetic counseling (+43%).
“The main drivers, I would argue, besides the Hawthorne effect, were a high level of physician engagement in the selection, management, and improvement of the metrics, and these metrics excited the care teams, which also provided some motivation,” she said. “We provided real-time, high-quality feedback of performance. And last but probably not least was a financial incentive for the CCP as a team, not part of any individual compensation.”
The investigators plan to continue measuring the metrics, to expand them to other sites in their network, and to add new metrics that are common across the programs to minimize measurement burden, according to Ms. Porter. “We also plan to build cohorts for value-based care and unplanned care like ED visits and unplanned admissions. Finally, we want to keep momentum going and capitalize upon a provider engagement in value measurement and improvement,” she said.
“Based on this work and prior abstracts, … there are many validated metrics to be used. So, to choose those metrics and to choose them through local leadership support, most importantly, engaging frontline staff and having their buy-in of the measures that you are collecting are important,” commented invited discussant Jessica A. Zerillo, MD, MPH, of the Beth Israel Deaconess Medical Center in Boston. “And this can include using incentives that drive such stakeholders, whether they be financial or simply pride with public reporting.”
Study details
“In the summer of 2015, we were starting to feel a lot of pressure to prepare for evolving reimbursement models,” Ms. Porter said, explaining the initiative’s genesis. “Mainly, how do we define our value, and how can we measure and improve on that value of the care we deliver? One answer, of course, is to measure and reduce unnecessary variation. And we knew, to be successful, we had to increase our physician engagement and leadership in the selection and improvement of our metrics.”
Physician leaders of the CCPs were asked to choose quality measures that met three criteria: they were meaningful and important to both the care team and patients, they had pertinent data elements already available in existing databases (to reduce documentation burden), and they were multidisciplinary in nature, reflecting the care provided by the whole program. The measures ultimately selected included a variety of those put forth by American Society of Clinical Oncology’s Quality Oncology Practice Initiative and the American Society for Radiation Oncology. CCPs were offered a financial incentive for meeting targets ranging from $75,000 to $125,000 that was based on number of providers and patient volume, rather than on the impact of improved metric. “This was really meant for reinvestment back into their quality programs,” Ms. Porter said. “I would argue this was really a culture-building year for us, and we hope that next year there might be a little bit more tangible value with the metrics.”
The quality team gave CCPs monthly or quarterly performance reports with unblinded physician- and patient-level details that were ultimately disseminated to all the other CCPs. They also investigated any missing data for individual metrics.
Study results showed that half of the 16 measures the physician leaders chose pertained to the diagnosis and treatment planning phase of care, according to Ms. Porter. “It was important to many of our CCPs to ensure that specific testing was done, which would then, in turn, drive treatment planning decisions,” she commented.
At the end of the year, each metric was assessed among 13 to 2,406 patients. “All CCPs met their predetermined target and earned their financial incentive award for the year,” Ms. Porter reported.
Improvement was most marked, with a 50% absolute increase, for the metric of completing a staging module, which required conversion of staging information (historically embedded in progress notes) into a structured format in a dedicated field in the electronic health record within 45 days of a patient’s first cancer treatment. This practice enables ready identification of stage cohorts in which value of care can be assessed, she noted.
There were also sizable absolute increases in relevant CCPs in the proportion of blood and marrow transplant recipients referred to survivorship care by day 100 (+20%) and visiting that service by day 180 (+13%), recording of hand and foot pain (+34%) and radiation dermatitis (+21%), mismatch repair testing in patients with newly diagnosed colorectal cancer (+10%), referral of patients with newly diagnosed ovarian cancer for genetic counseling (+43%), cytogenetic testing in patients with newly diagnosed hematologic malignancies (+17%), hepatitis B testing before rituximab administration (+17%), and allowance of at least 2 nights for treatment plan physics–quality assurance before the start of a nonemergent radiation oncology treatment (+14%).
Meanwhile, there were decreases, considered favorable changes, in chemotherapy use in the last 2 weeks of life among neuro-oncology patients (–9%) and in patients’ receipt of more than 10 fractions of radiation therapy for palliation of bone metastases (–9%).
Finally, there was no change in several metrics of quality that were already at very high or low levels, as appropriate, at baseline: molecular testing in patients with newly diagnosed acute myeloid leukemia (stable at 95%), hospice enrollment at the time of death for neuro-oncology patients (stable at 100%), chemotherapy in the last 2 weeks of life for patients with sarcoma (stable at 0%), and epidermal growth factor receptor testing in patients with newly diagnosed lung adenocarcinoma (stable at 98%).
ORLANDO – A multifaceted portfolio of physician-led measures with feedback and financial incentives can dramatically improve the quality of care provided at cancer centers, suggests the experience of Stanford (Calif.) Health Care.
Physician leaders of 13 disease-specific cancer care programs (CCPs) identified measures of care that were meaningful to their team and patients, spanning the spectrum from new diagnosis through end of life and survivorship care. Quality and analytics teams developed 16 corresponding metrics and performance reports used for feedback. Programs were also given a financial incentive to meet jointly set targets.
After a year, the CCPs had improved on 12 of the metrics and maintained high baseline levels of performance on the other 4 metrics, investigators reported at a symposium on quality care sponsored by the American Society of Clinical Oncology. For example, they got better at entering staging information in a dedicated field in the electronic health record (+50% absolute increase), recording hand and foot pain (+34%), performing hepatitis B testing before rituximab use (+17%), and referring patients with ovarian cancer for genetic counseling (+43%).
“The main drivers, I would argue, besides the Hawthorne effect, were a high level of physician engagement in the selection, management, and improvement of the metrics, and these metrics excited the care teams, which also provided some motivation,” she said. “We provided real-time, high-quality feedback of performance. And last but probably not least was a financial incentive for the CCP as a team, not part of any individual compensation.”
The investigators plan to continue measuring the metrics, to expand them to other sites in their network, and to add new metrics that are common across the programs to minimize measurement burden, according to Ms. Porter. “We also plan to build cohorts for value-based care and unplanned care like ED visits and unplanned admissions. Finally, we want to keep momentum going and capitalize upon a provider engagement in value measurement and improvement,” she said.
“Based on this work and prior abstracts, … there are many validated metrics to be used. So, to choose those metrics and to choose them through local leadership support, most importantly, engaging frontline staff and having their buy-in of the measures that you are collecting are important,” commented invited discussant Jessica A. Zerillo, MD, MPH, of the Beth Israel Deaconess Medical Center in Boston. “And this can include using incentives that drive such stakeholders, whether they be financial or simply pride with public reporting.”
Study details
“In the summer of 2015, we were starting to feel a lot of pressure to prepare for evolving reimbursement models,” Ms. Porter said, explaining the initiative’s genesis. “Mainly, how do we define our value, and how can we measure and improve on that value of the care we deliver? One answer, of course, is to measure and reduce unnecessary variation. And we knew, to be successful, we had to increase our physician engagement and leadership in the selection and improvement of our metrics.”
Physician leaders of the CCPs were asked to choose quality measures that met three criteria: they were meaningful and important to both the care team and patients, they had pertinent data elements already available in existing databases (to reduce documentation burden), and they were multidisciplinary in nature, reflecting the care provided by the whole program. The measures ultimately selected included a variety of those put forth by American Society of Clinical Oncology’s Quality Oncology Practice Initiative and the American Society for Radiation Oncology. CCPs were offered a financial incentive for meeting targets ranging from $75,000 to $125,000 that was based on number of providers and patient volume, rather than on the impact of improved metric. “This was really meant for reinvestment back into their quality programs,” Ms. Porter said. “I would argue this was really a culture-building year for us, and we hope that next year there might be a little bit more tangible value with the metrics.”
The quality team gave CCPs monthly or quarterly performance reports with unblinded physician- and patient-level details that were ultimately disseminated to all the other CCPs. They also investigated any missing data for individual metrics.
Study results showed that half of the 16 measures the physician leaders chose pertained to the diagnosis and treatment planning phase of care, according to Ms. Porter. “It was important to many of our CCPs to ensure that specific testing was done, which would then, in turn, drive treatment planning decisions,” she commented.
At the end of the year, each metric was assessed among 13 to 2,406 patients. “All CCPs met their predetermined target and earned their financial incentive award for the year,” Ms. Porter reported.
Improvement was most marked, with a 50% absolute increase, for the metric of completing a staging module, which required conversion of staging information (historically embedded in progress notes) into a structured format in a dedicated field in the electronic health record within 45 days of a patient’s first cancer treatment. This practice enables ready identification of stage cohorts in which value of care can be assessed, she noted.
There were also sizable absolute increases in relevant CCPs in the proportion of blood and marrow transplant recipients referred to survivorship care by day 100 (+20%) and visiting that service by day 180 (+13%), recording of hand and foot pain (+34%) and radiation dermatitis (+21%), mismatch repair testing in patients with newly diagnosed colorectal cancer (+10%), referral of patients with newly diagnosed ovarian cancer for genetic counseling (+43%), cytogenetic testing in patients with newly diagnosed hematologic malignancies (+17%), hepatitis B testing before rituximab administration (+17%), and allowance of at least 2 nights for treatment plan physics–quality assurance before the start of a nonemergent radiation oncology treatment (+14%).
Meanwhile, there were decreases, considered favorable changes, in chemotherapy use in the last 2 weeks of life among neuro-oncology patients (–9%) and in patients’ receipt of more than 10 fractions of radiation therapy for palliation of bone metastases (–9%).
Finally, there was no change in several metrics of quality that were already at very high or low levels, as appropriate, at baseline: molecular testing in patients with newly diagnosed acute myeloid leukemia (stable at 95%), hospice enrollment at the time of death for neuro-oncology patients (stable at 100%), chemotherapy in the last 2 weeks of life for patients with sarcoma (stable at 0%), and epidermal growth factor receptor testing in patients with newly diagnosed lung adenocarcinoma (stable at 98%).
ORLANDO – A multifaceted portfolio of physician-led measures with feedback and financial incentives can dramatically improve the quality of care provided at cancer centers, suggests the experience of Stanford (Calif.) Health Care.
Physician leaders of 13 disease-specific cancer care programs (CCPs) identified measures of care that were meaningful to their team and patients, spanning the spectrum from new diagnosis through end of life and survivorship care. Quality and analytics teams developed 16 corresponding metrics and performance reports used for feedback. Programs were also given a financial incentive to meet jointly set targets.
After a year, the CCPs had improved on 12 of the metrics and maintained high baseline levels of performance on the other 4 metrics, investigators reported at a symposium on quality care sponsored by the American Society of Clinical Oncology. For example, they got better at entering staging information in a dedicated field in the electronic health record (+50% absolute increase), recording hand and foot pain (+34%), performing hepatitis B testing before rituximab use (+17%), and referring patients with ovarian cancer for genetic counseling (+43%).
“The main drivers, I would argue, besides the Hawthorne effect, were a high level of physician engagement in the selection, management, and improvement of the metrics, and these metrics excited the care teams, which also provided some motivation,” she said. “We provided real-time, high-quality feedback of performance. And last but probably not least was a financial incentive for the CCP as a team, not part of any individual compensation.”
The investigators plan to continue measuring the metrics, to expand them to other sites in their network, and to add new metrics that are common across the programs to minimize measurement burden, according to Ms. Porter. “We also plan to build cohorts for value-based care and unplanned care like ED visits and unplanned admissions. Finally, we want to keep momentum going and capitalize upon a provider engagement in value measurement and improvement,” she said.
“Based on this work and prior abstracts, … there are many validated metrics to be used. So, to choose those metrics and to choose them through local leadership support, most importantly, engaging frontline staff and having their buy-in of the measures that you are collecting are important,” commented invited discussant Jessica A. Zerillo, MD, MPH, of the Beth Israel Deaconess Medical Center in Boston. “And this can include using incentives that drive such stakeholders, whether they be financial or simply pride with public reporting.”
Study details
“In the summer of 2015, we were starting to feel a lot of pressure to prepare for evolving reimbursement models,” Ms. Porter said, explaining the initiative’s genesis. “Mainly, how do we define our value, and how can we measure and improve on that value of the care we deliver? One answer, of course, is to measure and reduce unnecessary variation. And we knew, to be successful, we had to increase our physician engagement and leadership in the selection and improvement of our metrics.”
Physician leaders of the CCPs were asked to choose quality measures that met three criteria: they were meaningful and important to both the care team and patients, they had pertinent data elements already available in existing databases (to reduce documentation burden), and they were multidisciplinary in nature, reflecting the care provided by the whole program. The measures ultimately selected included a variety of those put forth by American Society of Clinical Oncology’s Quality Oncology Practice Initiative and the American Society for Radiation Oncology. CCPs were offered a financial incentive for meeting targets ranging from $75,000 to $125,000 that was based on number of providers and patient volume, rather than on the impact of improved metric. “This was really meant for reinvestment back into their quality programs,” Ms. Porter said. “I would argue this was really a culture-building year for us, and we hope that next year there might be a little bit more tangible value with the metrics.”
The quality team gave CCPs monthly or quarterly performance reports with unblinded physician- and patient-level details that were ultimately disseminated to all the other CCPs. They also investigated any missing data for individual metrics.
Study results showed that half of the 16 measures the physician leaders chose pertained to the diagnosis and treatment planning phase of care, according to Ms. Porter. “It was important to many of our CCPs to ensure that specific testing was done, which would then, in turn, drive treatment planning decisions,” she commented.
At the end of the year, each metric was assessed among 13 to 2,406 patients. “All CCPs met their predetermined target and earned their financial incentive award for the year,” Ms. Porter reported.
Improvement was most marked, with a 50% absolute increase, for the metric of completing a staging module, which required conversion of staging information (historically embedded in progress notes) into a structured format in a dedicated field in the electronic health record within 45 days of a patient’s first cancer treatment. This practice enables ready identification of stage cohorts in which value of care can be assessed, she noted.
There were also sizable absolute increases in relevant CCPs in the proportion of blood and marrow transplant recipients referred to survivorship care by day 100 (+20%) and visiting that service by day 180 (+13%), recording of hand and foot pain (+34%) and radiation dermatitis (+21%), mismatch repair testing in patients with newly diagnosed colorectal cancer (+10%), referral of patients with newly diagnosed ovarian cancer for genetic counseling (+43%), cytogenetic testing in patients with newly diagnosed hematologic malignancies (+17%), hepatitis B testing before rituximab administration (+17%), and allowance of at least 2 nights for treatment plan physics–quality assurance before the start of a nonemergent radiation oncology treatment (+14%).
Meanwhile, there were decreases, considered favorable changes, in chemotherapy use in the last 2 weeks of life among neuro-oncology patients (–9%) and in patients’ receipt of more than 10 fractions of radiation therapy for palliation of bone metastases (–9%).
Finally, there was no change in several metrics of quality that were already at very high or low levels, as appropriate, at baseline: molecular testing in patients with newly diagnosed acute myeloid leukemia (stable at 95%), hospice enrollment at the time of death for neuro-oncology patients (stable at 100%), chemotherapy in the last 2 weeks of life for patients with sarcoma (stable at 0%), and epidermal growth factor receptor testing in patients with newly diagnosed lung adenocarcinoma (stable at 98%).
AT THE QUALITY CARE SYMPOSIUM
Key clinical point:
Major finding: Over a 1-year period, the center saw improvements in practices such as completion of staging modules (+50%), recording of hand and foot pain (+34%), hepatitis B testing before rituximab use (+17%), and referral of patients with ovarian cancer for genetic counseling (+43%).
Data source: An initiative targeting 16 quality metrics undertaken by 13 cancer care programs at Stanford Health Care.
Disclosures: Ms. Porter disclosed that she had no relevant conflicts of interest.
Decision support tool appears to safely reduce CSF use
ORLANDO – A decision support tool safely reduces use of colony-stimulating factors (CSFs) in patients undergoing chemotherapy for lung cancer, suggests a retrospective claims-based cohort study of nearly 3,500 patients across the country.
The rate of CSF use fell among patients treated in the nine states that implemented the tool – a library of chemotherapy regimens and their expected FN risk that uses preauthorization and an algorithm to promote risk-appropriate, guideline-adherent use – but it remained unchanged in the 39 states and the District of Columbia, where usual practice continued, investigators reported at a symposium on quality care sponsored by the American Society of Clinical Oncology and simultaneously published (J Oncol Pract. 2017 March 4. doi: 10.1200/JOP.2017.020867). The adjusted difference was nearly 9%.
“Decision support programs like the one highlighted here could be one way, definitely not the only way, of achieving guideline-adherent CSF use and reducing practice variation across the country,” commented coinvestigator Abiy Agiro, PhD, associate director of payer and provider research at HealthCore, a subsidiary of Anthem, in Wilmington, Delaware.
“Such efforts could also have unintended consequences, so it’s important to study relevant patient outcomes,” he added. “In this case, although it appears that the incidence of febrile neutropenia rising does not seem to relate with the program, the study does not establish the safety of CSF use reduction in lung cancer patients receiving chemotherapy. So, we should take the results with that caveat.”
Parsing the findings
Although the United States makes up just 4% of the world’s population, it uses nearly 80% of CSFs sold by a leading manufacturer, according to invited discussant Thomas J. Smith, MD, a professor of oncology and palliative medicine at Johns Hopkins University in Baltimore.
“When we rewrote the ASCO [American Society of Clinical Oncology] guidelines on CSF use in 2015, there were some specific indications: dose-intense chemo for adjuvant breast cancer and uroepithelial cancer and ... when the risk of febrile neutropenia is about 20% and dose reduction is not an appropriate strategy. We were quick to point out that most regimens have a risk of febrile neutropenia much less than that,” he noted.
Dr. Agiro and his colleagues’ findings are valid, real, and reproducible, Dr. Smith maintained. However, it is unclear to what extent the observed levels of CSF use represented overuse.
“In lung cancer, there are very few regimens that have a febrile neutropenia rate close to 20%,” he elaborated. “What we don’t know is how much of this [use] was actually justified. I would suspect it is 10% or 15%, rather than 40%.”
CSF use, as guided by the new tool, “might not support increased dose density [of chemotherapy], but I would challenge anybody in the audience to show me data in normal solid tumor patients that [show that] dose density maintained by CSFs makes a difference in overall survival,” he said.
Questions yet to be addressed include the difficulty and cost of using the decision support tool and the possible negative impact on practices’ finances, according to Dr. Smith.
“When ESAs [erythropoiesis-stimulating agents] came off being used so much, some of my friends’ practices took a 15% to 20% drop in their revenue, and this is an important source of revenue for a lot of practices,” he explained. “So, I hope that when we take this revenue away, that we are cognizant of that and realize that it’s just another stress on practices, many of which are under significant stress already.”
Study details
An estimated 26% of uses of CSFs in patients with lung cancer are not in accordance with the ASCO practice guidelines, according to Dr. Agiro. “Such variations from recommendations are sometimes the reason why different stakeholders take actions” to improve care, such as ASCO’s Quality Oncology Practice Initiative (QOPI) and the American Board of Internal Medicine’s Choosing Wisely initiative (J Oncol Pract. 2015;11:338-43).
The decision support tool evaluated in the study uses preauthorization before delivery of care and, therefore, differs from point-of-care interventions, he noted.
“The tool allows access to a library of chemotherapy regimens and their associated, expected febrile neutropenia risk based on the myelotoxicity of the planned regimens as indicated in published trials. The tool is accessible online and provides real-time recommendations that are tailored based on disease- and patient-specific factors for either the use of CSF or not,” he elaborated.
According to the tool’s algorithm, use is recommended for patients who are given a regimen with a high risk of febrile neutropenia (greater than 20%) and is not recommended for those given a low-risk regimen (less than 10%). It is tailored according to the presence of additional risk factors for the intermediate-risk group.
Oncologists use the tool only for patients starting a new chemotherapy and only in the first cycle, when the risk of febrile neutropenia is highest, according to Dr. Agiro. “Once the approval is given in the first cycle, it remains in effect for the next 6 months, so they don’t have to use it again and again in additional cycles,” he explained.
The decision support tool was implemented in nine states starting in July 2014. In the study, which was funded by Anthem, the investigators analyzed administrative claims data from commercially insured adult patients starting chemotherapy for lung cancer, assessing changes in outcomes between a preimplementation period (April 2013 to Dec. 2013) and a postimplementation period (July 2014 to March 2015).
Analyses were based on 1,857 patients in the states that implemented the tool and 1,610 patients in the states that did not.
The percentage of patients receiving CSFs in the 6 months after starting chemotherapy fell in states that implemented the decision support tool (from 48.4% to 35.6%) but remained stable in states that did not (43.2% and 44.4%), Dr. Agiro reported. The adjusted difference in differences was –8.7% (P less than .001).
Meanwhile, the percentage of patients admitted for febrile neutropenia or experiencing this outcome while hospitalized increased in both states implementing the tool (from 2.8% to 4.3%) and those not implementing it (from 3.1% to 5.1%). Although the magnitude of increase was smaller in the former (+1.5% vs. +2.0%), the difference was not significant. Findings were essentially the same among the subset of patients aged 65 years and older.
“It’s important to study both intended and unintended consequences of such interventions,” Dr. Agiro noted. “Our study goes beyond financial considerations by looking at unintended outcomes: in this case, focusing on the incidence of febrile neutropenia, an outcome that is of prime interest to patients and oncologists and payers alike.”
The study may have missed some cases of febrile neutropenia, he acknowledged. “Also, there are other important outcomes of concern. For example, were there any delays in chemotherapy administration or immune recovery that could have been triggered by the implementation of the decision support program?”
The impact, both intended and unintended, on practices warrants evaluation as well, he further noted. “An important question could be, ‘Does it take less time to use this decision support tool compared to the time taken with normal care processes?’ ”
Dr. Agiro disclosed that he is employed by, has stock or other ownership interests in, and receives research funding from Anthem.
ORLANDO – A decision support tool safely reduces use of colony-stimulating factors (CSFs) in patients undergoing chemotherapy for lung cancer, suggests a retrospective claims-based cohort study of nearly 3,500 patients across the country.
The rate of CSF use fell among patients treated in the nine states that implemented the tool – a library of chemotherapy regimens and their expected FN risk that uses preauthorization and an algorithm to promote risk-appropriate, guideline-adherent use – but it remained unchanged in the 39 states and the District of Columbia, where usual practice continued, investigators reported at a symposium on quality care sponsored by the American Society of Clinical Oncology and simultaneously published (J Oncol Pract. 2017 March 4. doi: 10.1200/JOP.2017.020867). The adjusted difference was nearly 9%.
“Decision support programs like the one highlighted here could be one way, definitely not the only way, of achieving guideline-adherent CSF use and reducing practice variation across the country,” commented coinvestigator Abiy Agiro, PhD, associate director of payer and provider research at HealthCore, a subsidiary of Anthem, in Wilmington, Delaware.
“Such efforts could also have unintended consequences, so it’s important to study relevant patient outcomes,” he added. “In this case, although it appears that the incidence of febrile neutropenia rising does not seem to relate with the program, the study does not establish the safety of CSF use reduction in lung cancer patients receiving chemotherapy. So, we should take the results with that caveat.”
Parsing the findings
Although the United States makes up just 4% of the world’s population, it uses nearly 80% of CSFs sold by a leading manufacturer, according to invited discussant Thomas J. Smith, MD, a professor of oncology and palliative medicine at Johns Hopkins University in Baltimore.
“When we rewrote the ASCO [American Society of Clinical Oncology] guidelines on CSF use in 2015, there were some specific indications: dose-intense chemo for adjuvant breast cancer and uroepithelial cancer and ... when the risk of febrile neutropenia is about 20% and dose reduction is not an appropriate strategy. We were quick to point out that most regimens have a risk of febrile neutropenia much less than that,” he noted.
Dr. Agiro and his colleagues’ findings are valid, real, and reproducible, Dr. Smith maintained. However, it is unclear to what extent the observed levels of CSF use represented overuse.
“In lung cancer, there are very few regimens that have a febrile neutropenia rate close to 20%,” he elaborated. “What we don’t know is how much of this [use] was actually justified. I would suspect it is 10% or 15%, rather than 40%.”
CSF use, as guided by the new tool, “might not support increased dose density [of chemotherapy], but I would challenge anybody in the audience to show me data in normal solid tumor patients that [show that] dose density maintained by CSFs makes a difference in overall survival,” he said.
Questions yet to be addressed include the difficulty and cost of using the decision support tool and the possible negative impact on practices’ finances, according to Dr. Smith.
“When ESAs [erythropoiesis-stimulating agents] came off being used so much, some of my friends’ practices took a 15% to 20% drop in their revenue, and this is an important source of revenue for a lot of practices,” he explained. “So, I hope that when we take this revenue away, that we are cognizant of that and realize that it’s just another stress on practices, many of which are under significant stress already.”
Study details
An estimated 26% of uses of CSFs in patients with lung cancer are not in accordance with the ASCO practice guidelines, according to Dr. Agiro. “Such variations from recommendations are sometimes the reason why different stakeholders take actions” to improve care, such as ASCO’s Quality Oncology Practice Initiative (QOPI) and the American Board of Internal Medicine’s Choosing Wisely initiative (J Oncol Pract. 2015;11:338-43).
The decision support tool evaluated in the study uses preauthorization before delivery of care and, therefore, differs from point-of-care interventions, he noted.
“The tool allows access to a library of chemotherapy regimens and their associated, expected febrile neutropenia risk based on the myelotoxicity of the planned regimens as indicated in published trials. The tool is accessible online and provides real-time recommendations that are tailored based on disease- and patient-specific factors for either the use of CSF or not,” he elaborated.
According to the tool’s algorithm, use is recommended for patients who are given a regimen with a high risk of febrile neutropenia (greater than 20%) and is not recommended for those given a low-risk regimen (less than 10%). It is tailored according to the presence of additional risk factors for the intermediate-risk group.
Oncologists use the tool only for patients starting a new chemotherapy and only in the first cycle, when the risk of febrile neutropenia is highest, according to Dr. Agiro. “Once the approval is given in the first cycle, it remains in effect for the next 6 months, so they don’t have to use it again and again in additional cycles,” he explained.
The decision support tool was implemented in nine states starting in July 2014. In the study, which was funded by Anthem, the investigators analyzed administrative claims data from commercially insured adult patients starting chemotherapy for lung cancer, assessing changes in outcomes between a preimplementation period (April 2013 to Dec. 2013) and a postimplementation period (July 2014 to March 2015).
Analyses were based on 1,857 patients in the states that implemented the tool and 1,610 patients in the states that did not.
The percentage of patients receiving CSFs in the 6 months after starting chemotherapy fell in states that implemented the decision support tool (from 48.4% to 35.6%) but remained stable in states that did not (43.2% and 44.4%), Dr. Agiro reported. The adjusted difference in differences was –8.7% (P less than .001).
Meanwhile, the percentage of patients admitted for febrile neutropenia or experiencing this outcome while hospitalized increased in both states implementing the tool (from 2.8% to 4.3%) and those not implementing it (from 3.1% to 5.1%). Although the magnitude of increase was smaller in the former (+1.5% vs. +2.0%), the difference was not significant. Findings were essentially the same among the subset of patients aged 65 years and older.
“It’s important to study both intended and unintended consequences of such interventions,” Dr. Agiro noted. “Our study goes beyond financial considerations by looking at unintended outcomes: in this case, focusing on the incidence of febrile neutropenia, an outcome that is of prime interest to patients and oncologists and payers alike.”
The study may have missed some cases of febrile neutropenia, he acknowledged. “Also, there are other important outcomes of concern. For example, were there any delays in chemotherapy administration or immune recovery that could have been triggered by the implementation of the decision support program?”
The impact, both intended and unintended, on practices warrants evaluation as well, he further noted. “An important question could be, ‘Does it take less time to use this decision support tool compared to the time taken with normal care processes?’ ”
Dr. Agiro disclosed that he is employed by, has stock or other ownership interests in, and receives research funding from Anthem.
ORLANDO – A decision support tool safely reduces use of colony-stimulating factors (CSFs) in patients undergoing chemotherapy for lung cancer, suggests a retrospective claims-based cohort study of nearly 3,500 patients across the country.
The rate of CSF use fell among patients treated in the nine states that implemented the tool – a library of chemotherapy regimens and their expected FN risk that uses preauthorization and an algorithm to promote risk-appropriate, guideline-adherent use – but it remained unchanged in the 39 states and the District of Columbia, where usual practice continued, investigators reported at a symposium on quality care sponsored by the American Society of Clinical Oncology and simultaneously published (J Oncol Pract. 2017 March 4. doi: 10.1200/JOP.2017.020867). The adjusted difference was nearly 9%.
“Decision support programs like the one highlighted here could be one way, definitely not the only way, of achieving guideline-adherent CSF use and reducing practice variation across the country,” commented coinvestigator Abiy Agiro, PhD, associate director of payer and provider research at HealthCore, a subsidiary of Anthem, in Wilmington, Delaware.
“Such efforts could also have unintended consequences, so it’s important to study relevant patient outcomes,” he added. “In this case, although it appears that the incidence of febrile neutropenia rising does not seem to relate with the program, the study does not establish the safety of CSF use reduction in lung cancer patients receiving chemotherapy. So, we should take the results with that caveat.”
Parsing the findings
Although the United States makes up just 4% of the world’s population, it uses nearly 80% of CSFs sold by a leading manufacturer, according to invited discussant Thomas J. Smith, MD, a professor of oncology and palliative medicine at Johns Hopkins University in Baltimore.
“When we rewrote the ASCO [American Society of Clinical Oncology] guidelines on CSF use in 2015, there were some specific indications: dose-intense chemo for adjuvant breast cancer and uroepithelial cancer and ... when the risk of febrile neutropenia is about 20% and dose reduction is not an appropriate strategy. We were quick to point out that most regimens have a risk of febrile neutropenia much less than that,” he noted.
Dr. Agiro and his colleagues’ findings are valid, real, and reproducible, Dr. Smith maintained. However, it is unclear to what extent the observed levels of CSF use represented overuse.
“In lung cancer, there are very few regimens that have a febrile neutropenia rate close to 20%,” he elaborated. “What we don’t know is how much of this [use] was actually justified. I would suspect it is 10% or 15%, rather than 40%.”
CSF use, as guided by the new tool, “might not support increased dose density [of chemotherapy], but I would challenge anybody in the audience to show me data in normal solid tumor patients that [show that] dose density maintained by CSFs makes a difference in overall survival,” he said.
Questions yet to be addressed include the difficulty and cost of using the decision support tool and the possible negative impact on practices’ finances, according to Dr. Smith.
“When ESAs [erythropoiesis-stimulating agents] came off being used so much, some of my friends’ practices took a 15% to 20% drop in their revenue, and this is an important source of revenue for a lot of practices,” he explained. “So, I hope that when we take this revenue away, that we are cognizant of that and realize that it’s just another stress on practices, many of which are under significant stress already.”
Study details
An estimated 26% of uses of CSFs in patients with lung cancer are not in accordance with the ASCO practice guidelines, according to Dr. Agiro. “Such variations from recommendations are sometimes the reason why different stakeholders take actions” to improve care, such as ASCO’s Quality Oncology Practice Initiative (QOPI) and the American Board of Internal Medicine’s Choosing Wisely initiative (J Oncol Pract. 2015;11:338-43).
The decision support tool evaluated in the study uses preauthorization before delivery of care and, therefore, differs from point-of-care interventions, he noted.
“The tool allows access to a library of chemotherapy regimens and their associated, expected febrile neutropenia risk based on the myelotoxicity of the planned regimens as indicated in published trials. The tool is accessible online and provides real-time recommendations that are tailored based on disease- and patient-specific factors for either the use of CSF or not,” he elaborated.
According to the tool’s algorithm, use is recommended for patients who are given a regimen with a high risk of febrile neutropenia (greater than 20%) and is not recommended for those given a low-risk regimen (less than 10%). It is tailored according to the presence of additional risk factors for the intermediate-risk group.
Oncologists use the tool only for patients starting a new chemotherapy and only in the first cycle, when the risk of febrile neutropenia is highest, according to Dr. Agiro. “Once the approval is given in the first cycle, it remains in effect for the next 6 months, so they don’t have to use it again and again in additional cycles,” he explained.
The decision support tool was implemented in nine states starting in July 2014. In the study, which was funded by Anthem, the investigators analyzed administrative claims data from commercially insured adult patients starting chemotherapy for lung cancer, assessing changes in outcomes between a preimplementation period (April 2013 to Dec. 2013) and a postimplementation period (July 2014 to March 2015).
Analyses were based on 1,857 patients in the states that implemented the tool and 1,610 patients in the states that did not.
The percentage of patients receiving CSFs in the 6 months after starting chemotherapy fell in states that implemented the decision support tool (from 48.4% to 35.6%) but remained stable in states that did not (43.2% and 44.4%), Dr. Agiro reported. The adjusted difference in differences was –8.7% (P less than .001).
Meanwhile, the percentage of patients admitted for febrile neutropenia or experiencing this outcome while hospitalized increased in both states implementing the tool (from 2.8% to 4.3%) and those not implementing it (from 3.1% to 5.1%). Although the magnitude of increase was smaller in the former (+1.5% vs. +2.0%), the difference was not significant. Findings were essentially the same among the subset of patients aged 65 years and older.
“It’s important to study both intended and unintended consequences of such interventions,” Dr. Agiro noted. “Our study goes beyond financial considerations by looking at unintended outcomes: in this case, focusing on the incidence of febrile neutropenia, an outcome that is of prime interest to patients and oncologists and payers alike.”
The study may have missed some cases of febrile neutropenia, he acknowledged. “Also, there are other important outcomes of concern. For example, were there any delays in chemotherapy administration or immune recovery that could have been triggered by the implementation of the decision support program?”
The impact, both intended and unintended, on practices warrants evaluation as well, he further noted. “An important question could be, ‘Does it take less time to use this decision support tool compared to the time taken with normal care processes?’ ”
Dr. Agiro disclosed that he is employed by, has stock or other ownership interests in, and receives research funding from Anthem.
AT THE QUALITY CARE SYMPOSIUM
Key clinical point:
Major finding: The percentage of patients receiving CSFs fell in states that used the tool, versus those that did not (difference in differences, –8.7%), but changes in admissions for febrile neutropenia did not differ significantly.
Data source: A retrospective cohort study of 3,467 patients from 48 states starting chemotherapy for lung cancer.
Disclosures: Dr. Agiro disclosed that he is employed by, has stock or other ownership interests in, and receives research funding from Anthem. The study was funded by Anthem.
Lung cancer pathways reduce cost of care without compromising outcomes
ORLANDO – Implementation of clinical pathways aimed at improving appropriate, evidence-based care for patients with metastatic non–small-cell lung cancer (NSCLC) reduces costs without negatively affecting survival, the Dana-Farber Cancer Institute’s experience suggests.
“At Dana-Farber ... we have looked toward pathways as a potential tool to help manage complexity and resource utilization,” senior author David M. Jackman, MD, explained at a symposium on quality care sponsored by the American Society of Clinical Oncology. “We see pathways as a patient-centered platform that provides real-time decision-making support across the continuum of cancer care. We think that these should be based on preemptive decision making, reflect current standards of care, incorporate feedback from which we can learn from our practice patterns, and support clinical research.”
After the customized Dana-Farber Lung Pathways were implemented in 2014, the cost of outpatient care per patient in the first year after diagnosis fell by about $17,000, or 25%, primarily driven by reduced use of antineoplastic agents, according to data reported at the symposium and simultaneously published (J Oncol Pract. 2017 Mar 4. doi: 10.1200/JOP.2017.021741). Meanwhile, median survival remained at about 11 months, even trending slightly upward.
“Frankly, I’d like to think that we were delivering reasonable and expert care prior to 2014, so I did not anticipate that we were going to see a major change in terms of improvement in survival. But it is important for us to make sure that as we implemented Pathways, there was certainly no decrease in such care,”said Dr. Jackman, medical director of Clinical Pathways at Dana-Farber and an assistant professor of medicine, Harvard Medical School, Boston.
He and his colleagues plan to expand Pathways to cover the full spectrum of cancer care at their center, encompassing medical, radiation, and surgical oncology, he said.
“We also think that pathways can have a major impact on things like symptom management and survivorship care,” he added. “And as we work to embed all of our trials within our Pathways system, and as we push to have our trials in our satellites and in our network affiliates, we hope that this combination of activity can help move us from being not just a good care network, but also a research network.”
The pathways will still have to address some of the thornier issues related to the value of care, Dr. Jackman acknowledged “It’s incredibly easy for us to look at two equivalent therapies in terms of toxicity and efficacy and pick the cheaper one. The harder conversations are to come, that is, what if something is x dollars more expensive and only improves things by a small number of months, is it really worth it?
“Finally, we hope that pathways can be an area for innovation, not used solely to manage costs and to make decisions based on yesteryear, but also to help us move forward and to be the watering hole where everybody comes, as we build out our system that is looking granularly at genomics in order to help match patients with trial opportunities, and for researchers, to help them find specific patients for their trials,” he said. “Pathways can potentially be the nexus where everyone comes and where doctors are informed in real time about opportunities for their patients.”
More evidence of benefit
The Dana-Farber study adds to others showing that the benefits of pathways are real and reproducible, according to invited discussant Thomas J. Smith, MD, professor of oncology and palliative medicine at Johns Hopkins Medicine in Baltimore.
“More importantly, I think, for patients, who are getting hit with these bills and might have a 20% copay, it’s going to reduce their copays and for all the right reasons,” Dr. Smith concluded.
Pathways development
In developing the pathways, Dana-Farber began with lung cancer in part because the center sees a high volume of patients with the disease. In addition, decision making for this malignancy is complex, and there was considerable variation in oncologists’ practices.
“Our platform exists as an independent web-based system that currently lives outside of our EMR. Physicians can access this in real time, in the clinic room with the patient if they so choose,” Dr. Jackman explained. “From our EMR, we are flagged every time a provider orders a new start [of therapy], whether it’s IV chemo, oral chemo, or hormonal therapy. From our vendor, we receive granular treatment decision information made within the pathways system – information about the provider and site, information about the patients, their disease, and the line of therapy, as well as other important factors that drive decision making. Finally, from our clinical trials system interface, we can confirm trial enrollment data.”
Oncologists are free to leave the suggested pathway if their clinical judgment favors an alternate course, according to Dr. Jackman.
“We always want our physicians to feel comfortable treating the patients in front of them however they see best fit. If that means an off-pathway therapy, we want them to have the freedom to do that,” he said. “But we think one of the major tools of the pathways is to help capture the reasons why. So if they think it’s warranted and appropriate, go ahead, go off pathway, but tell us why you are doing it so we can learn from it.”
Using Pathways has not proved burdensome, according to Dr. Jackman. Navigating through the system requires about a minute or two, and use is required only when a patient is starting a new therapy, which typically occurs less than once per half-day clinic session.
Study details
In the study, he and colleagues compared costs of care in the first year after diagnosis of stage IV NSCLC between 160 patients treated at Dana-Farber in 2012 (before Pathways implementation) and 210 patients treated there in 2014 (after Pathways implementation).
“It should be noted that because we are a free-standing outpatient cancer center, all of the costs that we were able to gather are intramural and therefore related only to outpatient activities,” he pointed out.
The total annual costs of care per patient, adjusted for potential confounders (age, sex, race, distance to the institute, clinical trial enrollment, and EGFR and ALK status) fell by $17,085 after implementation of Pathways, from $69,122 to $52,037 (P = .01), he reported.
The largest source of cost savings by far, accounting for 73% of the total, was reduced use of antineoplastic agents (chemotherapy, biologics, and other anticancer agents). Cost for this component fell from $44,237 per patient to $31,846 (P less than .01).
“The majority of this savings came through a reduction in the use of what we considered unwarranted use of combination chemotherapy,” Dr. Jackman said. “In the first-line setting, we specifically went after the regimen of carboplatin, pemetrexed, and bevacizumab; based on our interpretation of the PointBreak study, we felt that that regimen did not bring additional efficacy but did essentially double drug costs. In going after that, we reduced not only use of that but also the subsequent use of pemetrexed plus bevacizumab maintenance. In the second-line setting, with the implementation of Pathways, we saw a decrease in the use of inappropriate platinum-based doublet therapy in those patients who had previously progressed on a platinum-based doublet.”
Median overall survival did not decrease and in fact increased slightly, from 10.7 months before Pathways implementation to 11.2 months afterward (P = .08). Corresponding 1-year rates of survival were 52% and 64%.
“We stand on the shoulders of those who came before us, who have also shown savings associated with implementation of pathways,” concluded Dr. Jackman. “But we hope that we add our voice and our data to this argument that pathways, I think, are a reasonable tool as we try to manage complexity and resource utilization. In addition, we do so without impinging upon clinical outcomes.”
The study was limited by its inclusion of only outpatient costs at Dana-Farber, he acknowledged. “You and we would be very interested in being able to know whether our Pathways implementation affected ED [emergency department] visits or hospitalizations. To that end, we are working with some of our regional payers to try to transparently share data around outcomes, costs, and usage, so that we can learn more in this regard.”
Dr. Jackman disclosed that he is an adviser or consultant to Bayer, Celgene, CVS Caremark, Genentech, and Lilly.
ORLANDO – Implementation of clinical pathways aimed at improving appropriate, evidence-based care for patients with metastatic non–small-cell lung cancer (NSCLC) reduces costs without negatively affecting survival, the Dana-Farber Cancer Institute’s experience suggests.
“At Dana-Farber ... we have looked toward pathways as a potential tool to help manage complexity and resource utilization,” senior author David M. Jackman, MD, explained at a symposium on quality care sponsored by the American Society of Clinical Oncology. “We see pathways as a patient-centered platform that provides real-time decision-making support across the continuum of cancer care. We think that these should be based on preemptive decision making, reflect current standards of care, incorporate feedback from which we can learn from our practice patterns, and support clinical research.”
After the customized Dana-Farber Lung Pathways were implemented in 2014, the cost of outpatient care per patient in the first year after diagnosis fell by about $17,000, or 25%, primarily driven by reduced use of antineoplastic agents, according to data reported at the symposium and simultaneously published (J Oncol Pract. 2017 Mar 4. doi: 10.1200/JOP.2017.021741). Meanwhile, median survival remained at about 11 months, even trending slightly upward.
“Frankly, I’d like to think that we were delivering reasonable and expert care prior to 2014, so I did not anticipate that we were going to see a major change in terms of improvement in survival. But it is important for us to make sure that as we implemented Pathways, there was certainly no decrease in such care,”said Dr. Jackman, medical director of Clinical Pathways at Dana-Farber and an assistant professor of medicine, Harvard Medical School, Boston.
He and his colleagues plan to expand Pathways to cover the full spectrum of cancer care at their center, encompassing medical, radiation, and surgical oncology, he said.
“We also think that pathways can have a major impact on things like symptom management and survivorship care,” he added. “And as we work to embed all of our trials within our Pathways system, and as we push to have our trials in our satellites and in our network affiliates, we hope that this combination of activity can help move us from being not just a good care network, but also a research network.”
The pathways will still have to address some of the thornier issues related to the value of care, Dr. Jackman acknowledged “It’s incredibly easy for us to look at two equivalent therapies in terms of toxicity and efficacy and pick the cheaper one. The harder conversations are to come, that is, what if something is x dollars more expensive and only improves things by a small number of months, is it really worth it?
“Finally, we hope that pathways can be an area for innovation, not used solely to manage costs and to make decisions based on yesteryear, but also to help us move forward and to be the watering hole where everybody comes, as we build out our system that is looking granularly at genomics in order to help match patients with trial opportunities, and for researchers, to help them find specific patients for their trials,” he said. “Pathways can potentially be the nexus where everyone comes and where doctors are informed in real time about opportunities for their patients.”
More evidence of benefit
The Dana-Farber study adds to others showing that the benefits of pathways are real and reproducible, according to invited discussant Thomas J. Smith, MD, professor of oncology and palliative medicine at Johns Hopkins Medicine in Baltimore.
“More importantly, I think, for patients, who are getting hit with these bills and might have a 20% copay, it’s going to reduce their copays and for all the right reasons,” Dr. Smith concluded.
Pathways development
In developing the pathways, Dana-Farber began with lung cancer in part because the center sees a high volume of patients with the disease. In addition, decision making for this malignancy is complex, and there was considerable variation in oncologists’ practices.
“Our platform exists as an independent web-based system that currently lives outside of our EMR. Physicians can access this in real time, in the clinic room with the patient if they so choose,” Dr. Jackman explained. “From our EMR, we are flagged every time a provider orders a new start [of therapy], whether it’s IV chemo, oral chemo, or hormonal therapy. From our vendor, we receive granular treatment decision information made within the pathways system – information about the provider and site, information about the patients, their disease, and the line of therapy, as well as other important factors that drive decision making. Finally, from our clinical trials system interface, we can confirm trial enrollment data.”
Oncologists are free to leave the suggested pathway if their clinical judgment favors an alternate course, according to Dr. Jackman.
“We always want our physicians to feel comfortable treating the patients in front of them however they see best fit. If that means an off-pathway therapy, we want them to have the freedom to do that,” he said. “But we think one of the major tools of the pathways is to help capture the reasons why. So if they think it’s warranted and appropriate, go ahead, go off pathway, but tell us why you are doing it so we can learn from it.”
Using Pathways has not proved burdensome, according to Dr. Jackman. Navigating through the system requires about a minute or two, and use is required only when a patient is starting a new therapy, which typically occurs less than once per half-day clinic session.
Study details
In the study, he and colleagues compared costs of care in the first year after diagnosis of stage IV NSCLC between 160 patients treated at Dana-Farber in 2012 (before Pathways implementation) and 210 patients treated there in 2014 (after Pathways implementation).
“It should be noted that because we are a free-standing outpatient cancer center, all of the costs that we were able to gather are intramural and therefore related only to outpatient activities,” he pointed out.
The total annual costs of care per patient, adjusted for potential confounders (age, sex, race, distance to the institute, clinical trial enrollment, and EGFR and ALK status) fell by $17,085 after implementation of Pathways, from $69,122 to $52,037 (P = .01), he reported.
The largest source of cost savings by far, accounting for 73% of the total, was reduced use of antineoplastic agents (chemotherapy, biologics, and other anticancer agents). Cost for this component fell from $44,237 per patient to $31,846 (P less than .01).
“The majority of this savings came through a reduction in the use of what we considered unwarranted use of combination chemotherapy,” Dr. Jackman said. “In the first-line setting, we specifically went after the regimen of carboplatin, pemetrexed, and bevacizumab; based on our interpretation of the PointBreak study, we felt that that regimen did not bring additional efficacy but did essentially double drug costs. In going after that, we reduced not only use of that but also the subsequent use of pemetrexed plus bevacizumab maintenance. In the second-line setting, with the implementation of Pathways, we saw a decrease in the use of inappropriate platinum-based doublet therapy in those patients who had previously progressed on a platinum-based doublet.”
Median overall survival did not decrease and in fact increased slightly, from 10.7 months before Pathways implementation to 11.2 months afterward (P = .08). Corresponding 1-year rates of survival were 52% and 64%.
“We stand on the shoulders of those who came before us, who have also shown savings associated with implementation of pathways,” concluded Dr. Jackman. “But we hope that we add our voice and our data to this argument that pathways, I think, are a reasonable tool as we try to manage complexity and resource utilization. In addition, we do so without impinging upon clinical outcomes.”
The study was limited by its inclusion of only outpatient costs at Dana-Farber, he acknowledged. “You and we would be very interested in being able to know whether our Pathways implementation affected ED [emergency department] visits or hospitalizations. To that end, we are working with some of our regional payers to try to transparently share data around outcomes, costs, and usage, so that we can learn more in this regard.”
Dr. Jackman disclosed that he is an adviser or consultant to Bayer, Celgene, CVS Caremark, Genentech, and Lilly.
ORLANDO – Implementation of clinical pathways aimed at improving appropriate, evidence-based care for patients with metastatic non–small-cell lung cancer (NSCLC) reduces costs without negatively affecting survival, the Dana-Farber Cancer Institute’s experience suggests.
“At Dana-Farber ... we have looked toward pathways as a potential tool to help manage complexity and resource utilization,” senior author David M. Jackman, MD, explained at a symposium on quality care sponsored by the American Society of Clinical Oncology. “We see pathways as a patient-centered platform that provides real-time decision-making support across the continuum of cancer care. We think that these should be based on preemptive decision making, reflect current standards of care, incorporate feedback from which we can learn from our practice patterns, and support clinical research.”
After the customized Dana-Farber Lung Pathways were implemented in 2014, the cost of outpatient care per patient in the first year after diagnosis fell by about $17,000, or 25%, primarily driven by reduced use of antineoplastic agents, according to data reported at the symposium and simultaneously published (J Oncol Pract. 2017 Mar 4. doi: 10.1200/JOP.2017.021741). Meanwhile, median survival remained at about 11 months, even trending slightly upward.
“Frankly, I’d like to think that we were delivering reasonable and expert care prior to 2014, so I did not anticipate that we were going to see a major change in terms of improvement in survival. But it is important for us to make sure that as we implemented Pathways, there was certainly no decrease in such care,”said Dr. Jackman, medical director of Clinical Pathways at Dana-Farber and an assistant professor of medicine, Harvard Medical School, Boston.
He and his colleagues plan to expand Pathways to cover the full spectrum of cancer care at their center, encompassing medical, radiation, and surgical oncology, he said.
“We also think that pathways can have a major impact on things like symptom management and survivorship care,” he added. “And as we work to embed all of our trials within our Pathways system, and as we push to have our trials in our satellites and in our network affiliates, we hope that this combination of activity can help move us from being not just a good care network, but also a research network.”
The pathways will still have to address some of the thornier issues related to the value of care, Dr. Jackman acknowledged “It’s incredibly easy for us to look at two equivalent therapies in terms of toxicity and efficacy and pick the cheaper one. The harder conversations are to come, that is, what if something is x dollars more expensive and only improves things by a small number of months, is it really worth it?
“Finally, we hope that pathways can be an area for innovation, not used solely to manage costs and to make decisions based on yesteryear, but also to help us move forward and to be the watering hole where everybody comes, as we build out our system that is looking granularly at genomics in order to help match patients with trial opportunities, and for researchers, to help them find specific patients for their trials,” he said. “Pathways can potentially be the nexus where everyone comes and where doctors are informed in real time about opportunities for their patients.”
More evidence of benefit
The Dana-Farber study adds to others showing that the benefits of pathways are real and reproducible, according to invited discussant Thomas J. Smith, MD, professor of oncology and palliative medicine at Johns Hopkins Medicine in Baltimore.
“More importantly, I think, for patients, who are getting hit with these bills and might have a 20% copay, it’s going to reduce their copays and for all the right reasons,” Dr. Smith concluded.
Pathways development
In developing the pathways, Dana-Farber began with lung cancer in part because the center sees a high volume of patients with the disease. In addition, decision making for this malignancy is complex, and there was considerable variation in oncologists’ practices.
“Our platform exists as an independent web-based system that currently lives outside of our EMR. Physicians can access this in real time, in the clinic room with the patient if they so choose,” Dr. Jackman explained. “From our EMR, we are flagged every time a provider orders a new start [of therapy], whether it’s IV chemo, oral chemo, or hormonal therapy. From our vendor, we receive granular treatment decision information made within the pathways system – information about the provider and site, information about the patients, their disease, and the line of therapy, as well as other important factors that drive decision making. Finally, from our clinical trials system interface, we can confirm trial enrollment data.”
Oncologists are free to leave the suggested pathway if their clinical judgment favors an alternate course, according to Dr. Jackman.
“We always want our physicians to feel comfortable treating the patients in front of them however they see best fit. If that means an off-pathway therapy, we want them to have the freedom to do that,” he said. “But we think one of the major tools of the pathways is to help capture the reasons why. So if they think it’s warranted and appropriate, go ahead, go off pathway, but tell us why you are doing it so we can learn from it.”
Using Pathways has not proved burdensome, according to Dr. Jackman. Navigating through the system requires about a minute or two, and use is required only when a patient is starting a new therapy, which typically occurs less than once per half-day clinic session.
Study details
In the study, he and colleagues compared costs of care in the first year after diagnosis of stage IV NSCLC between 160 patients treated at Dana-Farber in 2012 (before Pathways implementation) and 210 patients treated there in 2014 (after Pathways implementation).
“It should be noted that because we are a free-standing outpatient cancer center, all of the costs that we were able to gather are intramural and therefore related only to outpatient activities,” he pointed out.
The total annual costs of care per patient, adjusted for potential confounders (age, sex, race, distance to the institute, clinical trial enrollment, and EGFR and ALK status) fell by $17,085 after implementation of Pathways, from $69,122 to $52,037 (P = .01), he reported.
The largest source of cost savings by far, accounting for 73% of the total, was reduced use of antineoplastic agents (chemotherapy, biologics, and other anticancer agents). Cost for this component fell from $44,237 per patient to $31,846 (P less than .01).
“The majority of this savings came through a reduction in the use of what we considered unwarranted use of combination chemotherapy,” Dr. Jackman said. “In the first-line setting, we specifically went after the regimen of carboplatin, pemetrexed, and bevacizumab; based on our interpretation of the PointBreak study, we felt that that regimen did not bring additional efficacy but did essentially double drug costs. In going after that, we reduced not only use of that but also the subsequent use of pemetrexed plus bevacizumab maintenance. In the second-line setting, with the implementation of Pathways, we saw a decrease in the use of inappropriate platinum-based doublet therapy in those patients who had previously progressed on a platinum-based doublet.”
Median overall survival did not decrease and in fact increased slightly, from 10.7 months before Pathways implementation to 11.2 months afterward (P = .08). Corresponding 1-year rates of survival were 52% and 64%.
“We stand on the shoulders of those who came before us, who have also shown savings associated with implementation of pathways,” concluded Dr. Jackman. “But we hope that we add our voice and our data to this argument that pathways, I think, are a reasonable tool as we try to manage complexity and resource utilization. In addition, we do so without impinging upon clinical outcomes.”
The study was limited by its inclusion of only outpatient costs at Dana-Farber, he acknowledged. “You and we would be very interested in being able to know whether our Pathways implementation affected ED [emergency department] visits or hospitalizations. To that end, we are working with some of our regional payers to try to transparently share data around outcomes, costs, and usage, so that we can learn more in this regard.”
Dr. Jackman disclosed that he is an adviser or consultant to Bayer, Celgene, CVS Caremark, Genentech, and Lilly.
AT THE QUALITY CARE SYMPOSIUM
Key clinical point:
Major finding: The annual cost of outpatient care per patient fell by $17,085, mainly because of reduced use of antineoplastic agents, whereas median survival remained at about 11 months.
Data source: A cohort study among patients with newly diagnosed metastatic NSCLC, comparing 160 treated before and 210 treated after pathways implementation.
Disclosures: Dr. Jackman disclosed that he is an adviser or consultant to Bayer, Celgene, CVS Caremark, Genentech, and Lilly.